- *Corresponding Author:
- Yunji Xu
Department of General Surgery, Second Affiliated Hospital, Hengyang Medical School, University of South China, Hengyang, Hunan Province 421001, China
E-mail: xuyunji1122@163.com
| This article was originally published in a special issue, “Clinical Advancements in Life Sciences and Pharmaceutical Research” |
| Indian J Pharm Sci 2024:86(5) Spl Issue “67-73” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
Due to the high recurrence and mortality rate of liver cancer, most of the people are prone to mental disorders after diagnosis and during the treatment process. Depression is one of the most common mental disorders. 8 %-24 % of cancer individuals experience depression. Depression can significantly interfere with a patient’s ability to cope with cancer, physical symptoms and treatment which can have a negative impact on treatment effectiveness. In this study, we studied the clinical information of 42 individuals with liver cancer complicated with depression where we divided them into control and treatment groups. The treatment group (n=24) was treated with fluoxetine, psychological counselling combined with acupuncture while control group (n=18) was treated with fluoxetine and psychological counselling. We have comparatively analysed the hospital anxiety and depression scale scores and tumors disease progression in two groups. We did not find any difference in age, tumor staging, liver cancer treatment plan and pre-treatment hospital anxiety and depression scale score between the two groups (p>0.05). The cure rate of the treatment group was significantly higher than that of the control group (p<0.05). Similarly, the disease progression of liver cancer was significantly better in the cure and stabilized of depression (p=0.017 and p=0.012).
Keywords
Acupuncture, liver cancer, selective serotonin reuptake inhibitor, fluoxetine, moxibustion
Liver cancer is the most common malignant tumor worldwide and 905 677 (4.7 %) new cases have been recorded and accounted for 830 180 (8.3 %) new deaths in 2020 alone[1]. The latest data shows that China has 389 000 new cases of liver cancer annually, ranking 4th among malignant tumors[2]; the annual mortality rate is 336 000, ranking 2nd among malignant tumor deaths where the disease burden is heavy[2].
People widely understand that suffering from cancer is endless pain, torment leading to death[3]. The diagnosis and treatment of cancer can bring many different emotions to patients such as anger, confusion, fear, anxiety and sadness[4]; for some patients, sadness can evolve into a serious problem. Depression is one of the most common mental disorders[5] and research has shown that the incidence of depression in cancer patients ranges from 8 %-24 %[5]. The occurrence of depression is influenced by many factors, including general factors (gender, age and family income), disease and treatment factors (cancer type, stage and treatment plan), tolerance to pain, educational level, family and social environment factors[6]. Depression can significantly interfere with patient’s ability to cope with cancer, physical symptoms and treatment which can have a negative impact on treatment effectiveness[6]. It includes changes in medical compliance, increased hospitalization rate and length of hospital stay, increased suicidal ideation and mortality[7]. However, the high recurrence and mortality rate of liver cancer is more likely to lead to patient frustration and despair. Therefore, it is very necessary to take corresponding interventions to reduce the incidence rate of depression in liver cancer patients.
Fluoxetine is a Selective Serotonin Reuptake Inhibitor (SSRI) that can effectively inhibit neurons from taking up serotonin from synaptic gaps, increasing the availability of this neurotransmitter in the gaps for practical use, thereby improving emotional states and treating depressive disorders[8-12]. Acupuncture is an ancient technique, belonging to traditional Chinese medicine[13] which is a promising non pharmacological treatment for alleviating depressive symptoms, that can replace medication or supplement treatment to improve outcomes[14]. Compared with drug therapy, acupuncture has the advantage of low cost and minimal side effects[15]. In addition, increasing evidence suggests that acupuncture combined with medication is more effective, safe, well tolerated and effective than medication alone, reflecting the potential benefits of acupuncture combined with medication in treating depression[16].
In this study, we retrospectively collected clinical data from 42 individuals with liver cancer complicated with depression and were divided into control and treatment groups. The treatment group, included 24 individuals who were treated with drugs, psychological counselling combined with acupuncture and moxibustion while the observation group included 18 individuals were treated with drug psychological counselling. We compared Hospital Anxiety and Depression Scale (HADS) scores and tumors disease progression in both the groups.
Materials and Methods
General information:
The clinical data of all the individuals were diagnosed liver cancer complicated with depression in Zhuzhou Central Hospital from January 2022 to January 2024 was collected. The diagnosis of liver cancer was confirmed by two pathologists and has been completed the standard treatment. The diagnostic criteria for depression are based on the Diagnostic and Statistical Manual 5th edition (DSM-5) of mental disorders[17]; the screening method adopted was HADS[18]. Based on inclusion and exclusion criteria, the individuals were divided into two groups, control and treatment groups. The control group was given SSRI medication (fluoxetine) and psychological counselling, while the treatment group was given SSRI medication (fluoxetine) and psychological counselling combined with acupuncture. All the patients provided written informed consent for treatment which was approved by the Ethics Committee of the Department of General Surgery, Second Affiliated Hospital, Hengyang Medical School, University of South China (Approval No: 2021094-14-HYMS).
Inclusion criteria: Patients diagnosed with liver cancer complicated with depression; patients who have completed liver cancer treatment; patients having no mental disorders previously; patients with liver cancer survival time >6 mo and patients with signed informed consent forms were included in the study.
Exclusion criteria: Patients not having liver cancer; patients having the history of depression or mental disorders previously and patients who are unable to adhere to treatment plan were excluded from the study.
Treatment:
Control group was given fluoxetine hydrochloride medication along with psychological counselling, while the treatment group was given fluoxetine medication and psychological counselling combined with acupuncture.
Medication: 2 tablets of 10 mg fluoxetine hydrochloride (Changzhou Siyao Pharmaceutical Co., Ltd., (Approval No: H19980139)) was given after breakfast orally, once daily for a course of 4 w.
Psychological counselling: Cognitive Behavioral Therapy (CBT) technique provides patients to face fear and gradually eliminate the fear through repeated exposure and experience while relaxation training helps the patients to control their anxiety levels through relaxation and breathing control techniques.
Acupuncture: Acupuncture points taichong (bilateral), Hegu (bilateral), Shenmen (bilateral), Baihui and Yintang used 0.35 mm3 and 25 mm millineedles, after routine disinfection. Primarily we injected the acupoints, Taichong, Hegu and Shenmen vertically and slowly, with a depth of 15 mm. Then we evenly lifted, inserted, twisted and rotated the technique until qi is obtained. Further needle was inserted at baihui at a 30° to the scalp. Quickly we inserted the needle under the scalp for 15 mm, then at Yintang acupoint where the local skin was pinched at level of 15 mm of the needle. Further, both Baihui and Yintang acupoints were twisted evenly, breathing was stopped immediately and the needle was left for 30 min; the treatment was followed once/day for the course of 4 w.
Observation indicators:
HADS score: 0-7 points is classified to be asymptomatic while 8-10 points belong to suspicious symptoms and 11-21 points definitely depict symptoms[18]. According to the HADS score, 0-7 points depicted disappearance of cured symptoms with normal emotions; score between 8-10 show improved symptoms with stabilized mood. 11-21 points denoted no improvement in symptoms or emotions.
Disease progression: Alpha-Fetoprotein (AFP) was evaluated using radioimmunoassay where we found elevated level of protein (>25 ng/ml) and Computed Tomography (CT) findings detected new tumors, lymph node metastases and distant metastases in other areas. Liver cancer patients were tested for AFP every month while liver CT was carried for every 3 mo.
Quality of life: Quality of Life Enjoyment and Satisfaction-Questionnaire (Q-LES-Q) was used to evaluate the quality of life of patients. This evaluation form contains a total of 16 self-assessment items. Each grade was divided into points 1-70. 1 point depicted highly dissatisfied and 2 points denoted dissatisfied. There are 5 levels where 3 points mean average, 4 points means satisfied and 5 points comprehended as highly satisfied. The total score ranged from 14- 70 points. Higher score depicted better happiness and quality of life satisfaction among the patients. The first 14 items were used to generate the total score, while the remaining 2 items were separate which were used to evaluate and study drug related satisfaction and overall quality of life[19].
Statistical analysis:
Data analysis was conducted using Statistical Package for Social Sciences (SPSS) version 26.0 software. Normally distributed continuous data was represented in terms of mean±standard deviation (x̄ ±s). Categorical data were presented as frequencies (n) and data comparisons were conducted using Chisquare (χ2) tests or the Monte Carlo method where p<0.05 was considered to be statistically significant; two-sided tests were performed, with a significance level set at Alpha (α)=0.05.
Results and Discussion
Clinical characteristics of liver cancer complicated with depression were evaluated. Based on the inclusion and exclusion criteria, a total of 42 patients with liver cancer complicated with depression were collected. The average age is 40 y, with 6 male and 10 female individuals. The tumor staging is stage I in 2 patients, stage II in 4 patients, stage III in 18 patients and stage IV among 10 patients. 10 patients underwent surgery combined with chemotherapy and 14 patients underwent Transarterial Chemoembolization (TACE) combined with chemotherapy. Among them, 24 patients were treated with medication and psychological counselling combined with acupuncture (treatment group). Drug treatment and psychological counselling for 18 other patients (control group). There is no difference in age, tumor staging, liver cancer treatment plan and pre-treatment HADS score between the two groups (p>0.05) (Table 1).
| Variable | Control group | Treatment group | p |
|---|---|---|---|
| Age (y) | 57.389±9.648 | 55.375±10.324 | 0.097 |
| Gender | 0.151 | ||
| Male | 10 | 18 | |
| Female | 8 | 6 | |
| Stage | 0.864 | ||
| I | 2 | 3 | |
| II | 5 | 6 | |
| III | 7 | 9 | |
| IV | 4 | 6 | |
| Treatment | 0.430 | ||
| Surgery and chemotherapy | 8 | 6 | |
| TACE and chemotherapy | 10 | 18 | |
| Complications of chemotherapy | 0.582 | ||
| 1 | 0 | 0 | |
| 2 | 3 | 3 | |
| 3 | 10 | 12 | |
| 4 | 4 | 9 |
Table 1: Clinical characteristics of liver cancer patients complicated with depression
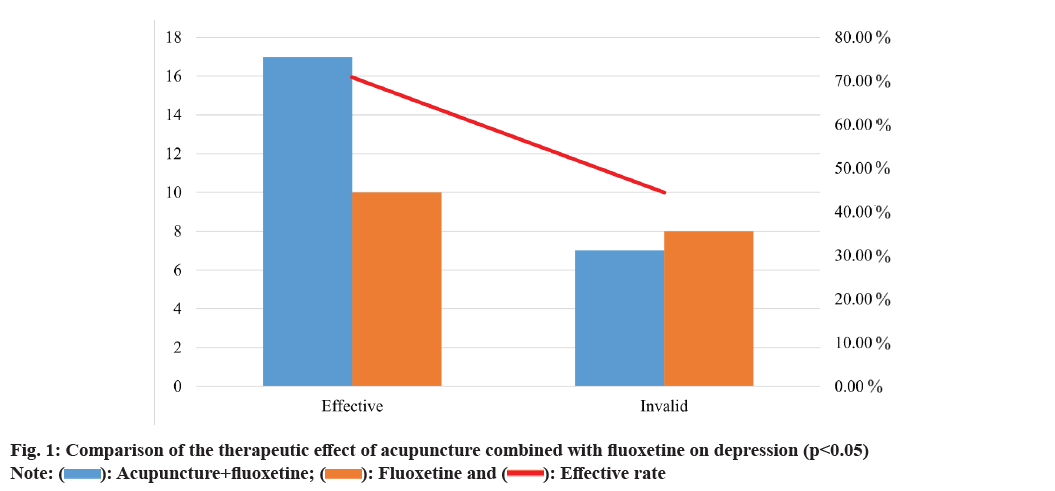
Further, acupuncture adjuvant therapy for depression in liver cancer was studied. We compared HADS scores between two groups after therapy cycles 1, 2 and 3. After one course of treatment, 10 patients were cured and 15 patients improved in the treatment group with a total effective rate of 83.3 %. In the control group, 8 patients were cured and 10 patients improved with a total effective rate of 60.0 %. After two course of treatment, 10 patients were cured and 15 patients improved in the treatment group, with a total effective rate of 83.3 %. In the control group, 8 patients were cured and 10 patients improved, with a total effective rate of 60.0 %. After three course of treatment, 10 patients were cured and 15 patients improved in the treatment group with total effective rate of 83.3 %. In the control group, 8 patients were cured and 10 patients improved with a total effective rate of 60.0 %. Cure rate of the treatment group is significantly higher than that of the control group (p<0.05) (fig. 1, Table 2 and Table 3).
| Group | 1st course HADS | 2nd course HADS | 3rd course HADS | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 0-7 | 8-10 | 11-21 | 0-7 | 8-10 | 11-21 | 0-7 | 8-10 | 11-21 | |
| Control | 4 | 5 | 9 | 7 | 3 | 9 | 7 | 3 | 8 |
| Treatment | 8 | 5 | 11 | 12 | 3 | 9 | 13 | 4 | 7 |
Table 2: Comparison of HDA scores between the two groups on 1st, 2nd and 3rd courses of treatment
| Group | n | Cure | Stabilized | Healed | Efficiency (%) |
|---|---|---|---|---|---|
| Control | 24 | 13 | 4 | 6 | 70.83 %* |
| Treatment | 18 | 7 | 3 | 8 | 44.44 % |
Note: *p<0.05 compared with the control group
Table 3: Comparison of therapeutic effects of the two groups
Effect of depression in the progression of liver cancer was studied. After three courses of treatment, we compared the relationship between the therapeutic effect (cured, stabilized and healed) of depression and the progression of liver cancer. Among patients who have been cured, stabilized and healed of depression, there were 2 patients, 1 patient and 11 patients of liver cancer progression, respectively (Table 4). Compared with healed of depression, there is a significant difference in cure and stabilized (p=0.017 and p=0.012) (fig. 2).
| n | Depression | Progressive disease | p |
|---|---|---|---|
| 20 | Cure | 2 (10 %) | 0.017 |
| 8 | Stabilized | 1 (14.29 %) | 0.012 |
| 14 | Healed | 11 (78.57 %) | 1 |
Table 4: Depression and disease progression in patients
Depression has become a commonly accompanying symptom in cancer patients, with about 8 %-24 % of cancer patients suffering from depression for a long time[5]. There is a common comorbidity between malignant tumors and depression. Cancer may lead to low mood in patients and gradually might develop symptoms related to depression, while also increasing the likelihood of depression in patients from multiple aspects[6]. Chang et al.[19] evaluated data from nearly 460 000 cancer patients in the United Kingdom from 1998 to 2020, covering 26 common cancers. The results showed that depression is the most common mental illness among cancer patients, followed by anxiety, schizophrenia, bipolar disorder and personality disorder[19]. However, the standard drug treatment for depression is not entirely satisfactory due to the adverse reactions and delayed onset[20]. At present, clinical studies have shown that acupuncture can alleviate primary depression, especially mild cases. As a separate and auxiliary treatment, it can help to manage post-stroke depression, pain related and postpartum depression[21]. It was emphasized that acupuncture combined with antidepressants not only enhanced the improvement of primary and secondary depressive symptoms, but also reduced the side effects of drug treatment[22].
In this study, we retrospectively studied the clinical characteristics of patients with depression. This study targeted depression through drug and psychological counselling combined with acupuncture. Then, we evaluated the therapeutic effect of depression through the HADS score. We found that after the treatment of drugs, psychological counselling and acupuncture, the cure rate of patients with depression was significantly higher than that of patients treated with drugs and psychological counselling. The results show that acupuncture has an effective auxiliary role in the treatment of depression.
Acupuncture can treat many diseases and is gradually recognized by the Western society, such as nausea and vomiting (including chemotherapy induced), pain (including myofascial pain, low back pain, headache, herpes zoster and pain caused by malignant tumor bone metastasis), addiction, stroke rehabilitation, menstrual cramps, fibromyalgia, osteoarthritis, carpal tunnel syndrome and asthma[23]. More and more evidence shows that acupuncture combined with medication has better efficacy and safety than medication alone in the treatment of depression[24]. In a study, 302 breast cancer patients showed that acupuncture could improve cancer related anxiety and depression[25]. Yu et al.[26] found that acupuncture can effectively alleviate the depression of patients with malignant tumor, improve their sleep, quality of life when studying depression and insomnia of patients with malignant tumor.
Han et al.[27] summarized the impact of acupuncture and electroacupuncture on cancer, they found that acupuncture and electroacupuncture can not only alleviate pain, but also alleviate cancer related complications, such as fatigue, insomnia, Coronary Artery Disease (CAD), pain, xerostomia, anxiety and depression; our results have been consistent with the reports.
The specific mechanism that acupuncture can alleviate the symptoms of depression is still unclear. Currently, it is believed to be related to genetic, neurobiological and psychosocial cultural factors. Research shows that depression is the result of environmental and genetic factors where genetic factors account for 31 %-42 % of the incidence rate[28]. The hypothesis of monoamine neurotransmitters and their receptors is a classic hypothesis in the pathogenesis of depression. In vertebrates, the deficiency of the 5-Hydroxytryptamine (5-HT) can lead to diseases such as depression, phobia, obsessive-compulsive disorder, generalized anxiety disorder and posttraumatic stress disorder. Depressed patients may exhibit a decrease in brain 5-HT and changes in 5-HT receptors, such as upregulation of 5-HT2 and downregulation of 5-HT1A receptors. Some studies have shown that electroacupuncture can regulate 5-HT receptor, restore hippocampal Cornu Ammonis (CA) 1 synaptic plasticity and thus alleviates depressive symptoms[29,30]. In addition, acupoint stimulation can also have antidepressant effects by improving 5-HT and upregulating 5-HT receptors content in synaptic gaps in brain regions[31].
Interestingly, acupuncture can improve the immunity system of cancer patients. Li et al.[32] found in the study of breast cancer that acupuncture improves immunity and fatigue after chemotherapy in breast cancer patients by inhibiting the leptin/Adenosine Monophosphate activated Protein Kinase (AMPK) signaling pathway. Liu et al.[33] believes that in immunosuppressive diseases, such as cancer, acupuncture can enhance immunity and its possible mechanism is that acupuncture enhances Natural Killer (NK) and Cluster of Differentiation (CD8+) T cell functions and restores the balance of T helper (Th) 1/ Th2, Th17/regulatory T (Treg) cells and Macrophage (M) 1/M2. In this study, we found that after the treatment of depression in cancer patients, disease progression significantly increased compared to patients who did not alleviate. This may be related to the fact that the treatment of acupuncture and moxibustion improves the patient’s immunity. However, there are studies which report that antidepressants can help improve cancer treatment. Antidepressants reduce the level of serotonin in the peripheral circulation, enhance the infiltration of tumor CD8+ T cells and slow down the growth of pancreatic and colon cancer in mice. When combined with immunotherapy, antidepressants can prevent cancer progression in the long term[34].
Drug treatment, psychological counselling and acupuncture along with moxibustion treatment can better alleviate tumor related depression and can improve tumor disease control rate.
Author’s contributions:
Wenbing Li participated in the design, performed statistical analysis and drafted the manuscript. Yin Tao, Peng Wu and Hongjie He collected clinical data, helped to draft the manuscript and performed statistical analysis. Yunji Xu conceived and designed the study and revised the manuscript. All the authors read and approved the final manuscript.
Funding:
This study was supported by the Scientific Research Project of Hunan Provincial Health Commission (Grant No: D202304017818).
Conflict of interests:
The authors declared no conflict of interests.
References
- Gilles H, Garbutt T, Landrum J. Hepatocellular carcinoma. Crit Care Nurs Clin North Am 2022;34(3):289-301.
[Crossref]
- Qin Y, Tang C, Li J, Gong J. Liver cancer in China: The analysis of mortality and burden of disease trends from 2008 to 2021. BMC Cancer 2024;24(1):1-15.
[Crossref] [Google Scholar] [PubMed]
- Iskandar AC, Rochmawati E, Wiechula R. Experiences and perspectives of suffering in cancer: A qualitative systematic review. Eur J Oncol Nurs 2021;54:1-10.
[Crossref] [Google Scholar] [PubMed]
- Niedzwiedz CL, Knifton L, Robb KA, Katikireddi SV, Smith DJ. Depression and anxiety among people living with and beyond cancer: A growing clinical and research priority. BMC Cancer 2019;19(1):1-9.
[Crossref] [Google Scholar] [PubMed]
- Depressive disorder (depression). World Health Organization (WHO); 2023.
- Wang YH, Li JQ, Shi JF, Que JY, Liu JJ, Lappin JM, et al. Depression and anxiety in relation to cancer incidence and mortality: A systematic review and meta-analysis of cohort studies. Mol Psychiatry 2020;25(7):1487-99.
[Crossref] [Google Scholar] [PubMed]
- McCarron RM, Shapiro B, Rawles J, Luo J. Depression. Ann Intern Med 2021;174(5):65-80.
[Crossref]
- Shen D, Zhao H, Gao S, Li Y, Cheng Q, Bi C, et al. Clinical serum metabolomics study on fluoxetine hydrochloride for depression. Neurosci Lett 2021;746:1-13.
[Crossref] [Google Scholar] [PubMed]
- Joo MK, Kim DH. Vagus nerve-dependent effects of fluoxetine on anxiety- and depression-like behaviors in mice. Eur J Pharmacol 2023;953:1-17.
[Crossref] [Google Scholar] [PubMed]
- Shu X, Sun Y, Sun X, Zhou Y, Bian Y, Shu Z, et al. The effect of fluoxetine on astrocyte autophagy flux and injured mitochondria clearance in a mouse model of depression. Cell Death Dis 2019;10(8):1-16.
[Crossref] [Google Scholar] [PubMed]
- Li W, Ali T, Zheng C, Liu Z, He K, Shah FA, et al. Fluoxetine regulates eEF2 activity (phosphorylation) via HDAC1 inhibitory mechanism in an LPS-induced mouse model of depression. J Neuroinflammation 2022;19(1):1-19.
[Crossref] [Google Scholar] [PubMed]
- Zhou X, Teng T, Zhang Y, Giovane CD, Furukawa TA, Weisz JR, et al. Comparative efficacy and acceptability of antidepressants, psychotherapies, and their combination for acute treatment of children and adolescents with depressive disorder: A systematic review and network meta-analysis. Lancet Psychiatry 2020;7(7):581-601.
[Crossref] [Google Scholar] [PubMed]
- Robinson N, Lorenc A, Ding W, Jia J, Bovey M, Wang XM. Exploring practice characteristics and research priorities of practitioners of traditional acupuncture in China and the EU-A survey. J Ethnopharmacol 2012;140(3):604-13.
[Crossref] [Google Scholar] [PubMed]
- Yang NN, Lin LL, Li YJ, Li HP, Cao Y, Tan CX, et al. Potential mechanisms and clinical effectiveness of acupuncture in depression. Curr Neuropharmacol 2022;20(4):738-50.
[Crossref] [Google Scholar] [PubMed]
- Hou Z, Yu X, Chen J, Brenner JS, Sun Z, Shang H. Does acupuncture have advantages in the rehabilitation of vascular mild cognitive impairment? A systematic review and meta-analysis. Heliyon 2023;9(8):1-18.
[Crossref] [Google Scholar] [PubMed]
- Chan YY, Lo WY, Yang SN, Chen YH, Lin JG. The benefit of combined acupuncture and antidepressant medication for depression: A systematic review and meta-analysis. J Affect Disord 2015;176:106-17.
[Crossref] [Google Scholar] [PubMed]
- Posar A, Visconti P. Autism spectrum disorder and the Diagnostic and Statistical Manual of mental disorders-Fifth edition (DSM-5): The experience of 10 y. Turk Arch Pediatr 2023;58(6):658-9.
[Crossref] [Google Scholar] [PubMed]
- Sivertsen HE, Helvik AS, Gjøra L, Haugan G. Psychometric validation of the Hospital Anxiety and Depression Scale (HADS) in community-dwelling older adults. BMC Psychiatry 2023;23(1):1-9.
[Crossref] [Google Scholar] [PubMed]
- Chang WH, Lai AG. Cumulative burden of psychiatric disorders and self-harm across 26 adult cancers. Nat Med 2022;28(4):860-70.
[Crossref] [Google Scholar] [PubMed]
- Jha MK, Mathew SJ. Pharmacotherapies for treatment-resistant depression: How antipsychotics fit in the rapidly evolving therapeutic landscape. Am J Psychiatry 2023;180(3):190-9.
[Crossref] [Google Scholar] [PubMed]
- Armour M, Smith CA, Wang LQ, Naidoo D, Yang GY, MacPherson H, et al. Acupuncture for depression: A systematic review and meta-analysis. J Clin Med 2019;8(8):1-11.
[Crossref] [Google Scholar] [PubMed]
- Armour M, Smith CA, Wang LQ, Naidoo D, Yang GY, MacPherson H, et al. Acupuncture for depression: A systematic review and meta-analysis. J Clin Med 2019;8(8):1-22.
[Crossref] [Google Scholar] [PubMed]
- Zhuang Y, Xing JJ, Li J, Zeng BY, Liang FR. History of acupuncture research. Int Rev Neurobiol 2013;111:1-23.
[Crossref] [Google Scholar] [PubMed]
- Zhang Z, Li S, Meng H, Wang Y, Zhang Y, Wu M, et al. Efficacy and safety of acupuncture in the treatment of depression: A systematic review of clinical research. Anat Rec 2021;304(11):2436-53.
[Crossref] [Google Scholar] [PubMed]
- Greenlee H, DuPont‐Reyes MJ, Balneaves LG, Carlson LE, Cohen MR, Deng G, et al. Clinical practice guidelines on the evidence-based use of integrative therapies during and after breast cancer treatment. CA Cancer J Clin 2017;67(3):194-232.
[Crossref] [Google Scholar] [PubMed]
- Yu FE, Wang XY, Li SD, Zhang Y, Wang HM, Min LI, et al. Clinical research of acupuncture on malignant tumor patients for improving depression and sleep quality. J Tradit Chin Med 2011;31(3):199-202.
[Crossref] [Google Scholar] [PubMed]
- Han QQ, Fu Y, Le JM, Ma YJ, Wei XD, Ji HL, et al. The therapeutic effects of acupuncture and electroacupuncture on cancer-related symptoms and side-effects. J Cancer 2021;12(23):7003-9.
[Crossref] [Google Scholar] [PubMed]
- Alshaya DS. Genetic and epigenetic factors associated with depression: An updated overview. Saudi J Biol Sci. 2022;29(8):103311.
[Crossref] [Google Scholar] [PubMed]
- Han X, Wu H, Yin P, Chen Z, Cao X, Duan Y, et al. Electroacupuncture restores hippocampal synaptic plasticity via modulation of 5-HT receptors in a rat model of depression. Brain Res Bull 2018;139:256-62.
[Crossref] [Google Scholar] [PubMed]
- Chen L, Yao Z, Qu S, Zhang J, Zhang J, Zhang Z, et al. Electroacupuncture improves synaptic plasticity by regulating the 5-HT1A receptor in hippocampus of rats with chronic unpredictable mild stress. J Int Med Res 2020;48(5):1-13.
[Crossref] [Google Scholar] [PubMed]
- Duan D, Tu Y, Yang X, Liu P. Electroacupuncture restores 5-HT system deficit in chronic mild stress-induced depressed rats. Evid Based Complement Alternat Med 2016;2016:1-17.
[Crossref] [Google Scholar] [PubMed]
- Li J, Fu R, Guo X, Pan Z, Xie J. Acupuncture improves immunity and fatigue after chemotherapy in breast cancer patients by inhibiting the leptin/AMPK signaling pathway. Support Care Cancer 2023;31(9):1-10.
[Crossref] [Google Scholar] [PubMed]
- Liu F, Wang Y, Lyu K, Du X, Zhou M, Shi J, et al. Acupuncture and its ability to restore and maintain immune homeostasis. QJM 2024;117(3):167-76.
[Crossref] [Google Scholar] [PubMed]
- Schneider MA, Heeb L, Beffinger MM, Pantelyushin S, Linecker M, Roth L, et al. Attenuation of peripheral serotonin inhibits tumor growth and enhances immune checkpoint blockade therapy in murine tumor models. Sci Transl Med 2021;13(611):1-18.
[Crossref] [Google Scholar] [PubMed]
 ): Acupuncture+fluoxetine; (
): Acupuncture+fluoxetine; (  ): Fluoxetine and (
): Fluoxetine and ( ): Effective rate
): Effective rate 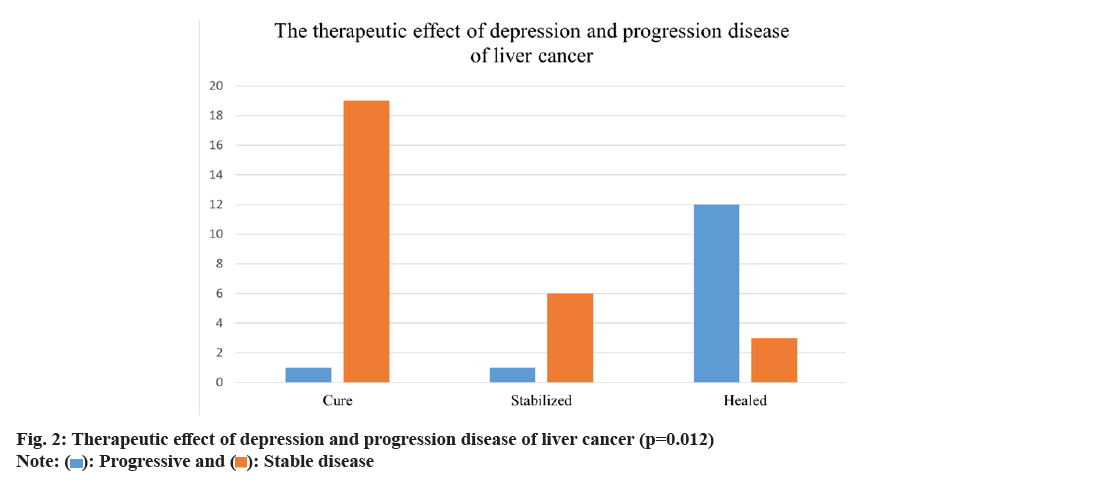
 ): Progressive and (
): Progressive and (  ): Stable disease
): Stable disease 



