- *Corresponding Author:
- Y. Lu
Anesthesiology Department, Second Hospital, Tianjin Medical University, Tianjin 300211, China
E-mail: luyuechun_tianjin@126.com
| This article was originally published in a special issue, "Clinical and Experimental Studies on Drug and Intervention Repurposing in China |
| Indian J Pharm Sci 2019:81(4)spl issue1;138-144 |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
In order to study the effects of propofol and sevoflurane on postoperative delirium in patients with malignant tumors, elderly patients who suffered from malignant tumors were selected as the research subjects and were divided into the propofol group and the sevoflurane group, who were induced anesthesia with Propofol and sevoflurane, respectively before surgery to observe the bispectral index, mean arterial pressure and heart rate of each patient before anesthesia, during the surgery, and in the recovery period. In addition, the mini-mental state examination was utilized to evaluate the mental status of patients, the confusion assessment model for intensive care unit was utilized to evaluate the conditions of postoperative delirium of patients, the Prince-Henry pain scale was utilized to evaluate the degree of postoperative pain of patients, and the enzyme-linked immunosorbent assay was utilized to detect the protein concentrations of NSE, S100β, and IL-2 of patients. The results showed that the bispectral index, mean arterial pressure and heart rate of patients decreased significantly during the surgery compared to those values before anesthesia, in both groups of patients(p<0.05); however, the inter-group differences in the bispectral index, mean arterial pressure and heart rate between the propofol group and the sevoflurane group were not statistically significant. In terms of the mini-mental state examination results of patients in the propofol group and the sevoflurane group, those obtained on the postoperative d 3 and postoperative d 5 were lower than those obtained on the preoperative 1d, and the differences were statistically significant (p<0.05); however, the inter-group differences of the mini-mental state examination results between the propofol group and the sevoflurane group were not statistically significant. In terms of the incidence rates of postoperative delirium in patients in the propofol group and the sevoflurane group, those on the postoperative d 3 were relatively higher, and the differences were statistically significant (p<0.05); however, the inter-group differences of the postoperative delirium incidence rates between the propofol group and the sevoflurane group were not statistically significant. In terms of the Prince-Henry pain scale results of patients in the propofol group and the sevoflurane group, respectively on postoperative d 1, 2, and 3, the intra-group differences were also not statistically significant, and the inter-group differences were not statistically significant. In terms of the ELISA results of the NSE, S100β, and IL-2 protein concentrations of patients in the propofol group and the sevoflurane group, the NSE and S100β protein concentrations were significantly increased on the postoperative d 1, 2 and 3 compared with those at preoperative 10 min (p<0.05); the IL-2 protein concentrations were not different between the preoperative 10 min and the postoperative d 1, 2 and 3 and the inter-group differences were also not significant. Anesthesia inductions with propofol or sevoflurane had influence on postoperative delirium of patients undergoing surgical treatment for malignant tumors.
Keywords
Propofol, sevoflurane, malignant tumour, postoperative delirium, anaesthesia
Postoperative delirium (POD) refers to the condition of delirium after operations and surgeries, which is a common complication of anaesthesia[1]. POD often occurs within 5 d after surgeries. The risk factors of POD include predisposing factors such as advanced age, visual disorder, hearing impairment, mental disorder, hepatic dysfunction, renal dysfunction, dehydration, Parkinson’s disease and alcohol abuse, as well as precipitating factors such as malnutrition, hypoxia, retained muscular relaxants, acute urinary retention, indwelling urethral catheter, transfusion reactions, or severe drug reactions[2,3]. A study found that the incidence rate of POD was about 10 to 50 % in elderly patients over 65 y[4]. POD is characterized by acute onset and fluctuating disease progression and is divided into 3 subtypes, the high activity type, the low activity type, and the mixed type[5]. Of all the subtypes, the high activity type is also called the agitation type, and its clinical manifestations are obviously agitated behaviours, multilingualism, delusion, and aggressive behaviours; the low activity type is also called the quiet type, and its clinical manifestations are silence, slow responses, drowsiness, listlessness, and cognitive separation; the mixed type has the manifestations of the former 2 subtypes alternatively. POD is an exclusionary diagnosis that has no sequela[6-8]. However, POD can lead to increased heart rate (HR), elevated blood pressure, wound bleeding, and prolonged postoperative recovery period. It also increases the incidence rates of postoperative pulmonary infection, bedsores, and venous thrombosis, which brings heavy burdens to both hospitals and families[9,10].
Malignant tumours are common in elderly patients and are also the major cause of death[11]. At present, the main treatment methods are surgery, radiation therapy, and chemical cytotoxic therapy, of which surgical treatment is the oldest and most effective treatment[12]. Surgical treatment is not limited by biological characteristics, and there is no potential carcinogenic risk, which can effectively cure most undistributed tumours[13]. However, during the surgeries, the operative process is relatively complicated, the time required is long, the scope is wide, and the stress responses of patients are huge. Therefore, general anaesthesia is usually required in surgical treatments of tumours[14]. Propofol and sevoflurane are the most commonly used intravenous and inhaled anaesthetics, which can be used for the induction and maintenance of general anaesthesia[15]. Propofol is usually used together with epidural or spinal anaesthesia. It is also often used with muscle relaxants, analgesics, or inhaled anaesthetics. The adverse reactions are mild excitability and local pain[16,17]. Sevoflurane is usually mixed with oxygen or oxygen and nitrous oxide. The adverse reactions are malignant hyperthermia, rhabdomyolysis, shock, and allergy-like symptoms[18]. In summary, studies on the effects of propofol and sevoflurane on malignant tumour surgeries are relatively rare. Therefore, taking elderly patients with malignant tumors as research subjects, the effects of propofol and sevoflurane on POD in patients with malignant tumours were explored, providing a reference for clinical anaesthesia medication.
A total of 120 elderly patients with malignant tumours who were 65-85 y old treated in a hospital (from January to July 2018) were selected as the research subjects, with an average age of 75.32 y. All patients were randomly divided into the propofol group (60 patients) and the sevoflurane group (60 patients). In the propofol group, there were 26 males and 24 females, aged 66-85 y, with an average age of 74.76 y. In the sevoflurane group, there were 24 males and 26 females, aged 65-87 y, with an average age of 75.88 y. All general information of patients in both groups, such as age, gender, and admission time, was not significantly different; thus, the experiment was of comparability. The experimental protocol received approval of the ethics committee of the hospital. Inclusion criteria were, all patients included in the experiment should be older than 65 y; patients who received surgical treatments of tumours with general anaesthesia, and the surgeries lasted for more than 2 h; patients who could communicate well with the medical personnel, and were of good clinical compliance; patients who had complete clinical data; patients who signed the informed consent forms. Exclusion criteria were patients who suffered from severe hepatic or renal dysfunctions; patients who suffered from cognitive function impairment or mental diseases; patients who suffered from severe tumours; patients who received craniocerebral operations; patients whose preoperative ASA≥grade IV.
All patients should not take preanesthetic drugs and fast for 12 h before surgery; in addition, water was banned for 6 h before surgery. Before anaesthesia induction, patients inhaled oxygen for 5 min with an oxygen flow rate of 5 l/min. Then, patients were given sufentanil (0.3-0.6 μg/kg, Yichang Renfu Pharmaceutical Co., Ltd., Chin), cis-atracurium (0.1~0.2 mg/kg, Shanghai Hengrui Pharmaceutical Co., Ltd., China), and propofol (0.5~1.0 mg/kg, Sichuan Guorui Pharmaceutical Co., Ltd., China) through intravenous injections. Patients in the propofol group continued to receive propofol injections intravenously and were added with sufentanil and cis-atracurium regularly to maintain anaesthesia. Patients in the sevoflurane group continued to inhale sevoflurane and were added with sufentanil and cisatracurium regularly to maintain anaesthesia. The concentrations and rates of anaesthetics of patients in both groups were regulated to maintain the bispectral index (BIS) being in the range of 40-60; in addition, blood transfusion was given to patients to maintain the haemoglobin being in the range of 7-10 g/dl. The mean arterial pressure (MAP) of each patient was monitored and was maintained at ±20 % of the baseline value; meanwhile, the HR of each patient was maintained fluctuating in the range of 60-100 beats/min. The values of BIS, MAP, and HR of patients before anaesthesia, during the surgeries and in the recovery period were recorded. The anaesthesia was terminated after the suture was completed. Within the 2 d after the surgeries, patients received the patient-controlled intravenous analgesia (PCIA) and intravenous injections of sufentanil (1.3 μg/kg, sufentanil was diluted to 100 ml with saline), with a single dosage of 2 ml and the injection rate of 2 ml/h.
The mini-mental state examination (MMSE) is a dementia screening scale that comprehensively, accurately, and rapidly reflects the mental state of the subject and the degree of cognitive impairment. MMSE evaluates the time-orientation ability, location-orientation ability, immediate memory, attention and computational ability, delayed memory, language skills, and visual space. MMSE has a total of 30 questions, with 1 point for each question. The standards of normal boundary values are as follows: illiterate >17 points, primary school >20 points, junior high school and above >24 points. On preoperative d 1 and postoperative d 3 and 5, the MMSE was utilized to evaluate the mental states of patients.
The confusion assessment model for intensive care unit (CAM-ICU) is a scale that evaluates the state of consciousness of ICU patients, which can be used to observe POD in patients. First, the level of consciousness was assessed. The evaluation criteria are as follows: 4 points for aggressive behaviours; 3 points for extreme agitation; 2 points for agitation; 1 point for irritability; 0 points for clear-headed and quiet; -1 point for drowsiness; -2 points for mild sedation; -3 points for moderate sedation; -4 points for deep sedation; -5 points for impossibility of being wakened. If a patient got <-3 points, the evaluation was stopped and was continues once the patient regained consciousness. If a patient got ≤-3 points, the evaluation of the consciousness of patients was carried out by the criteria of acute changes or fluctuations in consciousness, attention disorders, changes in consciousness levels, and confusion of thinking. If the patient had acute changes or fluctuations in consciousness, attention disorder, and altered levels of consciousness, the CAM-ICU would be positive. Other manifestations were considered CAM-ICU negative. A positive CAM-ICU overall evaluation of the patient indicated the presence of delirium, and a negative CAM-ICU overall evaluation of the patient indicated the absence of delirium. Respectively on preoperative 1 d and postoperative 3 and 5 d, the CAM-ICU was utilized to evaluate the POD conditions of patients.
The Prince-Henry pain scale (PHPS) was used to evaluate the degree of postoperative pain of patients. The PHPS is divided into 5 levels and the grading criteria are as follows: no pain occurs when coughing, 0 points; pain occurs when coughing, 1 point; pain occurs when breathing deeply, no pain occurs in a quiet state, 2 points; pain occurs at rest, the degree of pain is light and is tolerable, 3 points; severe pain occurs at rest and is unbearable, 4 points. The degree of postoperative pain was evaluated respectively on postoperative d 1, 2 and 3.
At preoperative 10 min, postoperative d 1, 2 and 3, 5 ml of venous blood samples were drawn from the upper limbs of patients, centrifuged for 5 min (5000 rpm) in a centrifuge and the upper plasma was stored in a -80° refrigerator. The protein concentrations of NSE, S100β, and IL-2 were detected by ELISA using an ELISA kit (Beijing Jiehui Bogao Biotechnology Co., Ltd., China).
In this study, the SPSS 22.0 statistics software was used for statistical analysis of the data; all quantitative data were submitted to normal distribution test and homogeneity test of variance and were expressed as the mean±standard deviation (SD). The one-way ANOVA was used for comparison between groups; if the normal distribution and variance were consistent, the LSD method was used; otherwise, the SNK-q test was used. Pearson correlation analysis was used to analyse the correlations between two parameters, p<0.05 indicated the statistical significance of the difference.
The comparative results of BIS value, MAP and HR between the propofol group and the sevoflurane group were shown in Table 1. As shown in Table 1, the BIS value, MAP, and HR of patients in the propofol and the sevoflurane group significantly decreased during the surgeries compared to those before anesthesia (p<0.05). However, the inter-group differences of BIS value, MAP, and HR between the propofol and the sevoflurane group were not significantly different.
| Groups | Indicators | Before anaesthesia | During the surgeries | Recovery period |
|---|---|---|---|---|
| The propofol group | BIS value | 101±1 | 52±3 | 100±2 |
| MAP (mmHg) | 82±4 | 69±6 | 80±5 | |
| HR (times/min) | 80±5 | 65±7 | 81±6 | |
| The sevoflurane group | BIS value | 100±1 | 51±3 | 99±2 |
Table 1: BIS value, MAP, and HR in the propofol group and the sevoflurane group
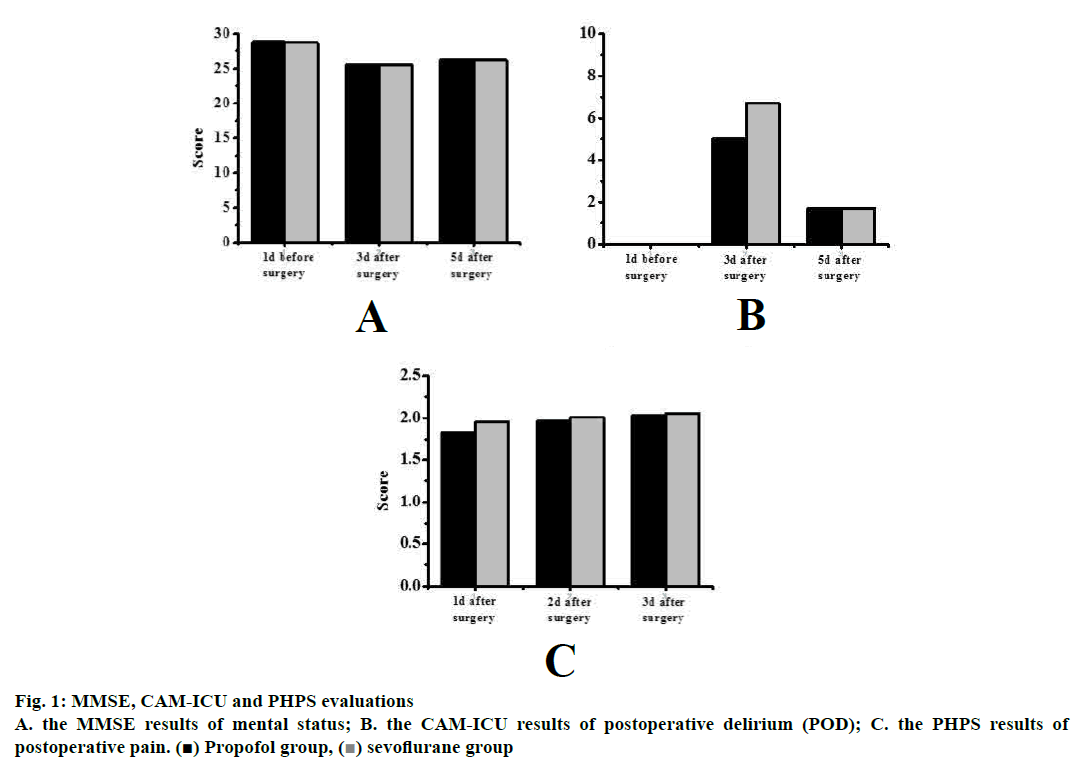
The MMSE results of the mental states of the patients were shown fig. 1A. As shown in fig. 1A, in the propofol group, the MMSE results were 28.9±0.5, 25.5±0.3 and 25.3±0.5 points on preoperative d 1, postoperative 3 and 5, respectively, indicating that the MMSE results of patients in the propofol group on postoperative d 3 and 5 were significantly lower than those obtained on preoperative d 1 (p<0.05). In the sevoflurane group, the MMSE results were 28.7±0.6, 25.6±0.4 and 26.2± 0.5 points on preoperative d 1, postoperative d 3 and 5, indicating that the MMSE values of patients in the sevoflurane group on postoperative d 3 and 5 were significantly lower than those obtained on preoperative d 1 (p<0.05). However, the inter-group differences of the MMSE values between the propofol and the sevoflurane group were not significantly different (p>0.05).
The CAM-ICU results of the POD conditions of the patients were shown in fig. 1B. No patients in the propofol and the sevoflurane groups developed POD. In the propofol group, 3 patients developed POD on postoperative d 3 and the incidence rate of POD was 5.0 %. In the sevoflurane group, 4 patients developed POD on postoperative 3 d, and the incidence rate of POD was 6.7 %. In the propofol group, 1 patient developed POD on postoperative d 5 and the incidence rate of POD was 1.7 %. In the sevoflurane group, 1 patient developed POD on postoperative d 5 and the incidence rate of POD was 1.7 %. It could be concluded that compared to postoperative d 5, the incidence rates of POD on postoperative d 3 were significantly higher (p<0.05). However, the inter-group differences of the POD incidence rates between the propofol group and the sevoflurane group were not significant.
The PHPS results of postoperative pain of patients were shown fig. 1C. As shown in fig. 1C, on postoperative d 1, 2, and 3, the PHPS results of patients in the propofol group were 1.83±0.11, 1.96±0.14 and 2.03±0.19 points, respectively and the differences were not statistically significant. On postoperative d 1, 2 and 3, the PHPS results of patients in the sevoflurane group were, 1.95±0.14, 2.01±0.17 and 2.06±0.24 points, respectively and the differences were not statistically significant; in addition the inter-group differences of PHPS results between the propofol group and the sevoflurane group were not significant.
The ELISA results of NSE, S100β and IL-2 protein concentrations of patients were shown in fig. 2. In the propofol group, compared with preoperative 10 min, the NSE protein concentrations on postoperative d 1, 2 and 3 were significantly increased (p<0.05); compared to the level at preoperative 10 min, the S100β protein concentrations on postoperative d 1, 2 and 3 were significantly increased (p<0.05); however, the differences between IL-2 concentrations at preoperative 10 min and postoperative d 1, 2 and 3 were not significantly different. In the sevoflurane group, compared to preoperative 10 min, the NSE protein concentrations on postoperative d 1, 2 and 3 were also significantly increased (p<0.05); compared to preoperative 10 min, the S100β protein concentrations on postoperative d 1, 2 and 3 were significantly increased (p<0.05); however, the differences between IL-2 levels at preoperative 10 min and on the postoperative d 1, 2 and 3 were not statistically significant. However, the inter-group differences of NSE, S100β, and IL-2 protein concentrations between the propofol and the sevoflurane group were not significantly different (p>0.05).
The effects of propofol and sevoflurane on POD in patients with malignant tumours were explored. The elderly patients who suffered from malignant tumours were selected as the research subjects and were divided into the propofol group and the sevoflurane group, who received anaesthesia induction with propofol and sevoflurane, respectively before their surgeries to observe the BIS, MAP and HR of each patient before anaesthesia, during surgery and in the recovery period. In addition, the MMSE was utilized to evaluate the mental status of patients, the CAMICU was utilized to evaluate the conditions of POD in patients, the PHPS was utilized to evaluate the degree of postoperative pain of patients, and the ELISA assays were utilized to detect the concentrations of NSE, S100β, and IL-2 of patients. The results showed that the BIS value, MAP and HR of patients in the propofol and the sevoflurane group decreased significantly during surgery compared to those before anaesthesia (p<0.05); however, the inter-group differences of BIS, MAP and HR between the propofol and the sevoflurane groups were not statistically significant. The MMSE results of patients in the propofol group and the sevoflurane group obtained on the postoperative d 3 and 5 were significantly lower than those obtained on the preoperative d 1 (p<0.05); however, the inter-group differences of the MMSE results between the propofol group and the sevoflurane group were not significant (p>0.05). The incidence rates of POD in patients in the propofol group and the sevoflurane group on the postoperative d 3 were significantly higher (p<0.05); however, the inter-group differences in the POD incidence rates between the propofol group and the sevoflurane group were not statistically significant. The PHPS results of patients in the propofol group and the sevoflurane group on postoperative d 1, 2 and 3 were not significantly different as well as the inter-group differences. The ELISA results of the NSE, S100β, and IL-2 protein concentrations of patients in the propofol group and the sevoflurane group were compared it was observed that the NSE and S100β protein levels were significantly increased on the postoperative d 1, 2 and 3 compared to those at preoperative 10 min (p<0.05); the IL-2 protein concentrations were not changed between the preoperative 10 min and the postoperative d 1, 2, and 3 as well as the inter-group level differences were also not significant. Thus, in terms of the surgical treatments for patients with malignant tumours, the anaesthesia induction by propofol and sevoflurane had no obvious differences in the effects on POD. However, certain deficiencies were identified in this study; for example, the data collection of samples was relatively less that caused the result being biased to a certain extent. Therefore, the data capacity would be further increased in the subsequent studies to reach more valuable conclusions.
References
- Lee C, Lee CH, Lee G, Lee M, Hwang J. The effect of the timing and dose of dexmedetomidine on postoperative delirium in elderly patients after laparoscopic major non-cardiac surgery: A double blind randomized controlled study. J Clin Anesth 2018;47:27-32.
- Kant IMJ, de Bresser J, van Montfort SJT, Slooter AJC, Hendrikse J. MRI Markers of Neurodegenerative and Neurovascular Changes in Relation to Postoperative Delirium and Postoperative Cognitive Decline. Am J Geriatr Psychiatry 2017;25(10):1048.
- Choi NY, Kim EH, Baek CH, Sohn I, Yeon S, Chung MK, et al. Development of a nomogram for predicting the probability of postoperative delirium in patients undergoing free flap reconstruction for head and neck cancer. Eur J Surg Oncol 2017;43(4):683-8.
- Nadler JW, Evans JL, Fang E, Preud'Homme XA, Daughtry RL, Chapman JB, et al. A randomised trial of peri?operative positive airway pressure for postoperative delirium in patients at risk for obstructive sleep apnoea after regional anaesthesia with sedation or general anaesthesia for joint arthroplasty. Anaesthesia 2017;72(6):729-36.
- Tanaka P, Goodman S, Sommer BR, Maloney W, Huddleston J, Lemmens HJ, et al. The effect of desflurane versus propofol anesthesia on postoperative delirium in elderly obese patients undergoing total knee replacement: A randomized, controlled, double-blinded clinical trial. J Clin Anesth 2017;61(4):17-22.
- Lingehall HC, Smulter NS, Lindahl E, Lindkvist M, Engström KG, Gustafson YG, et al. Preoperative Cognitive Performance and Postoperative Delirium Are Independently Associated with Future Dementia in Older People Who Have Undergone Cardiac Surgery: A Longitudinal Cohort Study. Crit Care Med 2017;45(8):1.
- Deiner S, Luo X, Lin HM, Sessler DI, Saager L, Sieber FE, et al. Intraoperative Infusion of Dexmedetomidine for Prevention of Postoperative Delirium and Cognitive Dysfunction in Elderly Patients Undergoing Major Elective Noncardiac Surgery: A Randomized Clinical Trial. JAMA Surg 2017;152(8):e171505.
- Susheela AT, Packiasabapathy S, Gasangwa DV, Patxot M, O'Neal J, Marcantonio E, et al. The use of dexmedetomidine and intravenous acetaminophen for the prevention of postoperative delirium in cardiac surgery patients over 60 years of age: a pilot study. F1000Res 2017;6:1842.
- Avidan MS, Maybrier HR, Abdallah AB, Jacobsohn E, Vlisides PE, Pryor KO, et al. Intraoperative ketamine for prevention of postoperative delirium or pain after major surgery in older adults: an international, multicentre, double-blind, randomised clinical trial. Lancet 2017;390(10091):267.
- Tobar E, Abedrapo MA, Godoy JA, Llanos JL, Díaz MJ, Azolas R, et al. Impact of hypotension and global hypoperfusion in postoperative delirium: a pilot study in older adults undergoing open colon surgery. Rev Bras Anestesiol 2018;68(2):135.
- Puerta-GarciaSandoval P, Lizaur-Utrilla A, Trigueros-Rentero MA, Lopez-Prats FA. Mid- to long-term results of allograft–prosthesis composite reconstruction after removal of a distal femoral malignant tumor are comparable to those of the proximal tibia. Knee Surg Sports Traumatol Arthrosc 2018;27(7):1-8.
- Clermonts SHEM, van Loon YT, Schiphorst AHW, Wasowicz DK, Zimmerman DDE. Transanal minimally invasive surgery for rectal polyps and selected malignant tumors: caution concerning intermediate-term functional results. Int J Colorectal Dis 2017;32(12):1-9.
- Devnani B, Biswas A, Bakhshi S, Khan SA, Mridha AR, Agarwal S. Primary Intraosseous Malignant Peripheral Nerve Sheath Tumor of Metacarpal Bones of the Hand in a Patient Without Neurofibromatosis 1: Report of a Rare Case. Indian J Med Paediatr Oncol 2017;38(2):232-5.
- Abu Arja MH, Patel P, Shah SH, Auletta JJ, Meyer EK, Conley SE, et al. Synchronous Central Nervous System Atypical Teratoid/Rhabdoid Tumor and Malignant Rhabdoid Tumor of the Kidney: Case Report of a Long-Term Survivor and Review of the Literature. World Neurosurg 2018;111:6-15.
- Deng F, Wang S, Zhang L, Xie X, Cai S, Li H, et al. Propofol Through Upregulating Caveolin-3 Attenuates Post-Hypoxic Mitochondrial Damage and Cell Death in H9C2 Cardiomyocytes During Hyperglycemia. Cell Physiol Biochem 2017;44(1):279.
- Jerath A, Panckhurst J, Parotto M, Lightfoot N, Wasowicz M, Ferguson ND, et al. Safety and Efficacy of Volatile Anesthetic Agents Compared With Standard Intravenous Midazolam/Propofol Sedation in Ventilated Critical Care Patients: A Meta-analysis and Systematic Review of Prospective Trials. Anesth Analg 2017;124(4):1190.
- Cascella M, Fusco R, Caliendo D, Granata V, Carbone D, Muzio MR, et al. Anesthetic dreaming, anesthesia awareness and patient satisfaction after deep sedation with propofol target controlled infusion: A prospective cohort study of patients undergoing day case breast surgery. Oncotarget 2017;8(45):79248-56.
- Lu X, Lv S, Mi Y, Wang L, Wang G. Neuroprotective effect of miR-665 against sevoflurane anesthesia-induced cognitive dysfunction in rats through PI3K/Akt signaling pathway by targeting insulin-like growth factor 2. Am J Transl Res 2017;9(3):1344.
 ) Propofol group, (
) Propofol group, ( ) sevoflurane group
) sevoflurane group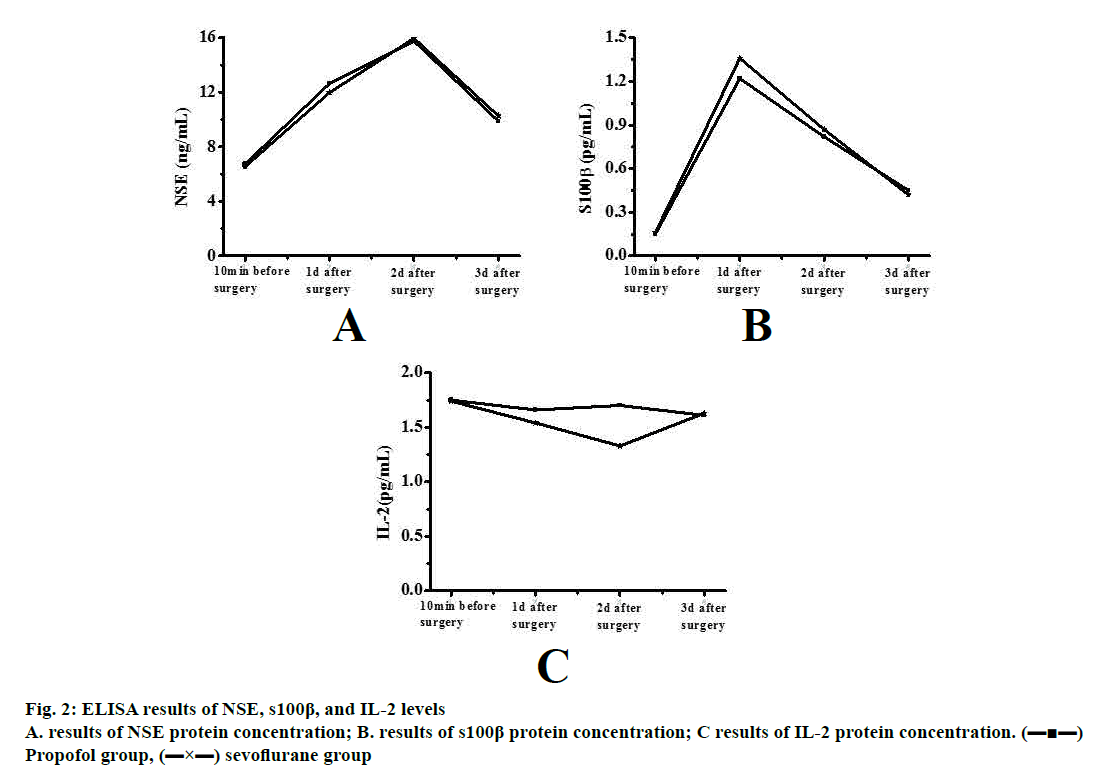
 ) Propofol group, (
) Propofol group, ( ) sevoflurane group
) sevoflurane group



