- *Corresponding Author:
- Yan Mei
Affiliated Hospital of Tianjin Academy of Traditional Chinese Medicine, Tianjin 300120, China
E-mail: nuodun@163.com
| This article was originally published in a special issue, “Drug Discovery and Repositioning Studies in Biopharmaceutical Sciences” |
| Indian J Pharm Sci 2024:86(4) Spl Issue “814-825” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
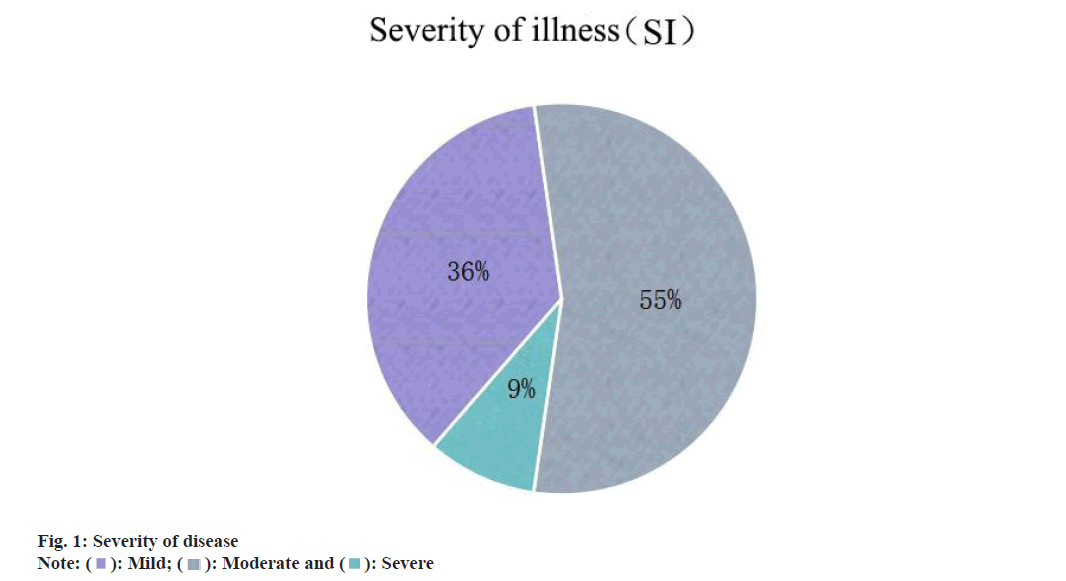
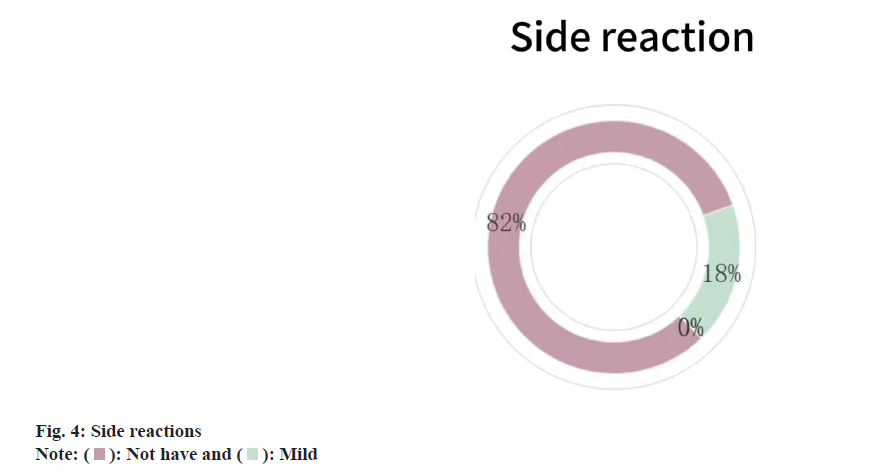
To observe and explore the clinical effect of Chinese acupuncture and electro acupuncture in the treatment of somatic symptoms and to analyze the mechanism of action. 77 patients with psychosomatic symptoms who were treated from July 2022 to July 2023 in Affiliated Hospital of Tianjin University of Chinese Medicine from July 2023 were divided into 38 patients in acupuncture treatment group (acupuncture combined with electroacupuncture therapy and with or without drugs) and 39 patients in non-acupuncture treatment group (other conventional treatment group that had not received acupuncture). Compare the symptom check list 90, cornell medical index and WCPA somatic symptoms rating scale, clinical global impression scales before and after 4 w of treatment. None of the four scales was statistically significant before treatment (p>0.05), and comparison of symptom self-rating scale (symptom check list 90) (p<0.05). Comparison of cornell medical index table; within and between groups (p<0.05). Comparison of clinical somatic symptoms classification scale (WCPA) of Western psychiatric association; there was no significant difference between groups before and after (p>0.05), and the scores of WCPA scale A, C and D dimensions were significantly lower than that of non-acupuncture group, p<0.05, and the differences of B and E dimensions were not significant p>0.05. The overall clinical efficacy scale acupuncture treatment group was mostly mild and moderate (55 % and 36 %), acupuncture had no significant side effects (82 %), efficacy index was significant (p>1.0 points), response rate reached 81.82 %, and global improvement was significant improvement (46 %). After systematically evaluating the somatic symptoms and clinical efficacy of patients, it is sufficient evidence to provide more scientific and effective treatment plans for patients with psychosomatic symptom disorders, and to provide more accurate diagnosis and treatment methods for clinicians.
Keywords
Acupuncture, psychosomatic medicine, stress, anxiety, depression
Many people in today are more or less troubled by physical symptoms that may result from multiple factors such as psychological stress, mood disorders or lifestyle habits. In the clinical complex condition of many patients, most medical staff often focus on the diagnosis, treatment plan and post-disease care of the disease, while ignoring the reason why the patients actually come to see the doctor[1]. The diagnosis and treatment mostly focus on the diseases caused by physical symptoms. Although it can control some clinical symptoms, the psychosocial problems will soon relapse after not being fundamentally solved, and then delay or repeat and eventually turn into refractory or severe diseases. Therefore, the study of the diagnosis and treatment of somatic symptoms under the psychosomatic medicine theory is of great significance. The field of modern psychosomatic medicine focuses more on the interaction between biological psychological factors, physical health and social function. Year by year, researchers have formed a complete set of bio-psychological-social three-dimensional model theory, which eventually develops into the mode of psychological-body-social intersection under the continuous experimental research of diseases[2]. In the past few decades, many researchers have had their own unique insights and theoretical achievements in acupuncture for the treatment of mood disorders (anxiety, depression, compulsion, etc.) sleep disorders and psychiatric diseases[3]. Although the research results involve somatic symptoms and have certain efficacy on the relief of clinical symptoms, there are still few observations and studies on somatic symptoms from the perspective of psychosomatic medicine. Some reports show that the traditional medical intervention method, the main acupoint matching method of acupuncture, have an obvious effect on the treatment of mood disorders and SD in psychosomatic medicine[3]. Based on this, the holistic therapy of traditional medicine acupuncture combined with electroacupuncture used in this study emerged at the historic moment and has its progressive development. It can not only improve the physical symptoms of patients, but also greatly improve the overall mental state and quality of life, which is reported as follows.
Materials and Methods
Source of case data:
Seventy-seven patients with somatic symptoms who were treated in the outpatient department from July 2022 to the Department of the Affiliated Hospital of Tianjin University of Traditional Chinese Medicine (TCM) from July 2022 were divided into acupuncture treatment group and non-acupuncture treatment group by random number chart. Age was 18 y-65 y, and the general data were not significantly different (p>0.05), which was comparable.
Diagnostic criteria: Psychosomatic symptoms and disorder: Li et al.[4]. Symptoms criteria include at least one of the following; depression, anxiety, insomnia, pain and other somatization symptoms.
Serious criteria: Social functions are partially impaired or self-painful, prompting them to seek medical treatment.
Disease course criteria: More than 1 w. All parts of the body discomfort or pain, including difficulty falling asleep, dream, easy to wake up, frequent urination, nausea, vomiting, diarrhea, constipation, stomach distension, chest tightness, palpitations, dry mouth, tremor, headache, muscle pain, joint pain, skin itching symptoms in any one or more continuous or regular.
Inclusion criteria: Meet the above diagnostic criteria, the chief complaint meets and complete the evaluation of Symptom Check List 90 (SCL- 90), Cornell Medical Index (CMI), WCPA somatic symptoms rating scale (WCPA), Clinical Global Impression (CGI) scales; 18 y-65 y old (including 18 y and 65 y old), whether male or female; those who have taken or not taken psychotropic drugs before or during acupuncture treatment but the symptoms are not obvious; the clinical data of the patient is complete and has a high degree of cooperation, and has the normal communication and communication skills. Normal intelligence, with autonomy to complete the assessment of the scale; no history of serious physical diseases or brain organic diseases; the patient and his/her family members gave the informed consent for the study and voluntarily signed the informed consent form.
Exclusion criteria: Combined with other serious underlying diseases or in the acute period/fluctuation period of the disease; severe somatic symptoms caused by other causes such as primary somatic diseases; various mental and cognitive disorders; having a history of mental illness, such as drug abuse and alcohol dependence; pregnant women, coagulation dysfunction, skin infection, ulcers and other cannot bear acupuncture treatment, dizzy acupuncture, etc.; eliminate those who are not serious and complete answers, and are not willing to participate in the scale evaluation.
Elimination criteria: Cases with irregular and incomplete scale; patients with serious adverse reactions or sudden other diseases during acupuncture treatment who are not suitable for further study and patients ordered by the investigator (such as poor compliance, not receiving medical advice, etc.). Patients who lost contact by default or family members failed to continue to acupuncture for 4 w.
Study methods:
Grouping of cases: It was divided into acupuncture treatment group and non-acupuncture treatment group. The acupuncture treatment group used acupuncture (Hua Tuo brand 0.3×40 mm 10 pcs) combined with Baihui and Yintang acupuncture for 30 min each; the non-acupuncture treatment group was other conventional treatment group that had not received acupuncture. There were 40 patients in each group, 38 in the final acupuncture group, 39 in the non-acupuncture group, 3 shedding (two patients lost contact midway, one did not reach the time of acupuncture treatment for 4 w), a total of 77 patients.
Treatment methods: The acupuncture treatment group received acupuncture treatment according to the main point matching method and the main point was selected; Baihui, Yintang and Hetgu (double); the allotment points are categorized according to the WCPA[5] as follows; biological symptoms choose Zusanli (double) and Sanyinjiao (double). Cognitive symptoms of selected heart shu, liver shu, and kidney shu (double). Imaginary symptoms choose Sishencong, Lingtai, Shenting, Shenmen (double). Suppression symptoms choose Zusanli (double), Sanyinjiao (double), Neiguan (double), Anmian (double), Danzhong, Qimen. Provocative symptoms Dazhui, Zusanli (double), Sanyinjiao (double), Neiguan (double), Taichong (double), Taiyang (double); electric needle (Baihui and Yintang point), the treatment time is 30 min. The non-acupuncture treatment group only received conventional drugs other than acupuncture.
Research methodology: In this study, the main indicators such as somatic symptoms before and after treatment analysis understand the development trend of clinical psychosomatic symptoms, combined with the clinical data of the subjects, specifically for subjects with the presence of somatic symptoms using the scale assessment, independent according to the instruction prompt in turn. Subject by the researcher himself, using the way of field questionnaire, the experiment has five questionnaires, test subjects according to the instruction first fill in personal information, clear answer after answer; subjects fully fill in general data, SCL-90, CMI, WCPA, insight into the curative effect of the disease treatment advantage and related knowledge. During the course of the study, the patient’s somatic symptoms were first assessed, with the employed symptom assessment tools including SCL-90, CMI and WCPA. These scales were chosen based on their wide application and reliable reliability and validity. Through the evaluation of the scale, the somatic symptoms and the degree of damage to psychosomatic health were determined. 80 patients were selected from the inclusion and exclusion criteria. After randomization, the condition was evaluated before and after treatment to compare the changes before and after treatment in the two groups. Based on the efficacy of the acupuncture group, the random sampling method was adopted, and 11 patients were randomly selected for CGI test to improve and analyze the treatment effect. Time of first test was the day of the first subject and second test time was 4 w after the first subject.
Efficacy determination criteria:
General indicators: Gender, age, time of onset, course of disease can be obtained through the general data sheet (self-compiled); the somatization, compulsion, depression, anxiety, paranoia, and other indicators in SCL-90 were reduced according to the score of SCL-90 after diagnosis and the total score and any factor (total score>160 or >positive items>43 or any factor>2), if the total score of the number of positive items or any factor is reduced, higher or flat score is invalid; the total score, eyes, ears, respiratory, cardiovascular, digestive, urinary, muscle, skin system and other indicators in CMI were based on the evaluation score of the first diagnosis, the total score after treatment and the score of each factor (the total score of men was 35 MR was 15; female total score 40 MR total score 20) lower than the significant effect, any reduction of the total score or MR or any factor score is effective, elevated or flat score is invalid; the four and total items of ABCD in WCPA were compared the data of each item and total score of ABCDE after the first diagnosis and treatment, both are reduced and effective. The total score and the reduced score of any item is effective, increased or equal is invalid; in the severity of CGI 0-7 (0 means no disease and 7 means extreme heavy), the total evaluation of 0-7 (0 represents no evaluation and 7 represents serious deterioration), the efficacy index of the efficacy and side reaction coding table (4-0.25), the higher the index, the better the clinical efficacy.
Statistical methods:
The database was established using Excel software, data statistical analysis using Statistical Package for the Social Sciences (SPSS) 26.0, measurement data in presentation, Wilcoxon signed rank sum test, and count data in percent (%), Chi-square (χ2) (x̄ ±s) tested, and used statistical methods to compare the differences between the two groups.
Results and Discussion
The mean age of the patients was (53±12.63) y, and the mean total disease duration was (43.08±82.05) mo. The differences in patient age, age at first onset, and disease course were insignificant, p>0.05 as shown in Table 1. Patient degree, disease reason and marital status were not significant, p>0.05 as shown in Table 2-Table 4.
| Project | Group | n | Mean | Z | p |
|---|---|---|---|---|---|
| Age | Needle thorn | 38 | 51.97±12.72 | -1.413 | 0.158 |
| Non-acupuncture | 39 | 48.67±12.5 | |||
| Age at first onset | Needle thorn | 38 | 46.89±14.29 | -1.488 | 0.137 |
| Non-acupuncture | 39 | 41.92±14.47 | |||
| Course of disease | Needle thorn | 38 | 52.84±85.7 | -1.617 | 0.106 |
| Non-acupuncture | 39 | 33.56±78.26 |
Table 1: Mean Values of Age and Disease Duration
| Degree of education | Primary school and below | Junior middle school | Senior middle school | University and above |
|---|---|---|---|---|
| Needle thorn group | 1 | 16 | 11 | 10 |
| Non-acupuncture group | 3 | 15 | 9 | 12 |
| χ2 | 1.448 | |||
| p | 0.694 | |||
Table 2: Distribution of Patients
| Onset of season | Spring | Summer | Autumn | Winter |
|---|---|---|---|---|
| Needle thorn group | 5 | 7 | 16 | 10 |
| Non-acupuncture group | 7 | 8 | 15 | 9 |
| χ2 | 0.472 | |||
| p | 0.925 | |||
Table 3: Seasonal Distribution of Patients
| Marriage | Married | Unmarried | Dissociation | Bereft of one's spouse |
|---|---|---|---|---|
| Needle thorn group | 22 | 8 | 5 | 3 |
| Non-acupuncture group | 26 | 7 | 3 | 3 |
| χ2 | 0.893 | |||
| p | 0.827 | |||
Table 4: Distribution of the Marital Status of the Patients
There were 13 men, 25 women, 13 men and 26 women in the non-acupuncture group (Table 5), with no significant difference in patient sex ratio, p>0.05. In conclusion, the difference in general patient data comparison was not significant, with p>0.05.
| Project | Male | Female |
|---|---|---|
| Needle thorn group | 13 | 25 |
| Non-acupuncture group | 13 | 26 |
| χ2 | 0.007 | |
| p | 0.935 | |
Table 5: Sex Distribution
The total scores varied significantly before and after the intervention, p<0.05. In the non-acupuncture group, p>0.05 (Table 6). No difference in scores after the intervention, p>0.05 (Table 7).
| Scale | Pre-intervention | Post-intervention | Z | p | ||||
|---|---|---|---|---|---|---|---|---|
| Acupuncture group | Non-acupuncture group | Acupuncture group | Non-acupuncture group | Acupuncture group | Non-acupuncture group | Acupuncture group | Non-acupuncture group | |
| SCL-90 | 190.92±59.45 | 186.59±67.11 | 171.32±59.33 | 170.33±64.27 | -2.016 | -1.369 | 0.044 | 0.171 |
| CMI | 48.05±15.88 | 49.87±16.92 | 40.39±12.8 | 45.38±16.22 | -2.778 | -1.305 | 0.005 | 0.192 |
| WCPA | 51.21±8.52 | 52.31±7.98 | 46.76±7.77 | 50.21±7.99 | -2.835 | -1.461 | 0.005 | 0.144 |
Table 6: Comparison of the Scales before and after Intervention
| Scale | Pre-intervention | Post-intervention | Z | p |
|---|---|---|---|---|
| SCL-90 sub-dimension | ||||
| Somatization | 2.04±0.69 | 1.58±0.54 | -3.27 | 0 |
| Depressed | 2.51±0.88 | 2.08±0.79 | -2.44 | 0.02 |
| Anxious | 2.53±0.67 | 2.25±0.63 | -2.11 | 0.04 |
| PMI sub-dimensions | ||||
| Eye ear | 3.21±1.65 | 1.58±0.54 | -0.61 | 0.54 |
| Breathe | 3.03±1.9 | 2.08±0.79 | -0.77 | 0.44 |
| Cardiovascular | 4.34±2.44 | 2.25±0.63 | -1.83 | 0.06 |
| Digestion | 5.39±3.27 | 2.71±1.21 | -2.3 | 0.02 |
| Muscle | 2.34±1.7 | 2.66±1.23 | -1.09 | 0.28 |
| Skin | 2±1.71 | 3.63±1.85 | -2.25 | 0.02 |
| Nerve | 3.13±2.16 | 4.55±2.68 | -1.57 | 0.12 |
| Urination | 2.39±1.6 | 2.13±1.53 | -0.46 | 0.65 |
| M-R | 19.24±7.01 | 16.89±6.5 | -0.31 | 0.76 |
| WCPA sub-dimension | ||||
| A | 16.11±5.47 | 14.55±4.94 | -1.37 | 0.17 |
| B | 15.03±2.99 | 13.82±2.62 | -1.79 | 0.07 |
| C | 5.89±3.27 | 5.82±3.23 | -0.07 | 0.95 |
| D | 7.05±3.1 | 6.32±2.83 | -1.19 | 0.23 |
| E | 7.13±2.66 | 6.26±2.52 | -1.39 | 0.16 |
Table 7: Comparison of Scl, Pmi and Wcpa Sub-Dimension Scores before and after Acupuncture Intervention
The scores of SCL-90 sub-dimensions varied significantly before and after intervention, with anxiety, depression and somatization factors; p<0.05. No difference in muscle and urinary dimensions, p>0.05 and other sub-dimensions, such as eye, ear, respiratory, cardiovascular, digestion and skin, p<0.05. The differences in the WCPA scores for each sub-dimensions were not significant, p>0.05 (Table 8).
| Scale | Needle thorn group | Non-acupuncture group | Z | p |
|---|---|---|---|---|
| SCL-90 | 171.32±59.33 | 170.33±64.27 | -0.484 | 0.628 |
| CMI | 40.39±12.8 | 45.38±16.22 | -1.382 | 0.167 |
| WCPA | 46.76±7.77 | 50.21±7.99 | -1.913 | 0.056 |
Table 8: Comparison of Total Scores of Each Scale after the Intervention
Only somatization scores on the SCL-90 scale in the non-acupuncture group, p<0.05. Other subdimensions were not significant, p>0.05. The differences in eyes, ear, respiration, muscle, urinary and cardiovascular dimensions were not significant, p>0.05, only two sub-dimensions, skin and digestion, p<0.05. WCPA the differences in the scores were not significant, p>0.05 (Table 9).
| Scale | Pre-intervention | Post-intervention | Z | p |
|---|---|---|---|---|
| SCL-90 sub-dimension | ||||
| Somatization | 2.26±0.61 | 2.01±0.59 | -2.045 | 0.041 |
| Depressed | 2.47±0.83 | 2.33±0.78 | -0.74 | 0.459 |
| Anxious | 2.55±0.78 | 2.36±0.71 | -1.155 | 0.248 |
| PMI sub-dimensions | ||||
| Eye ear | 3.38±1.96 | 3.03±178 | 0.847a | 0.4 |
| Breathe | 2.59±1.68 | 2.36±1.48 | 0.644a | 0.522 |
| Cardiovascular | 5.00±1.74 | 4.69±2.61 | 0.508a | 0.613 |
| Digestion | 6.18±2.69 | 5.92±2.64 | 3.935 | 0 |
| Muscle | 1.92±1.35 | 1.74±1.35 | -0.962 | 0.336 |
| Skin | 1.26±1.29 | 1.08±1.22 | -3.627 | 0 |
| Nerve | 2.41±1.70 | 2.13±1.52 | -2.56 | 0.01 |
| Urination | 2.21±1.4 | 1.97±1.33 | -0.716 | 0.474 |
| M -R | 18.95±7.25 | 16.69±6.68 | -1.816 | 0.069 |
| WCPA sub-dimension | ||||
| A | 18.28±5.57 | 17.26±5.38 | -0.941 | 0.346 |
| B | 14.03±3.61 | 13.54±3.52 | -0.811 | 0.417 |
| C | 3.18±2.1 | 3.15±2.01 | -0.005 | 0.996 |
| D | 10.59±4.04 | 10.23±4.08 | -0.377 | 0.706 |
| E | 6.23±1.72 | 6.03±1.75 | -0.449 | 0.653 |
Table 9: Comparison of Scl, Pmi, Wcpa Sub-Dimension Scores before and after Intervention in the Non-Acupuncture Group
The post-intervention acupuncture group SCL-90 scale was significantly lower than that of the nonacupuncture group, with p<0.05. The digestion and skin dimension scores of the acupuncture group were significantly lower than those of the non-acupuncture group, with significant differences, p<0.05. The WCPA scales A, C and D were significantly lower than the non-acupuncture group, with p<0.05 (Table 10). No difference in the other sub-dimensions in each scale were significant, with p>0.05.
| Scale | Acupuncture group | Non-acupuncture group | Z | p |
|---|---|---|---|---|
| SCL-90 Sub-dimension | ||||
| Somatization | 1.58±0.54 | 2.01±0.59 | -3.445 | 0.001 |
| Depressed | 2.08±0.79 | 2.33±0.78 | -1.758 | 0.079 |
| Anxious | 2.25±0.63 | 2.36±0.71 | -0.591 | 0.554 |
| CMC sub-dimensions | ||||
| Eye ear | 1.58±0.54 | 3.03±178 | -0.609 | 0.542 |
| Breathe | 2.08±0.79 | 2.36±1.48 | -0.773 | 0.439 |
| Cardiovascular | 2.25±0.63 | 4.69±2.61 | -1.834 | 0.067 |
| Digestion | 2.71±1.21 | 5.92±2.64 | -2.302 | 0.021 |
| Muscle | 2.66±1.23 | 1.74±1.35 | -1.091 | 0.275 |
| Skin | 3.63±1.85 | 1.08±1.22 | -2.253 | 0.024 |
| Nerve | 4.55±2.68 | 2.13±1.52 | -1.571 | 0.116 |
| Urination | 2.13±1.53 | 1.97±1.33 | -0.456 | 0.649 |
| M -R | 16.89±6.5 | 16.69±6.68 | -0.307 | 0.759 |
| WCPA Sub-dimension | ||||
| A | 14.55±4.94 | 17.26±5.38 | -2.43 | 0.015 |
| B | 13.82±2.62 | 13.54±3.52 | -0.687 | 0.492 |
| C | 5.82 | 3.15±2.01 | -4.043 | 0 |
| D | 6.32±2.83 | 10.23±4.08 | -4.256 | 0 |
| E | 6.26±2.52 | 6.03±1.75 | -0.233 | 0.816 |
Table 10: Scl, Cmc, Wcpa Sub-Dimension Scores of the Two Groups after the Intervention
Most of the patients selected in the acupuncture treatment group had mild and moderate disease (SI) (fig. 1), the overall efficacy (GI) significantly improved (fig. 2), the Efficacy Index (EI) was >1.0, 5 had the highest 4.0 (fig. 3), no significant side effects (fig. 4), and the effective rate reached 81.82 % (Table 11).
| Project | Invalid/ deteriorated |
Valid | Excellence | A little effective | Effective percentage |
|---|---|---|---|---|---|
| Acupuncture group | 2 | 2 | 5 | 2 | 81.82 % |
| χ2 | 8.456 | ||||
| p | 0.037 | ||||
Table 11: Comparison of Efficacy after Acupuncture
The somatic symptoms intersect with the concepts of somatization symptoms, Somatization Disorder (SD), Somatoform Disorders (SFD) and Somatic Symptom Disorder (SSD) and have different characteristics. From the perspective of psychosomatic medicine, somatic symptoms are often a sub-health state, which does not belong to the conceptual category of disease. It can be understood as Psychosomatic Disorder (PSD), i.e., a series of pathological manifestations or clinical symptoms occurring under the influence of biological, psychological, social and other factors[5,6]. It affects the factors from many sources, not fully satisfied with the diagnostic criteria of the disease, the course of the disease or short or long, but the human body has social function damage or the subjective experience of the human body has extremely painful feelings (mental and physical). The somatic symptoms of psychosomatic symptoms discussed in this paper, i.e., the clinical phenomenon caused by psychological factors, also known as psychophysiological disorder, is a complex and multi-dimensional medical phenomenon. It involves the interaction between psychological factors and physiological responses, and is manifested in various forms, which may have serious effects on the quality of life, and physical and mental health of patients[7]. In recent years, with the increasing stress of modern society and lifestyle changes, the research in this field has gradually received wide attention, and the deep understanding of the interrelationship between mental health and physical health has increased. Many experts and scholars have also published theoretical and experimental evidence on acupuncture treatment of various mood disorders, mental disorders and other diseases[8-10], although the research results involve or do not involve somatic symptoms, and have certain efficacy on the relief of clinical symptoms, there are few observations and studies on somatic symptoms from the perspective of psychosomatic medicine. Early studies deepened from the biological dimension of disease, mainly focusing on the treatment effect of acupuncture on the physical symptoms produced after the diagnosis of disease, such as chronic pain, insomnia, anxiety and so on[10]. With the deepening of the research, the researchers also found that acupuncture treatment has a significant improvement on a variety of clinical physical symptoms. In a study of anxiety disorders[11], acupuncture treatment has been shown to be effective in relieving patient’s anxiety symptoms, and it achieves anxiety-relief effects by regulating the patient’s autonomic nervous system and endocrine system. This method has been mastered by Chinese medicine long ago, but due to the lack of integration of Chinese medicine theory and modern medicine, it is not recognized by the mainstream of society, and its internal mechanism lacks exploration, so it is given the name of witch doctor. In fact, this treatment is very easy to explain by modern science. Anxiety is accompanied by tension, helplessness and fear, and most patients are in a state of stress and sympathetic excitement, while acupuncture treatment can regulate sympathetic nerve through relevant mechanisms, relieve clinical symptoms, let patients deal with problems in a better state, master the way to solve the problem, and then reduce the incidence of stress events.
At the same time, the TCM theory can also explain the above phenomenon, and its core mechanism is the divine adjustment under the TCM theory. Traditional medicine emphasizes the overall concept and treatment based on syndrome differentiation, and believes that the emotional factor is one of the important causes of physical symptoms. For example, the book psychology of TCM details the relationship between emotional disorders and physical symptoms, pointing out that excessive emotions can lead to air disorders, and then cause a variety of physical discomfort[11]. Modern medicine focuses on exploring the occurrence mechanism of clinical somatic symptoms from the aspects of psychosocial factors and neurobiology. In recent years, remarkable progress has been made in the field of neurobiology, revealing the effects of psychological stress on the immune system, nervous system, etc. For example, a study published in advances in psychological science states that chronic psychological stress can lead to disorders of the immune system that increase the risk of somatic symptoms[12]. However, the understanding and treatment of clinical somatic symptoms in the perspective of traditional medicine and modern medicine are distinctive, but the combination of the two still needs to be deeply studied.
In TCM, spirit is the general term for the phenomenon of human life activities, including spiritual consciousness, perception, movement, which is generated by innate essence. Only spirit exists, people have life activities[12]. Spirit has the command, coordinates the operation of various Zangfu organs, maintains the effective operation of Qi, blood and body fluid, and keeps the meridians smooth. Body fluid is a general term for body fluid, containing body fluids, hormones and neurotransmitters[9]. Qi is a very fine micro substance to maintain life vitality, which has the functions of promoting, warmth, defense, solid photography and gasification, i.e., the Zangfu organs achieve the above functions through blood, body fluids, hormones, neurotransmitters, immune substances and other related substances. Corresponding to modern medicine, spirit in the human body is a general term of all organs, tissues, nervous system, Deoxyribonucleic Acid (DNA), cells, etc., and god adjustment is the regulation of endocrine, neurotransmitters and immune factors and other substances. The clinical data also confirmed that the diagnosis and treatment of psychosomatic diseases is better than the general treatment[12]. The pain that somatic symptoms bring to individuals is often doubled with basic biological therapy alone. From the perspective of TCM, the external physical symptoms are like shape, and their pathological manifestations are like spirit. Under the overall concept of TCM, the physical symptoms under psychosomatic medicine can be well explained and guided by the unity of form and spirit and the unity of nature and man in the treatment[2].
This paper is based on the WCPA classification observation acupuncture treatment effect of psychosomatic symptoms, demonstrated its effectiveness and development progress, the results showed that, the average age is (53±12.63) y old, is in retirement or retirement stage, mentality will inevitably produce corresponding changes, the first age before and after menopause, female than male, married majority (62.3 %), the average total course of disease is relatively long, thus patients with longterm mental and physical double torture. Most of the patients have junior high school education, and college and above also have a development trend, which may be related to the modern social environment model. More and more people with higher education have physical symptoms due to the pressure and other factors transmitted by various parties. This disease season is often frequent in autumn and winter, may be because of the temperature drop, human life activities reduced, biological rhythm adjustment, with the change of the environment will produce depression, suppress mood, interest decline, cannot lift the spirit and other performance. The total score of each scale in the acupuncture group was significantly lower than that before the intervention (p<0.05), while the difference was not significant in the non-acupuncture group, indicating that the acupuncture treatment was effective. However, the difference after the intervention was not significant compared with the conventional treatment in the non-acupuncture group, indicating that there is still much room for improvement in acupuncture therapy. Compared with the scale of sub-dimension score analysis found that acupuncture intervention for SCL-90 scale somatization, depression, anxiety dimension, CMI scale of the skin, nerve, eyes, ears, respiratory, cardiovascular, digestive system of physical performance, and not adapt, depression, anxiety, sensitive, anger, nervous psychological symptoms have better improvement effect. For the symptoms of the muscle and urinary system of the CMI scale, the various classification of the WCPA scale did not improve significantly. The SCL- 90 scale is mainly based on symptoms, which can evaluate and analyze psychological conditions from the side. The CMI scale is mostly used to evaluate individual conditions in normal healthy people or sub-health state, and is clinically applicable to patients with relatively mild diseases. WCPA scale is more inclined to evaluate the patients with PSD with clear physical and psychological symptoms, which is suitable for patients with obvious somatic symptoms of PSD. If the insignificant improvement of symptoms in the WCPA scale may be related to the severity of the symptoms, the average total score of the patients in this study was 49 points±8.4 points, and the scale was 100 points, indicating that the patient’s symptoms were mild and belong to the category of health or sub-health. When the score is not high, the difference in the score change is small. Therefore, the improvement was not significant. Through the scores of the two groups and the scores of each item, it can be seen that the acupuncture treatment group was significantly better than the non-acupuncture treatment group when the overall symptoms were not significantly improved, and the scores were significantly lower in items A, C and D, and the scores were not obvious in items B and E. Therefore, it may affect the efficacy with the surrounding living environment, acupuncture treatment cycle and the severity of the disease, mainly referring to the complex mechanism of cognitive somatic symptoms. One of the meanings of cognitive somatic symptoms refers to the human body’s understanding of its own physical perception, which is variable at any time, flexible and subjective. Therefore, the subjective evaluation of patients is also an influencing factor for the evaluation of the efficacy, which suggests that the theoretical basis can be provided through semistructured interviews or psychotherapy in the future.
And the dimensions of the SCL-90, somatization, anxiety, depression, CMI digestion, skin system, A, C, D were significantly lower, while the improvement of symptoms in other dimensions was not significant. Thus, the difference in the total scores was not significant. Symptoms of somatization, anxiety and depression are related to emotions, and related influencing factors include serotonin, autonomic nervous system, sex hormones, etc. The symptoms of digestive, skin and other systems are mainly related to somatization, anxiety and depression and A, C and D dimensions are mainly related to the presence of obvious symptoms, neurotransmitters and autonomic nervous system. The improvement of these three scores significantly indicates that neurotransmitters and autonomic nervous system are improved, which then improves the obvious existing somatic symptoms. Thus, acupuncture combined electric acupuncture treatment for neurotransmitters, autonomic nervous system, sex hormones, and neurotransmitters, autonomic nervous system, the regulation of sexual hormones and belong to the category of generalized “spirit” of TCM, so acupuncture improve the somatic symptoms of pathogenesis and god of TCM has the same way. The comparative analysis of efficacy in CGI scale showed that the severity of patients receiving acupuncture was mostly mild or moderate (55 % and 36 %), with high response rate (81.82 %), the overall assessment significantly improved, no obvious side effects (82 %), and relatively high efficacy index (all >1.0 points). It can be found that acupuncture combined with electroacupuncture therapy has some advantages.
Therefore, it has important theoretical and practical significance to the study of the perspective of psychosomatic medicine. Through the comprehensive theories and treatment methods of traditional medicine and modern medicine, we can diagnose and treat such diseases more comprehensively and provide patients with more effective treatment plans. At the same time, clinical medicine has the advantages of prospective and flexible thinking in the understanding of physical symptoms and classification. This also helps to promote the in-depth integration and development of traditional medicine and modern medicine in the field of psychosomatic medicine. This study shows that acupuncture combined with electroacupuncture has significant clinical effect in treating somatic symptoms, and acupuncture treatment can effectively relieve physical symptoms, improve quality of life, improve social function, and have high safety. Compared with traditional drug therapy, combination therapy has a more comprehensive and in-depth mechanism of action, which can provide comprehensive treatment for patients from multiple aspects, with a short cycle and relatively small side effects, which can provide more comprehensive, effective and cost-effective medical services for the majority of patients. Therefore, we recommend further promotion and application of acupuncture combined with electroacupuncture for treating somatic symptoms from a psychosomatic medical perspective in clinical practice.
In conclusion, this study provides a safe and effective treatment method for the regulation of somatic symptoms in the field of psychosomatic medicine. However, due to the insufficient sample size and short observation time, only 77 PSD patients with somatic symptoms were collected as the study subjects before and after treatment, and some study subjects who were not identified but chose to go to other departments for symptomatic treatment were not included. The research data are insufficient, the results are not completely authoritative and convincing; secondly, due to the researcher’s weak communication ability, the subjective interpretation in the scale is not easy, and the self-evaluation results may be slightly different. Clinical application prospect of TCM comprehensive treatment, future research can also expand the scale and time, pay attention to the rule of acupoint scientific and validity, according to different people, using more rigorous test design and control test to verify, by comparing different treatment effect of the method, to explore the relationship between the rule and individual differences, can provide a more reliable basis for clinical practice, for the development of psychosomatic medicine to provide more scientific basis.
Conflict of interests:
The authors declared no conflict of interests.
References
- Verma ML, Sharma P, Singh U, Sachan R, Sankhwar PL. Comparison of acceptability and efficacy of thermal ablation (thermocoagulation) and cryotherapy in via positive cervical lesions: A pilot study. Indian J Med Res 2023;158(4):423-31.
[Crossref] [Google Scholar] [PubMed]
- Zhang S, Ding R, Chen S, Meng X, Jianchao L, Wang DW, et al. Availability and trend of dissemination of cardiac rehabilitation in China: Report from the multicenter national registration platform between 2012 and 2021. Front Cardiovasc Med 2023;10:1210068.
- Jun MH, Kim YM, Kim JU. Modern acupuncture-like stimulation methods: A literature review. Integr Med Res 2015;4(4):195-219.
[Crossref] [Google Scholar] [PubMed]
- Li L, Zhang Y, Feng S, Cao Y, Li H, Li X, et al. Reliability and validity of the brief psychosomatic symptom scale (BPSS) in patients from general hospitals. Gen Hosp Psychiatry 2023;83:1-7.
[Crossref] [Google Scholar] [PubMed]
- Merdler I, Chitturi KR, Chaturvedi A, Rahman S, Cellamare M, Ozturk ST, et al. Exploring the interplay between coronary microvascular dysfunction and mental health. Cardiovasc Rev Med 2024.
[Crossref] [Google Scholar] [PubMed]
- Abdolkarimi M, Sadeghi-Yarandi M, Sakari P. Investigating the relationship between personality traits of hardiness and perfectionism with stress and psychosomatic symptoms: A cross-sectional study among nurses in Iran. BMC Psychol 2024;12(1):323.
[Crossref] [Google Scholar] [PubMed]
- Krug A, Stein F, David FS, Schmitt S, Brosch K, Pfarr JK, et al. Factor analysis of lifetime psychopathology and its brain morphometric and genetic correlates in a transdiagnostic sample. Transl Psychiatry 2024;14(1):235.
- Yin J, Chen Y, Huang M, Cao Z, Jiang Z, Li Y. Effects of perineal massage at different stages on perineal and postpartum pelvic floor function in primiparous women: A systematic review and meta-analysis. BMC Pregnancy Childbirth 2024;24(1):405.
[Crossref] [Google Scholar] [PubMed]
- Lleó A, Alcolea D. What can blood biomarkers tell us about patients with Lewy body dementia?. Neurology 2024;102(12):e209505.
[Crossref] [Google Scholar] [PubMed]
- Guo J, Luo HC. Differentiation of somatoform disorders in TCM acupuncture-moxibustion outpatient service. Zhongguo Zhenjiuxue 2006;26(11):814-7.
[Google Scholar] [PubMed]
- Vickers AJ, Cronin AM, Maschino AC, Lewith G, MacPherson H, Foster NE, et al. Acupuncturefor chronic pain: Individual patient data meta-analysis. Arch Intern Med 2012;172(19):1444-53.
[Crossref] [Google Scholar] [PubMed]
- Zhang D, Jiang H, Yang X, Zheng S, Li Y, Liu S, et al. Traditional Chinese medicine and renal regeneration: Experimental evidence and future perspectives. Chin Med 2024;19(1):77.
[Crossref] [Google Scholar] [PubMed]
 ): Mild; (
): Mild; ( ): Moderate and (
): Moderate and ( ): Severe
): Severe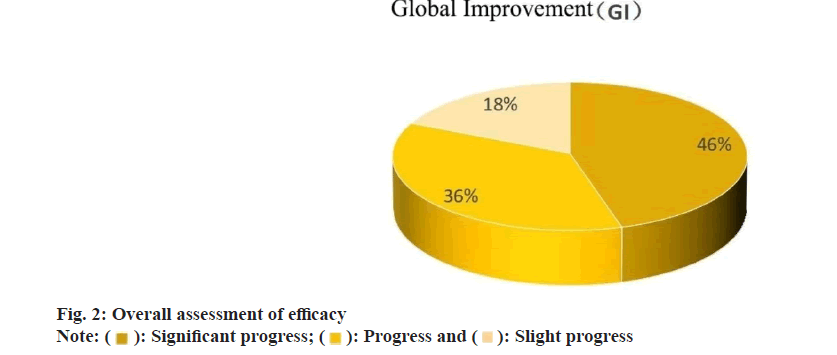
 ): Significant progress; (
): Significant progress; ( ): Progress and (
): Progress and ( ): Slight progress
): Slight progress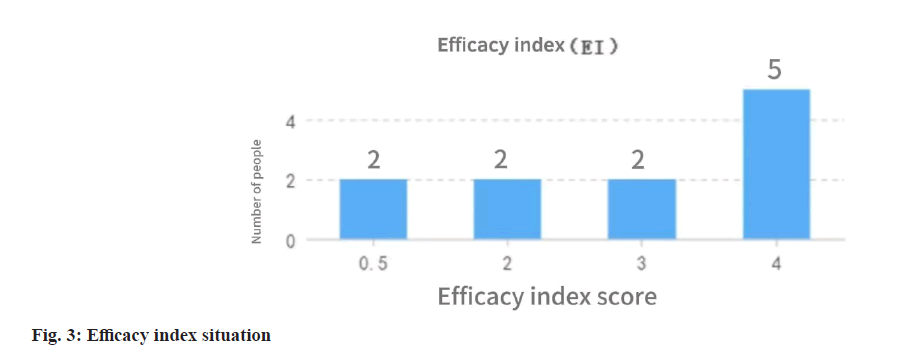
 ): Not have and (
): Not have and ( ): Mild
): Mild



