- *Corresponding Author:
- Weifeng Liu
Department of Anesthesiology, Nanfang Hospital, Southern Medical University, Guangzhou 516006, China
E-mail: sglwfeng01@21cn.com
| This article was originally published in a special issue,“Clinical Advancements in Life Sciences and Pharmaceutical Research” |
| Indian J Pharm Sci 2024:86(5) Spl Issue “60-66” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
The present study sets out to analyze the effective dose of remimazolam tosilate combined with nalbuphine in inhibiting somatic motor reflexes during induced abortion. From September 2022 to June 2023, individuals with induced abortion were selected. After intravenous injection of nalbuphine for 3 min and administration of remimazolam, the procedure was performed. Vital signs such as mean arterial pressure and heart rate were observed at different time points, before anesthesia induction (T0), after nalbuphine injection (T1), after remimazolam injection (T2), at the end of surgery (T3) and at the time of recovery from anesthesia (T4). The dosage of remimazolam, operation duration, recovery time and adverse reactions like uterine contraction pain, dizziness, hypoxemia, bradycardia, nausea and vomiting were recorded. Mean effective dose and 95 % effective dose of remimazolam+nalbuphine in induced abortion were tested using the Efron’s biased coin design method. Dose of 0.015 mg/kg nalbuphine, depicted effective dose and 95 % effective dose remimazolam in inhibiting the somatic motor reflexes during induced abortion which was found to be 0.439 mg/kg (95 % CI: 0.375-0.543 ) and 0.570 mg/kg (95 % CI: 0.500-1.533), respectively. Mean remimazolam dosage in patients was (22.21±5.02) mg with operation duration of (5.70±1.78) min and recovery time of (3.67±1.15) min. The major adverse reactions were hypoxemia, uterine contraction pain and dizziness. The above results indicated that the effective dose and 95 % effective dose of remimazolam in inhibiting the patients’ somatic motor reflexes were 0.439 mg/kg (95 % CI: 0.375-0.543 mg/kg) and 0.570 mg/kg (95 % CI: 0.500-1.533 mg/kg), respectively and the combination of them was safe in induced abortion.
Keywords
Remimazolam tosilate, nalbuphine, abortion, somatic motor reflexes
With the popularization of comfort medicine, painless induced abortion has become a common clinical option for termination of pregnancy[1,2]. Although the procedure is short in duration, it is highly anesthetic, demanding, requiring fast onset of anesthesia, good analgesic effects, quick recovery after surgery, complete consciousness when the patient leaves the hospital with no anesthetic residue and post-surgical effects[3-5]. At present, the common anesthetic choice in clinical practice is propofol combined with opioids. However, propofol itself has no or only weak analgesic effect, which often requires large dose when used alone, causing adverse reactions such as respiratory depression and circulation instability[6,7]. Therefore, it is necessary to optimize the selection of anesthesia strategies for patients undergoing induced abortion to provide them with safer and more reliable anesthesia options.
Remimazolam (RMZ) tosilate which is a Gamma Aminobutyric Acid (GABAA) receptor agonist and new benzodiazepine drug, with ultra-short-acting sedative and anesthetic effects[8]. Its advantages include quick onset of time, short maintenance and recovery time having no adverse reactions such as severe hypotension and respiratory depression, etc., in addition of having the ability to be rapidly antagonized by flumazenil within 30 s-1 min, with higher safety[9,10]. Moreover, RMZ can be metabolized by nonspecific esterases, independent of liver and kidney function whose metabolites have no pharmacological activity, further demonstrating its safety[11,12]. Nalbuphine (Nal) is an opioid agonist and antagonist, primarily acting on Kappa (κ) 1 at the spinal level and κ3 receptor at the supraspinal level[13]. Nal, as a partial antagonist of the Mu (μ) receptor, can avoid a series of adverse reactions such as respiratory depression, addiction, euphoria, bradycardia, itching, immunosuppression, nausea, vomiting, intestinal peristalsis disorders and decreased bladder muscle function, etc., associated with μ receptor activation[14,15]. As a complete agonist of the κ receptor, it can exert quick-onset, strong and lasting analgesic effects[16]. Furthermore, Nal has very weak activity against Delta (δ) receptor, thus helping patients avoid effects like irritability and anxiety related to the enhanced δ receptor activity[17]. Currently, there is no related research on RMZ used in induced abortion and its optimal dosage remains to be unclear. Therefore, this study mainly explores the effective dosage of Nal combined with RMZ in inhibiting somatic motor reflexes in induced abortion.
Materials and Methods
General information:
Approved by the hospital’s ethics committee, this study included 33 individuals who underwent painless induced abortion from September 2022 to June 2023 at our hospital. After intravenous injection of different doses of Nal for 3 min, bolus injection of RMZ, Ramsay score of 5 points and an Observer’s Assessment of Alertness/Sedation (OAA/S) scale score of 1 point, the operation was started.
Criteria for patient enrollment:
Inclusion criteria: Patients of age between (18- 45) y; patients having Body Mass Index (BMI) of 20-25 kg/m2; patients underlying the guidelines of America Society of Anesthesiologist (ASA) grading ? or ?; patients whose duration of menopause is 60 d; patients following no medication or surgical contraindications; patients having no serious underlying diseases and patients of fetal age, ≤10 w .
Exclusion criteria: Patients with Systolic (S) BP Systolic (S) BP ≥160 mmHg; individuals with Diastolic (D) BP ≥110 mmHg and Heart Rate (HR) ≥120 beats/min; individuals having the history of allergic reaction to benzodiazepines; individuals with the presence of myasthenia gravis; individuals with the history of neurological disorders or inability to communicate normally; individuals with long-term use of analgesic drugs; individuals with surgical time of (5-10 min) exceeding 15 min and patients who changed their surgical methods halfway.
Treatment method:
All the patients were subjected to fasting for at least 6 h and abstained from drinking for 2 h before surgery.
Blood Pressure (BP), HR and Oxygen Saturation (SpO2) were monitored after entering the operating room and the peripheral vein was opened, without pre-anesthetic medication. O2 was administered with a nasal catheter at 3 l/min. The operation was started after the administration of an appropriate dose of Nal (0.15 mg/kg) for 3 min and intravenous bolus injection of RMZ where Ramsay score was 5 points while OAA/S score of 1. RMZ dosage was determined by Efron’s Biased Coin Design (BCD) method. RMZ dose for the 1st patient was determined based on previous painless gastroenteroscopy studies. The 1st patient was given 0.25 mg/kg of RMZ and operation was started once the Ramsay score was 5 points and OAA/S score was 1 point. If the previous patient responded positively, then RMZ dose was increased by dose gradient for the next patient. In contrast, RMZ dosage was reduced by 1 dose gradient in the next patient if the previous patient responded negatively. The adjacent dose gradient of RMZ was set to 0.025 mg/kg by arithmetic progressions. If the patient develops somatic motor reflexes, 5 mg/dose of RMZ was given as rescue dose and the regimen was repeated until the motor reflexes disappeared.
If SBP during anesthesia was <30 % of the basic value, 1-2 mg of dopamine was injected intravenously; 0.3- 0.5 mg atropine was given in the case of HR≤50 beats/min; When SpO2 was no >90 %, the oxygen flow was increased and the airway was opened by holding the mandible and placing an oropharynx breather; if the condition did not improve, the breathing bag was manually controlled through the mask to assist ventilation. The recovery time refers to the time from the last intravenous injection of RMZ to the time when the patient could respond to calls with an OAA/S score of 4-5 points. When the patient recovered from anesthesia, with Staward score ≥4, consciousness level 4, and no dizziness and other discomfort, she was escorted out of the abortion room by nurses and transferred to the observation room for further monitoring and observation. Patients were followed up 1 h later.
Outcome measures:
The primary outcome measure was the RMZ dose while the secondary measures were vital signs that included Mean Arterial Pressure (MAP) and HR at the time of admission to the operating room, after injection, at the beginning and end of surgery, and at the time of recovery from anesthesia, operation duration, recovery time, and the incidence of adverse reactions such as uterine contraction pain, dizziness, hypoxemia, bradycardia, nausea and vomiting, etc.
Statistical analysis:
Excel and Statistical Package for Social Sciences (SPSS) software were used for data entry and statistical analysis, respectively. Continuous variables conforming to normal distribution was expressed by mean±standard deviation (x±s). Inter-group comparisons used one-way Analysis of Variance (ANOVA) and multiple time-point comparisons of hemodynamics were employed using repeated measures of ANOVA. Categorical variables are presented as percentages and Chi-square (χ2) test was used for comparisons. Mean Effective Dose (ED50), ED95 and 95 % Confidence Interval (CI) were calculated by Probit analysis. BCD test diagram and dose-effect curves were made by using GraphPad Prism.
Results and Discussion
Baseline data of all the patients was studied. Mean age of the 33 patients undergoing induced abortion was (28.73±6.22) y, with an average weight of (52.44±7.20) kg, BMI of (21.17±2.36) kg/m2 and duration of amenorrhea of (46.43±8.01) d. In terms of ASA grading, there were 16 patients of grade I and 17 patients of grade II (Table 1).
| Indicators | n=30 |
|---|---|
| Age (y) | 28.73±6.22 |
| Weight (kg) | 52.44±7.20 |
| BMI (kg/m2) | 21.17±2.36 |
| Duration of menopause (d) | 46.43±8.01 |
| ASA grade (I/II) | 14/16 |
Table 1: Analysis of Baseline Data
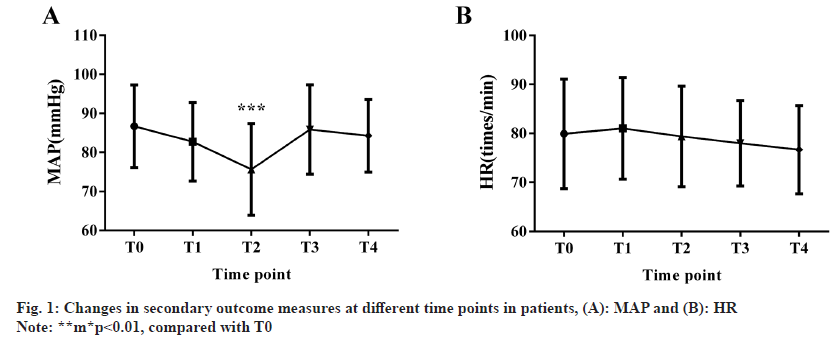
MAP and HR were evaluated at different time points. MAP results showed that compared with T0, patients’ MAP decreased significantly at T2 (p<0.05), but did not alter significantly at other time points (p>0.05), while no marked differences were identified in HR data across various time points (p>0.05) (fig. 1).
RMZ dose, operation duration and recovery time was evaluated among all the patients. The average dose of RMZ in 33 patients undergoing induced abortion was (22.21±5.02) mg while the operation duration and recovery time were (5.70±1.78) min and (3.67±1.15) min, respectively.
Adverse reactions of the patients were assessed where we found that the number of adverse reactions such as uterine contraction pain, dizziness, hypoxemia, bradycardia, nausea and vomiting in 33 patients with induced abortion was 4, 4, 5, 2 and 0, respectively, among which hypoxemia (15.15 %) was the most frequent, followed by uterine contraction pain and dizziness (both 12.12 %) and finally bradycardia (6.06 %) (Table 2).
| Indicators | n=30 |
|---|---|
| Uterine contraction pain | 4 (13.33) |
| Dizziness | 4 (13.33) |
| Hypoxemia | 5 (16.67) |
| Bradycardia | 2 (6.67) |
| Nausea and vomiting | 0 (0.00) |
| Total | 11 (36.67) |
Table 2: Adverse Reactions Among Patients
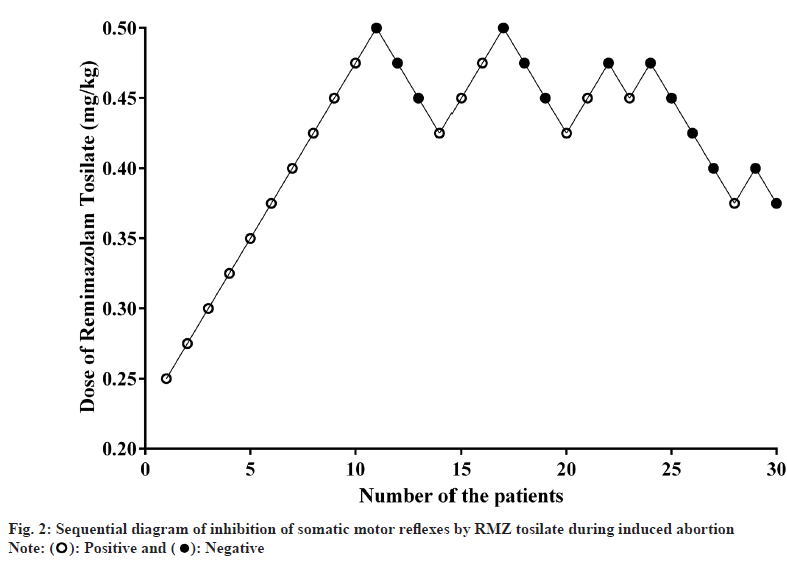
Sequential diagram and dose-effect curve were constructed. The initial dose of RMZ was 0.250 mg/ kg. A negative response occurred in the 11th and the 8th turning point occurred when the 33 patients were included. The trial was terminated when a negative reaction occurred in the 33 patients. 19 patients (57.6%) showed positive responses and 14 patients (42.4 %) had negative responses. Sequential diagram of RMZ inhibition of somatic motor reflexes (fig. 2). The regression equation as per Probit analysis was obtained for ED50 with a good fit as indicated by χ2=3.890 and p=0.919>0.05.
Probit (p) regression analysis=-5.512+12.548l g
In the context of Nal sedation, ED50 and ED95 of RMZ in inhibiting somatic motor reflexes during induced abortion were 0.439 mg/kg (95 % CI was 0.375-0.543 mg/kg) and 0.570 mg/kg (95 % CI was 0.500-1.533 mg/kg), respectively (Table 3).
| Dose (mg/kg) | n | Effectiveness/n (%) | ED50/mg·kg-1 (95 % CI) | ED95/mg·kg-1 (95 % CI) |
|---|---|---|---|---|
| 0.25 | 1 | 0 (0) | 0.439 (0.375, 0.543) | 0.570 (0.500, 1.533) |
| 0.275 | 1 | 0 (0) | ||
| 0.3 | 1 | 0 (0) | ||
| 0.325 | 1 | 0 (0) | ||
| 0.35 | 1 | 0 (0) | ||
| 0.375 | 3 | 1 (33.3) | ||
| 0.4 | 3 | 2 (66.7) | ||
| 0.425 | 4 | 1 (25.0) | ||
| 0.45 | 7 | 3 (42.9) | ||
| 0.475 | 6 | 4 (66.7) | ||
| 0.5 | 2 | 2 (100.0) |
Table 3: Corresponding Dose of Remimazolam Tosilate Used in Patients
To further optimize the experience of painless induced abortion, the combination of sedatives and analgesics is often the key to success of the surgery in alleviating pain and anxiety in female patients[18]. Although surgical duration of painless induced abortion is very short, patients often need to be discharged after symptoms such as dizziness and pain disappear[19], so it is necessary to continue to optimize sedation and analgesia strategies for painless induced abortion.
The strategy chosen in this study is the combination of RMZ and Nal. Of them, Nal can act on the spinal cord where the sympathetic and parasympathetic nervous systems have major impact on the uterus, accelerate the onset of effect and prolong the action time with the advantages of hemodynamic stability and mild respiratory depression, that may have certain clinical advantages in induced abortion and postoperative analgesia[20]. In the research of Fang et al.[21], Nal+propofol have been indicated to be superior to sufentanil+propofol in terms of clinical efficacy in induced abortion during early pregnancy, which is mainly reflected in the lower postoperative pain score, lower incidence and intensity of injection pain with higher patient satisfaction in the Nal group. However, Nal alone is not sufficient to meet the surgical needs; thus, it often needs to be combined with other drugs to ensure effectiveness. For example, according to Liu et al.[22], combined effect of ropivacaine in primiparas has significantly relieved pain faster during labor with lower risk of urinary retention. RMZ is new ultra-shortacting benzodiazepine, which can be used for gastrointestinal endoscopy to sedate and promote recovery, while being effective and safe for general anesthesia induction in ASA I or II patients[23]. RMZ has significant prophylactic effect on propofol injection-induced pain in patients with abortion or uterine curettage, with efficacy comparable to that of lidocaine and no serious adverse events, according to prospective, double-blind study[24]. It also has advantages over midazolam where carboxylate bonds are rapidly metabolized by tissue esterases into harmless metabolites and are associated with faster postoperative recovery than midazolam[25,26]. In this study, 30 individuals having mean age of 28.73±6.22 y, average weight of 52.44±7.20 kg with BMI of 21.17±2.36 kg/m2 and duration of menopause of 46.43±8.01 d, with induced abortion were included, with 14 patients of ASA grade I and 16 patients of ASA grade II. According to the hemodynamic analysis, MAP of patients at T2 reduced markedly versus T0, but HR did not changed statistically among multiple time points, suggesting that RMZ+Nal has little effects on hemodynamics during abortion operation. In a study by Yue et al.[27], the combination of RMZ and esketamine in abortion patients can not only take effect quickly and promote postoperative recovery, but also had mild hemodynamic side effects, similar to our research results. Perioperative data showed that the average RMZ dosage was (22.21±5.02) mg, average operation duration was (5.70±1.78) min and mean recovery time was (3.67±1.15) min. Hypoxemia (15.15 %), followed by uterine pain and dizziness (both 12.12 %) and bradycardia (6.06%) were the most common adverse events in perioperative patients.
This study showed that when 0.15 mg/kg of Nal was injected in painless induced abortion, ED50 and ED95 of RMZ in inhibiting somatic motor reflexes were 0.439 mg/kg (95 % CI was 0.375-0.543 mg/kg) and 0.570 mg/kg (95 % CI was 0.500-1.533 mg/kg), respectively, with obvious adverse reactions. This strategy can provide a new sedation and analgesia option for patients with painless induced abortion.
Funding:
This study was supported by the Guangdong Provincial Hospital Pharmacy Research Fund (Xinchen Comfort Medical Special Fund) (Grant No: 2020XC33).
Conflict of interests:
The authors declared no conflict of interests.
References
- Wang LH, Zhu HX, Su XJ, Hao WB. Anesthetic effect of preemptive analgesia of frequency acupoint electrical stimulation on painless-induced abortion. Zhongguo Zhen Jiu 2014;34(7):691-4.
[Google Scholar] [PubMed]
- Wu J, Han Y, Yang L, Liu Z. Analysis on the effect of intravenous anesthesia with dexmedetomidine and propofol combined with seaweed polysaccharides on hemodynamics and analgesia in pregnant females undergoing painless induced abortion. Pak J Pharm Sci 2021;34:1249-54.
[Crossref] [Google Scholar] [PubMed]
- Zheng M, Guo Y, Shan S, Yang S. Dezocine for anesthesia and stress reduction in induced abortion. Patient Prefer Adherence 2015;9:369-72.
[Crossref] [Google Scholar] [PubMed]
- Wang L, Li W, Xu R, Long L. Meta-analysis for the anesthesia effect and adverse reactions of etomidate and propofol on the painless abortion surgery. Zhong Nan Da Xue Xue Bao Yi Xue Ban 2016;41(4):427-33.
[Crossref] [Google Scholar] [PubMed]
- Yang Z, Yi B. Patient experience of sexual hallucinations after propofol-induced painless abortion may lead to violence against medical personnel. J Anesth 2016;30(3):486-8.
[Crossref] [Google Scholar] [PubMed]
- Zheng Y, Huang J, Mai Y, Li X, Zhang Z. The median effective dose of propofol combined with butorphanol during artificial abortion: A randomized controlled trial. Front Med 2023;10:1-12.
[Crossref] [Google Scholar] [PubMed]
- Quan ZF, Tian M, Chi P, Li X, He HL. Effective analgesic dose of dexamethasone after painless abortion. Int J Clin Exp Med 2014;7(8):2144-9.
[Google Scholar] [PubMed]
- Chen SH, Yuan TM, Zhang J, Bai H, Tian M, Pan CX, et al. Remimazolam tosilate in upper gastrointestinal endoscopy: A multicenter, randomized, non-inferiority, phase III trial. J Gastroenterol Hepatol 2021;36(2):474-81.
[Crossref] [Google Scholar] [PubMed]
- Wiltshire HR, Kilpatrick GJ, Tilbrook GS, Borkett KM. A placebo- and midazolam-controlled phase I single ascending-dose study evaluating the safety, pharmacokinetics, and pharmacodynamics of remimazolam (CNS 7056): Part II. Population pharmacokinetic and pharmacodynamic modeling and simulation. Anesth Analg 2012;115(2):284-96.
[Crossref] [Google Scholar] [PubMed]
- Morimoto Y, Yoshimatsu A, Yoshimura M. Anesthetic management for a patient with myotonic dystrophy with remimazolam. JA Clin Rep 2021;7(1):1-10.
[Crossref] [Google Scholar] [PubMed]
- Kim KM. Remimazolam: Pharmacological characteristics and clinical applications in anesthesiology. Anesth Pain Med 2022;17(1):1-11.
[Crossref] [Google Scholar] [PubMed]
- Stohr T, Colin PJ, Ossig J, Pesic M, Borkett K, Winkle P, et al. Pharmacokinetic properties of remimazolam in subjects with hepatic or renal impairment. Br J Anaesth 2021;127(3):415-23.
[Crossref] [Google Scholar] [PubMed]
- Mello NK, Mendelson JH, Sholar MB, Jaszyna-Gasior M, Goletiani N, Siegel AJ. Effects of the mixed mu/kappa opioid nalbuphine on cocaine-induced changes in subjective and cardiovascular responses in men. Neuropsychopharmacology 2005;30(3):618-32.
[Crossref] [Google Scholar] [PubMed]
- van Niel JC, Schneider J, Tzschentke TM. Efficacy of full µ-opioid receptor agonists is not impaired by concomitant buprenorphine or mixed opioid agonists/antagonists-preclinical and clinical evidence. Drug Res 2016;66(11):562-70.
[Crossref] [Google Scholar] [PubMed]
- Chen JC, Smith ER, Cahill M, Cohen R, Fishman JB. The opioid receptor binding of dezocine, morphine, fentanyl, butorphanol and nalbuphine. Life Sci 1993;52(4):389-96.
[Crossref] [Google Scholar] [PubMed]
- Pick CG, Paul D, Pasternak GW. Nalbuphine, a mixed kappa 1 and kappa 3 analgesic in mice. J Pharmacol Exp Ther 1992;262(3):1044-50.
[Google Scholar] [PubMed]
- Ortiz MI, Carino-Cortes R, Castaneda-Hernandez G. Participation of the opioid receptor-nitric oxide-cGMP-K+ channel pathway in the peripheral antinociceptive effect of nalbuphine and buprenorphine in rats. Can J Physiol Pharmacol 2020;98(11):753-62.
[Crossref] [Google Scholar] [PubMed]
- Allen RH, Singh R. Society of family planning clinical guidelines pain control in surgical abortion part 1-local anesthesia and minimal sedation. Contraception 2018;97(6):471-7.
[Crossref] [Google Scholar] [PubMed]
- Dragoman MV, Grossman D, Nguyen MH, Habib N, Kapp N, Tamang A, et al. Two prophylactic pain management regimens for medical abortion ≤63 d gestation with mifepristone and misoprostol: A multicenter, randomized, placebo-controlled trial. Contraception 2021;103(3):163-70.
[Crossref] [Google Scholar] [PubMed]
- Zeng R, Dong S, Wei Y. Influences of different doses of nalbuphine combined with propofol on the anesthetic effects, hemodynamics, inflammation and immunity of patients undergoing hysteroscopic surgery. Panminerva Med 2023;65(2):270-1.
[Crossref] [Google Scholar] [PubMed]
- Fang P, Qian J, Ding J, Pan X, Su H, Liu X. Comparison of analgesic effects between nalbuphine and sufentanil in first-trimester surgical abortion: A randomized, double-blind, controlled trial. Pain Ther 2022;11(1):121-32.
[Crossref] [Google Scholar] [PubMed]
- Liu GH, Liu LW, Ou LC, Cao XS, Pang Z, Wen XJ, et al. Effect of nalbuphine plus ropivacaine on vaginal labor in epidural analgesia. BMC Anesthesiol 2023;23(1):1-6.
[Crossref] [Google Scholar] [PubMed]
- Dai G, Pei L, Duan F, Liao M, Zhang Y, Zhu M, et al. Safety and efficacy of remimazolam compared with propofol in induction of general anesthesia. Minerva Anestesiol 2021;87(10):1073-9.
[Crossref] [Google Scholar] [PubMed]
- Guan X, Jiao Z, Gong X, Cao H, Liu S, Lan H, et al. Efficacy of pre-treatment with remimazolam on prevention of propofol-induced injection pain in patients undergoing abortion or curettage: A prospective, double-blinded, randomized and placebo-controlled clinical trial. Drug Des Devel Ther 2021;15:4551-8.
[Crossref] [Google Scholar] [PubMed]
- Sneyd JR, Rigby-Jones AE. Remimazolam for anaesthesia or sedation. Curr Opin Anaesthesiol 2020;33(4):506-11.
[Crossref] [Google Scholar] [PubMed]
- Schippers F, Pesic M, Saunders R, Borkett K, Searle S, Webster L, et al. Randomized crossover trial to compare abuse liability of intravenous remimazolam vs. intravenous midazolam and placebo in recreational central nervous system depressant users. J Clin Pharmacol 2020;60(9):1189-97.
[Crossref] [Google Scholar] [PubMed]
- Yue L, Ma X, Li N, Chen J, Wang J, Wan Z, et al. Remimazolam vs. propofol in combination with esketamine for surgical abortion: A double-blind randomized controlled trial. Clin Transl Sci 2023;16(9):1606-16.
[Crossref] [Google Scholar] [PubMed]
 ): Positive and (
): Positive and ( ): Negative
): Negative



