- *Corresponding Author:
- Rihong Bin
Department of Pre-Hospital Emergency Medicine, Zhuzhou Central Hospital, Zhuzhou, Hunan 412000, China
E-mail: 15973360008@163.com
| This article was originally published in a special issue, “Clinical Advancements in Life Sciences and Pharmaceutical Research” |
| Indian J Pharm Sci 2024:86(5) Spl Issue “54-59” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
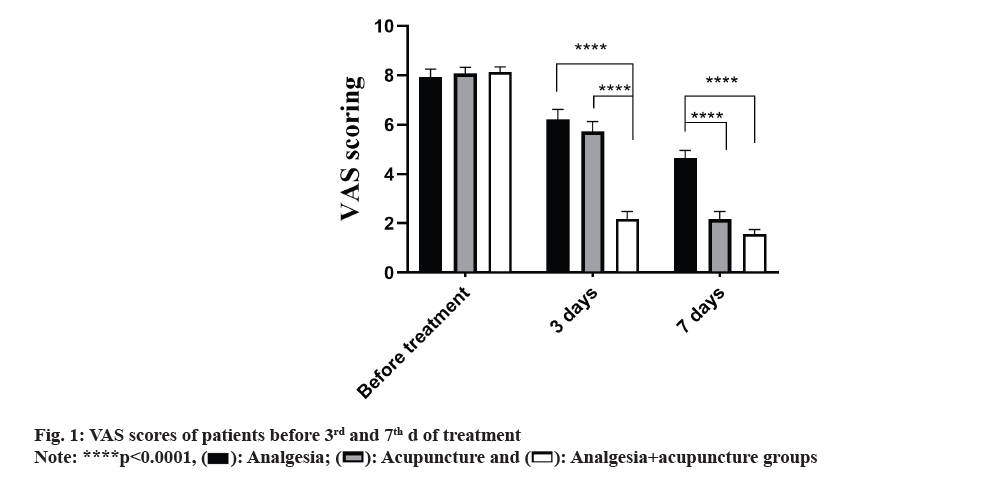
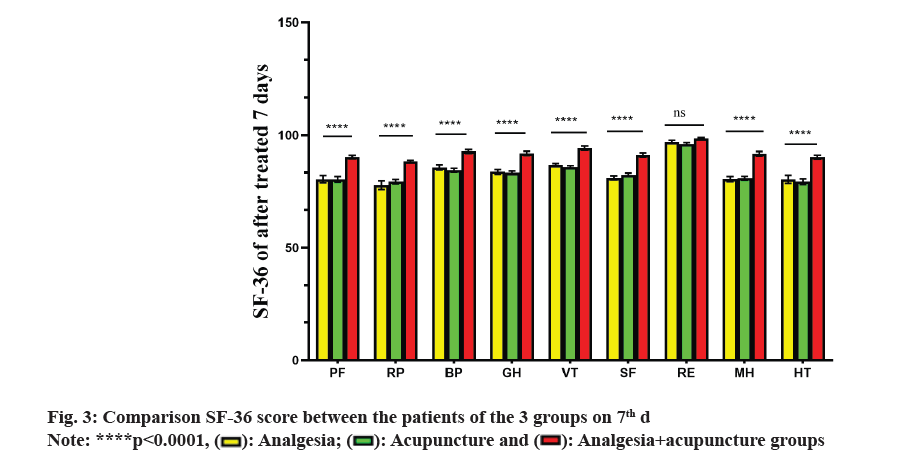
The objective of this study was to explore the therapeutic effect of analgesics combined with acupuncture on postherpetic neuralgia. 52 individuals suffering with postherpetic neuralgia were selected from Zhuzhou Central Hospital from January 2020 to 2021 and were divided into three groups who were treated with analgesics, acupuncture and combination of analgesics with acupuncture. All the individuals were evaluated for pain intensity, length of hospital stay and quality of life before and after 7 d of the treatment. Pain intensity and quality of life were evaluated using the visual analogue scale and medical outcomes study short form-36 health survey. Before treatment, no difference among three groups in their baseline characters like age, gender, visual analogue scale score and short form-36 were found (p>0.05). The visual analogue scale scoring of analgesia+acupuncture group significantly decreased compared with those of the analgesia and acupuncture groups on 3rd and 7th d ((p<0.0001 and p=0.003) and (p<0.0001 and p=0.109)). Analgesia+acupuncture group exhibited significantly shorter length of hospital stay than the other two groups (p<0.0001). On 7th d after treatment, short form-36 score of analgesia+acupuncture group was better than the other two groups (p<0.0001). This study promotes the treatment of patients with postherpetic neuralgia using analgesics with acupuncture which can help to relieve pain, shorten the hospital stay and improve the quality of life.
Keywords
Acupuncture, analgesia, postherpetic neuralgia, herpes zoster
Herpes Zoster (HZ) is a skin disease which is caused by the reactivation of varicella zoster virus after previous infection[1]. It develops in bands along the peripheral nerves on one side of the body whose main symptom is to cause neuropathic pain[2]. Postherpetic Neuralgia (PHN) often occurs in the elderly or immune compromised patients. After the surface of the skin heals, the pain lasts for 3 mo or even longer[3]. PHN is the most common type of neuropathic pain which often occurs in elderly or immunocompromised patients and is a self-limited disease[3,4]. The incidence rate and prevalence of PHN vary based on the duration and intensity of pain. A meta-analysis study reported that the annual rate of incidence of PHN is 3.9 %-42 % individuals among 100 000 individuals[4]. The annual rate of incidence and prevalence rate of HZ and PHN are gradually increasing with age[5]. Approximately 65 % of the patients with HZ aged 60 y and above can develop PHN while 75 % of the patients with HZ aged 70 y and above can develop PHN[6].
The clinical manifestations of PHN are complex and diverse, which can be intermittent or persistent. Common pain sites of PHN include unilateral chest, trigeminal nerve (mainly the ophthalmic branch) or neck, with the chest accounting for 50 % while the head, face, neck and waist accounting for 10 %-20 %, the sacrococcygeal region accounting for 2 %-8 % and the other parts accounting for <1 %[7]. The pain area of PHN is usually larger than the blister area and very few patients develop bilateral herpes[8]. PHN pain is divided into peripheral and central neuralgia, which involves a variety of receptors, pathways and transmitters[9]. Presently, analgesic drugs are the 1st choice of therapy, which are prescribed to decrease the clinical symptoms of pain. Oral and topical medications are the traditional treatments of PHN. At present, tricyclic antidepressants, pregabalin and 5 % lidocaine patches have been recommended as 1st line treatment[10]. Although these drugs can relieve pain, they still have several side effects such as sedation, xerostomia, confusion, dysrhythmia, weight gain, dizziness, somnolence, fatigue and ataxia[11]. Analgesic drugs are metabolized mainly in the liver and kidney[12]. Therefore, the use of analgesics is limited in patients with chronic renal insufficiency and liver function damage.
Acupuncture is a vital part of traditional Chinese medicine which is used to treat systemic diseases through the conduction of meridians and acupoints[13]. Acupuncture and moxibustion have strong practicability, which are used for treating a wide range of diseases. They exert unique therapeutic effects on diseases involving chronic strain in the joints and muscles[14]. Owing to the unique advantages of acupuncture for treating certain illnesses, the World Health Organization (WHO) has publicly declared the advantages of acupuncture in some diseases[15]. Presently, WHO has reported 43 types of diseases, including respiratory, ophthalmic diseases, oral (such as toothache, gingivitis and pain relief after tooth extraction) and gastrointestinal diseases, nerve, muscle, and bone diseases, headaches, migraine, intercostal neuritis, arthritis, lumbago and mild hemiplegia after stroke, which can be treated using acupuncture and moxibustion treatment with good therapeutic effects[15]. In order to explore the therapeutic effect of acupuncture on PHN, we collected 52 patients with PHN and randomly divided them into three groups for pain medication, acupuncture and pain medication combined with acupuncture.
Materials and Methods
General information:
52 individuals of PHN who were admitted in Zhuzhou Central Hospital from January 2019 to January 2021 were considered for this study. The study was approved by the This study was approved by the Ethics Committee of Zhuzhou Central Hospital (Approval No: 2018-08105) and all the patients provided written informed consent.
Inclusion criteria: Patients who were diagnosed and were confirmed to have PHN; patients who had complete clinical data information; patients having signed informed consent to participate in the study and patients whose Visual Analogue Scale (VAS) score was>6 were included in this study.
Exclusion criteria: Patients suffering from progressive chronic renal insufficiency or liver damage; patients who were allergic to the drugs used in the study and patients who did not provide consent to participate in treatment were excluded from the study.
Study design:
52 patients were randomly divided into three groups. 1st group had 14 patients (n=14) who were treated with analgesics (analgesic group), while the 2nd group had 16 patients (n=16) who were treated with analgesics combined with acupuncture (analgesic+acupuncture group) and the 3rd group included 22 patients (n=22) who were treated with acupuncture only (acupuncture group).
Analgesic drug treatment included 5 % of lidocaine and tramadol patches (Beijing Tede Pharmaceutical Co., Ltd., having Approval No: H20180007), which was given once/d. It was applied cumulatively within 24 h not exceeding 12 h. Similarly, pregabalin capsule (Qilu Pharmaceutical, Hainan Pharmaceutical Co., Ltd., with Approval No: 101106-201902) was used in the study. 75 mg of pregabalin was used as initial dose, followed by twice/day or once 50 mg, thrice/ day. Tramadol was also included in the study. The observation indicators after treatment was compared among
Ashi acupoint was considered as the main acupoint in acupuncture therapy. The area around the skin lesion (about 0.5-1 inch from herpes lesions) is generally considered to be the location of ashi acupoint.
Observation indicators:
For evaluating the therapeutic efficacy of the drugs, we studied intensity of pain, Quality of Life (QOL) and the adverse effects observed among the patients of the 3 groups.
VAS: VAS score was used to evaluate the pain intensity where 0 to 1 points was comprehended to have no pain; 2-4 points corresponded for mild pain while 5-7 points was considered as moderate pain and 8-10 points indicted severe pain[16]. VAS pain score self-evaluation forms were collected before and after the 3rd, 5th and 7th d treatment.
QOL: Medical Outcomes Study (MOS) 36-item Short-Form (SF)-36 health survey was used to evaluate the QOL of the patients[17]. SF-36 included 9 major and important aspects which included Physical Functioning (PF), Role Physical (RP), Body Pain (BP), General Health (GH), Vitality (VT), Functioning (SF), Role Emotional (RE), Mental Health (MH) and reported Health Transition (HT). High score indicated better health status.
Adverse effects: After 7 d of the treatment, we recorded the adverse events such as dizziness, drowsiness, vomiting and dry vomiting in patients of the 3 groups.
Statistical analysis:
Statistical Package for Social Sciences (SPSS) version 21.0 statistical software was used for analyzing the collected data. Measured data was expressed as mean±standard deviation; t-test was performed for the comparative analysis among the groups while the comparison of multiple groups was performed using a one-way Analysis of Variance (ANOVA) where p<0.05 was considered to be statistically significant.
Results and Discussion
The clinical baseline data characteristics of the patients such as age, gender, VAS scores, renal function and were analyzed. A total of 52 patients were enrolled in the study. Of note, 14 patients were treated with analgesia, 22 patients were treated with acupuncture, and 16 patients were treated with analgesia add acupuncture. No significant difference was found in terms of age, gender, VAS scoring, renal function and SF-36 survey scores among the three groups before treatment (p>0.05) (Table 1). 5 patients of the analgesic group were given tradamdol while 8 patients were given pregabalin orally. Patients of analgesia+acupuncture group were treated with oral tramadol besides acupuncture.
| Clinical characteristics | Group | p | ||
|---|---|---|---|---|
| Analgesia | Acupuncture | Analgesia+acupuncture | ||
| Age | 58.14±4.26 | 57.86±3.43 | 0.867 | |
| Gender | 1 | |||
| Male | 7 | 11 | 10 | |
| Female | 7 | 11 | 6 | |
| Site of pain | 0.669 | |||
| Chest | 12 | 15 | 11 | |
| Face | 2 | 7 | 5 | |
| VAS score | 0.27 | |||
| 2-4 | 0 | 0 | 0 | |
| 5-7 | 4 | 3 | 3 | |
| 8-10 | 10 | 19 | 11 | |
| Other therapy | 5 | 8 | 2 | 0.34 |
Table 1: Clinical Data of 52 Patients with Herpes Zoster
VAS scoring and length of hospital stay of the three groups was compared and analyzed where we found no difference before and after treatment (p>0.05) (fig. 1); however, the VAS score in analgesia+acupuncture group significantly decreased on 3rd d (p<0.0001). While we observed that the VAS score significantly decreased in acupuncture and analgesia+acupuncture groups than analgesia group on 7th d (p<0.0001). Similarly, compared with acupuncture and acupuncture+analgesia group, there was no difference in VAS scores (p>0.05). On the 3rd d, compared with the VAS scores of acupuncture and analgesia groups, no difference was found in their VAS scores (p=0.842).
Subsequently, length of the hospital stay in analgesia, acupuncture and analgesia+acupuncture groups were 11.36±2.21, 9.54±1.57 and 7.25±0.58 d, respectively. While comparing the hospital stay of the three groups, analgesia+acupuncture group depicted significantly shorter than the other two groups (p<0.0001 and p<0.05) (fig. 2). However, there was no difference between analgesia group and acupuncture group (p>0.05).
Further, QOL of the 3 groups was evaluated using SF-36 health score. Before treatment, SF-36 was not significantly different among the 3 groups (p>0.05) (Table 2). On 7th d after the treatment, SF-36 in analgesia+acupuncture group was better than those of the other two groups (p<0.0001) (fig. 3). However, SF-36 of the analgesia and acupuncture groups were not significantly different (p<0.05). In addition, in the 3 groups we found 2 patients who experienced dizziness while 1 patient experience vomiting as adverse reactions.
| Components of SF-36 | Analgesia | Acupuncture | Analgesia+acupuncture | p |
|---|---|---|---|---|
| PF | 68.71±5.09 | 69.18±4.92 | 68.86±5.51 | >0.05 |
| RP | 28.93±6.56 | 28.86±7.55 | 27.95±5.49 | |
| BP | 70.57±6.99 | 72.32±6.69 | 70.59±5.15 | |
| GH | 78.29±5.57 | 78.91±5.64 | 76.59±4.94 | |
| VT | 78.14±3.39 | 75.36±5.43 | 76.5±5.8 | |
| SF | 60.29±3.47 | 60.76±4.94 | 59.67±4.81 | |
| RE | 93.36±4.50 | 91±4.23 | 91.27±4.68 | |
| MH | 71.57±3.44 | 67.45±6.08 | 65.64±5.58 | |
| HT | 53.07±4.53 | 54.86±4.6 | 55.82±4.52 |
Table 2: Sf-36 Evaluated QOL among The 3 Groups before Treatment
According to the traditional Chinese medicine, PHN is called snake like sore and is generally believed to be associated with wind, dampness, heat and pathogenic factors, which are mostly caused by the accumulation of heat and toxins[18]. The main mechanism of PHN primarily includes qi, blood and pain impassability. Further, it includes the transformation of evil into fire. The main principles of treating PHN using traditional Chinese medicine are include removal of blood stasis, relieving pain, clearing the liver and purging fire[18]. According to the modern medical research, HZ is mainly distributed to the waist, chest and abdomen which accounts for about 70 % of the population followed by trigeminal HZ which accounts for approximately 20 %-30 % of the population. This virus mainly invades the spinal nerve and trigeminal nerve, thereby causing pain. The posterior branches of spinal nerves are distributed around the huatuo-jiaji acupoint. Therefore, acupuncture or electroacupuncture at this acupoint can block the conduction of pain fibers in the nerve.
In this study, 52 patients suffering with PHN were treated with analgesia, acupuncture and a combination of both the treatments. The results showed that analgesia combined with acupuncture significantly relieved pain and shortened the length of hospital stay. However, no difference was found in terms of pain relief and shorter hospital stays between the analgesia and acupuncture groups. SF-36 evaluation showed that analgesia+acupuncture group exhibited better QOL than the other two groups. Wang et al.[19] found that 74 patients who were treated with HZ sequelae neuralgia using electroacupuncture at Huatuo-Jiaji acupoints combined with moxibustion had better therapeutic effect.
Similarly, Ling et al.[20], found that fire needle cupping was superior to perioperative acupuncture cupping in the treatment of PHN patients. Two studies compared acupuncture and pharmacological therapy for treating PHN which utilized valaciclovir hydrochloride, carbamazepine, mecobalamine and vitamin B12. The results favored acupuncture with Mean Difference (MD) of 1.80, 95 % Confidence Interval (CI) of 1.72-1.87 and p<0.001. Furthermore, the pharmacological therapy reported 5 patients with stomach discomfort and 8 patients with vomiting[21,22]; acupuncture groups reported no complications. In another study, 70 patients with PHN were treated with elongated needles, bloodletting and cupping techniques while the control patients were treated with pregabalin[23]. VAS and QOL of the acupuncture group were improved compared with those of the pharmacological therapy where the MD was 3.78, 95 % CI was 2.59-4.97 and p<0.001. These results indicated that acupuncture is better than other treatments for PHN. Furthermore, in a study conducted by Ursini et al.[24] for treating PHN using superficial dry-needling (acupuncture) and sham acupuncture reported that acupuncture was not superior to sham acupuncture.
However, in this study VAS score>8 and pain could not be relieved using acupuncture treatment alone on 3rd or 4th d of the treatment. The patients could not tolerate the pain and required analgesic treatment as well; thus in analgesia group, 1/3rd of the patients required combination medication to tolerate the pain. The treatment outcome was satisfactory only in the analgesia combined with acupuncture and moxibustion treatment group. The result indicated that acupuncture alone cannot give better results than analgesia alone if the VAS score>8.
Although small sample size is a limitation of this study, we found that acupuncture combined with analgesia is a better way to relieve pain, shorten the length of hospital stays and improve the QOL of patients with PHN. So, conclusively we suggest combination of acupuncture with analgesia is worth of further clinical studies.
Author’s contributions:
Xinsheng Zheng and Huan Chen participated in drafting and designing the manuscript, and performed statistical analysis. Juan Yi, Jiaying Huang, Qipeng Tan and Cheng Huang collected clinical data, helped to draft the manuscript and performed statistical analyses. Rihong Bin conceived, designed the study and was involved in revision of the manuscript. All authors read and approved the final manuscript.
Funding:
This study was supported by the Hunan Administration of Traditional Chinese Medicine (Grant no: 2020104).
Conflict of interests:
The authors declared no conflict of interests.
References
- Schmader K. Herpes zoster. Ann Intern Med 2018;169(3):1-16.
[Crossref] [Google Scholar] [PubMed]
- Gnann JW Jr, Whitley RJ. Clinical practice. Herpes zoster. N Engl J Med 2002;347(5):340-6.
[Crossref] [Google Scholar] [PubMed]
- Gauthier A, Breuer J, Carrington D, Martin M, Rémy V. Epidemiology and cost of herpes zoster and post-herpetic neuralgia in the United Kingdom. Epidemiol Infect 2009;137(1):38-47.
[Crossref] [Google Scholar] [PubMed]
- Johnson RW, Rice AS. Clinical practice. Postherpetic neuralgia. N Engl J Med 2014;371(16):1526-33.
[Crossref] [Google Scholar] [PubMed]
- Forbes HJ, Thomas SL, Smeeth L, Clayton T, Farmer R, Bhaskaran K, et al. A systematic review and meta-analysis of risk factors for postherpetic neuralgia. Pain 2016;151(1):30-54.
[Crossref] [Google Scholar] [PubMed]
- Gruver C, Guthmiller KB. Postherpetic neuralgia. In: StatPearls 2023.
[Google Scholar] [PubMed]
- Massengill JS, Kittredge JL. Practical considerations in the pharmacological treatment of postherpetic neuralgia for the primary care provider. J Pain Res 2014;7:125-32.
[Crossref] [Google Scholar] [PubMed]
- Ngo AL, Urits I, Yilmaz M, Fortier L, Anya A, Oh JH, et al. Postherpetic neuralgia: Current evidence on the topical film-forming spray with bupivacaine hydrochloride and a review of available treatment strategies. Adv Ther 2020;37(5):2003-16.
[Crossref] [Google Scholar] [PubMed]
- Dworkin RH, Gnann JW Jr, Oaklander AL, Raja SN, Schmader KE, Whitley RJ. Diagnosis and assessment of pain associated with herpes zoster and postherpetic neuralgia. J Pain 2008;9:S37-44.
[Crossref] [Google Scholar] [PubMed]
- Kim SR, Khan F, Ramirez-Fort MK, Downing C, Tyring SK. Varicella zoster: An update on current treatment options and future perspectives. Expert Opin Pharmacother 2014;15(1):61-71.
[Crossref] [Google Scholar] [PubMed]
- Derry S, Wiffen PJ, Moore RA, Quinlan J. Topical lidocaine for neuropathic pain in adults. Cochrane Database Syst Rev 2014;2014(7):1-11.
[Crossref] [Google Scholar] [PubMed]
- Baldo BA. Opioid analgesic drugs and serotonin toxicity (syndrome): Mechanisms, animal models, and links to clinical effects. Arch Toxicol 2018;92(8):2457-73.
[Crossref] [Google Scholar] [PubMed]
- Wen J, Chen X, Yang Y, Liu J, Li E, Liu J, et al. Acupuncture medical therapy and its underlying mechanisms: A systematic review. Am J Chin Med 2021;49(1):1-23.
[Crossref] [Google Scholar] [PubMed]
- Vickers AJ, Vertosick EA, Lewith G, MacPherson H, Foster NE, Sherman KJ, et al. Acupuncture for chronic pain: Update of an individual patient data meta-analysis. J Pain 2018;19(5):455-74.
[Crossref] [Google Scholar] [PubMed]
- World Health Organization acupuncture list of conditions. Public Health Nigeria;1979.
- Price DD, McGrath PA, Rafii A, Buckingham B. The validation of visual analogue scales as ratio scale measures for chronic and experimental pain. Pain 1983;17(1):45-56.
[Crossref] [Google Scholar] [PubMed]
- Azen SP, Palmer JM, Carlson M, Mandel D, Cherry BJ, Fanchiang SP, et al. Psychometric properties of a Chinese translation of the SF-36 health survey questionnaire in the well elderly study. J Aging Health 1999;11(2):240-51.
[Crossref] [Google Scholar] [PubMed]
- Liu ZS, Peng WN, Liu BY, Wang J, Wang Y, Mao M, et al. Clinical practice guideline of acupuncture for herpes zoster. Chin J Integr Med 2013;19(1):58-67.
[Crossref] [Google Scholar] [PubMed]
- Wang Q, Yang L, Wang Y. The therapeutic effect of electroacupuncture at jiaji point combined with mild moxibustion on postherpetic neuralgia. Genomics Appl Biol 2018;37(12):5473-9.
- Ling X, Xu Qi, Ke M. Comparison of therapeutic effects of different acupuncture methods combined with cupping in the treatment of postherpetic neuralgia in middle-aged and elderly patients. 2022.
- Li W, Cai G, Wang Y. Clinical observation of 30 cases of PHN with electroacupuncture and bloodletting. Mod Diagn Treat 2014;25(7):1506-7.
- Wang M, Cai S. Clinical observation of acupuncture combined with plum blossom tapping and cupping treatment to shingles neuralgia. J Shanxi Univ Chin Med 2017;40:58-66.
- Wang X, Zhang F, Xu A. Observation of elongated needle and bloodletting for PHN. J Pract Tradit Chin Med 2015;31(10):943-4.
- Ursini T, Tontodonati M, Manzoli L, Polilli E, Rebuzzi C, Congedo G, et al. Acupuncture for the treatment of severe acute pain in herpes zoster: Results of a nested, open label, randomized trial in the VZV pain study. BMC Complement Altern Med 2011;11:1-8.
[Crossref] [Google Scholar] [PubMed]
 ): Analgesia; (
): Analgesia; ( ): Acupuncture and (
): Acupuncture and ( ): Analgesia+acupuncture groups
): Analgesia+acupuncture groups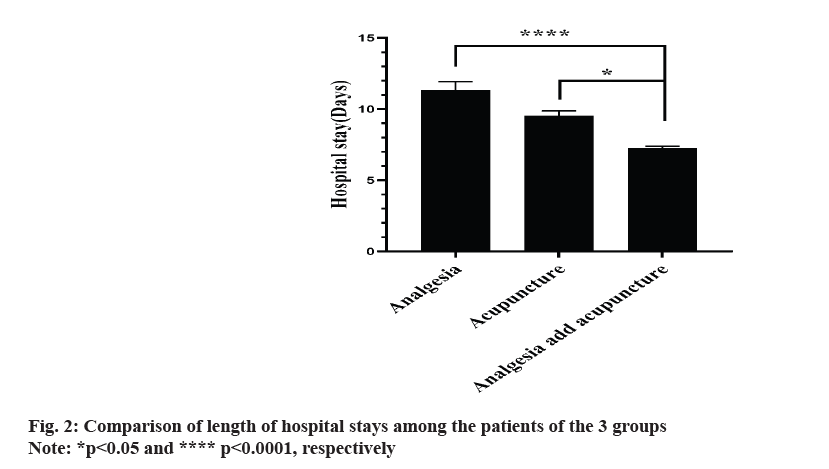
 ): Analgesia; (
): Analgesia; ( ): Acupuncture and (
): Acupuncture and ( ): Analgesia+acupuncture groups
): Analgesia+acupuncture groups



