- *Corresponding Author:
- H. R. L. B. Gen
Department of Medicine, Inner Mongolia Medical University, Hohhot, Inner Mongolia 010107, China
E-mail: hurile1997@163.com
| This article was originally published in a special issue, “Drug Discovery and Repositioning Studies in Biopharmaceutical Sciences” |
| Indian J Pharm Sci 2024:86(4) Spl Issue “129-135” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
Aim of this study was to study serum microribonucleic acid-30a expression and the cardioprotective mechanism of Mongolian medicine, Zadi-5 in myocardial ischemia-reperfusion injury model rats. 84 Sprague-Dawley male rats were selected and were divided into 7 groups, namely blank, model, sham operation, Chinese medicine, as well as Mongolian medicine high, medium and low dose groups, each with 12 rats. Among them, the Chinese medicine group was intervened by compound Danshen dripping pills while the Mongolian medicine (Zadi- 5) of high (1.6 g/kg), medium (0.8 g/kg) and low dose (0.4 g/kg) groups were given and the blank group was given an equal volume of distilled water of 1.0 ml/100 g. Myocardial ischemia-reperfusion injury rat model was established and the model was evaluated by electrocardiogram. In addition, serum and cardiac tissues of each group were collected to measure serum aspartate aminotransferase, lactate dehydrogenase and lactate dehydrogenase-1 contents; infarct area and cardiomyocyte apoptosis rate of rats were detected. Furthermore, the morphological changes of myocardial tissue, B cell lymphoma-2 and B cell lymphoma-2- associated protein X expression and microribonucleic acid-30a levels in myocardial tissue were determined. The experimental results showed successful construction of the MIRI rat model. Meanwhile, the arrangement of myocardial cells in the model group was disordered, accompanied by cell rupture, necrosis, inflammatory cell infiltration and myocardial fiber rupture; while the Chinese medicine and Mongolian medicine groups had reversed histological changes to varying degrees. The model group showed markedly reduced B cell lymphoma-2 protein expression and microribonucleic acid-30a levels in myocardial tissue than in blank and sham operation groups; however, B cell lymphoma-2 protein expression and miR-30a levels showed increasing trend of Chinese medicine as well as high and medium doses of Mongolian medicine. Zadi-5 may exert a cardioprotective effect by up-regulating serum microribonucleic acid-30a expression in ischemia-reperfusion injury rats.
Keywords
Zadi-5, ischemia, apoptosis, cardioprotection, B cell lymphoma-2, cardiomyocyte
Cardiovascular disease has always been a major threat to human health all over the world, among which acute Myocardial Infarction (MI) is a threat, which can easily lead to the onset and progression of ischemic heart failure[1,2]. Ischemia-Reperfusion Injury (IRI) is a key pathogenesis of myocardial injury associated with acute MI, which can lead to abnormal pathological manifestations such as cardiac insufficiency as well as Cardiomyocyte (CM) loss, fibrosis and apoptosis[3,4]. At present, the strength of treatment for Myocardial IRI (MIRI) is thrombolytic therapy, percutaneous coronary intervention or other revascularization which can achieve early restoration of blood flow in ischemic tissues and avoid ischemic CM death. However, these therapies may further aggravate cardiac damage[5,6]. Therefore, the exploration of MIRI treatment needs to be continuously advanced. In this study, we plan to construct a rat MIRI model and explore the effective treatment of MIRI from the mechanism of myocardial protection, aiming to provide new ideas for cardioprotection in MIRI-related patients.
In China, a history over years has shaped its ancient, unique and highly effective medical system (i.e. traditional Chinese medicine)[7]. Among them, there are also unique medical systems constructed by ethnic minorities, such as Mongolian medicine. Mongolian medicine focuses on the balance of the three elements of life namely, hii (wind), sar (bile) and badgan (phlegm). Doctors judge the unbalanced state of the body through observation, palpation and inquiry. Treatment mainly involves changing the patient's diet and behavior, supplemented with Mongolian medicine or other topical therapies according to the condition[8-10]. Mongolian medicine belongs to a branch of traditional Chinese medicine, which is made from natural plants, animals and mineral products; it comes in the form of decoctions, powders, pills and ointments[11,12]. This study focuses on the Mongolian medicine Zadi-5, also known as nutmeg-5, which is composed of nutmeg, Choerospondias axillaris fruit, Piper longum, Inula helenium (elecampane) root and Radix Aucklandia, etc., which can be used to treat heart diseases such as rapid heartbeat, palpitations, angina pectoris, vexation, insomnia and uneasiness. In the research of Wu et al.[13], it is also pointed out that the drug can be used for the treatment of depression in rat models and play an antidepressant role by coordinating the Phosphatidylinositol 3 kinase-protein Kinase B (PI3K-Akt) pathway.
Currently, research on serum micro Ribonucleic Acid (miRNA)-30a expression and the mechanism underlying the cardioprotection of Mongolian medicine Zadi-5 in MIRI model rats is relatively limited. This study hereby analyzed and validated to provide more clinical therapies.
Materials and Methods
Grouping and intervention:
84 Sprague-Dawley (SD) male rats, weighing 200±20 g, were randomized into 7 groups, namely blank, model, sham operation, Chinese medicine, high, medium, and low dose Mongolian medicine groups, each with 12 rats. Chinese medicine group was given 0.5 g/kg of compound Danshen dripping pills diluted in distilled water. 1.6 g/kg, 0.8 g/kg and 0.4 g/kg of Zadi-5 (Mongolian medicine) was given to high, medium and low dose groups by diluting in distilled water, respectively. Similarly, 1.0 ml/100 g of Zadi-5 were given distilled water of equal volume by gavage to blank, model and sham operation groups. The drug treatment was continued for 14 d once/day.
Preparation of animal model:
MIRI rat model was established by ligating the anterior descending branch of the left coronary artery 12 h after the last administration. Sham operation group was threaded but not ligated. The remaining administration groups underwent thoracotomy and ligation of the left anterior descending coronary artery for 30 min before reperfusion for 90 min. Electrocardiogram (ECG) was recorded to evaluate the validity of the model. Serum and heart tissue were collected for further study after successful modeling.
Enzyme-Linked Immunosorbent Assay (ELISA):
ELISA was carried out to determine serum Aspartate aminotransferase (AST), Lactate Dehydrogenase (LDH) and LDH-1 contents, and the experimental process strictly followed the kit instructions.
2,3,5-Triphenyl Tetrazolium Chloride (TTC) staining:
First, the heart was separated, rinsed with normal saline and refrigerated at -80° for 20 min. Then, the heart was cut into 2 mm slices along the long axis, placed in 1 % TTC solution, incubated at 37° for 30 min and fixed with 10 % neutral formaldehyde. Macroscopically, the non-infarcted myocardium was red and the infarct area was white. Using CIMA2400 image capturing analysis software system the percentage of MI area was calculated.
Terminal deoxynucleotidyl Transferase (TdT)- mediated deoxyuridine Triphosphate (dUTP) Nick End-Labeling (TUNEL):
Paraffin sections of rat myocardial tissue were made. TUNEL staining was performed according to the TUNEL apoptosis detection kit instructions after routine deparaffinization and hydration, followed by observation and visualizing under a light microscope. 5 visual fields were randomly selected from each paraffin section to count the number of positive cells and the total number of cells using ImageJ software. TUNEL assay denoted positive apoptotic CMs which were brown and normal CMs were blue and the apoptosis rate was calculated.
Number of positive cells/total number of cells×100 %
Morphological changes of myocardial tissue using Hematoxylin and Eosin (H&E) staining:
A portion of the myocardial tissue was immobilized using 10 % neutral formaldehyde solution and then cut into 5 μm serial sections using a tissue microtome after gradient alcohol dehydration, xylene transparentization and paraffin embedding. Following de-waxing with xylene and hydrating with gradient alcohol, the slices were dyed with H&E dye solution, differentiated with 75 % hydrochloric acid ethanol, stained with ammonia solution and dyed with H&E dye solution. This was followed by another gradient alcohol dehydration and xylene transparentization, after which neutral balsam was dripped to mount the slices. The pathological changes of myocardial tissue were finally observed under an optical microscope.
Western blotting:
B cell lymphoma-2 (Bcl-2) and Bcl-2-Associated protein X (BAX) protein levels in myocardial tissue were tested. Total tissue protein, extracted with a protein extraction kit, was quantified by the Bradford method. Then, an equal-volume loading buffer was added in boiling water bath for 10 min to denaturate the protein. Then, 20 μg of protein-like solution was transferred onto a Polyvinylidene Difluoride (PVDF) membrane by wet electroblotting. The PVDF membrane was sealed using 5 % skimmed milk powder for 2 h at room temperature, washed using Tris-Buffered Saline with Tween (TBST) buffer, incubated at 4° for 24 h. This process was followed by another TBST rinsing for 1 h at room temperature culture with corresponding second antibody diluent (dilution ratio: 1:2000), and continued the same process for 3 TBST rinses. After chemiluminescence assay for development, the protein bands were detected by an automatic gel imaging analysis system and the target proteins’ relative expression was detected and calculated by ImageJ software.
Real-time quantitative Reverse Transcription Polymerase Chain Reaction (qRT-PCR):
Total RNA was extracted from rat myocardium by the Total RNA Isolation (TRIzol) reagent, and its concentration and purity were detected by an ultraviolet spectrophotometer; complementary Deoxyribonucleic Acid (cDNA) was obtained from reverse transcription kit of RNA and used as a template for PCR amplification. Primer design and synthesis were obtained from Shanghai Xinfan Biotech, Co. Ltd., China. miR-30a expression relative to U6 was calculated using the 2-ΔΔct formula.
Statistical analysis:
Statistical Package for Social Sciences (SPSS) version 22.0 data statistics software was used for statistical processing. All the data was presented as mean±Standard Deviation (x̄±SD), using one-way Analysis of Variance (ANOVA) or Tamhane’s T2 test (in case of uneven variance) for analysis; p<0.05 were considered to be statistically different.
Results and Discussion
Animal model was constructed and pathological changes were studied. According to ECG and H&E staining, the rat limb at lead II position showed STsegment elevation when the left anterior descending coronary artery was ligated for ischemia, but the ST segment gradually returned to normal during reperfusion, indicating the successful construction of a MIRI model. By H&E staining, it was observed that the myocardial tissue and cells of the model group rats were disorderly arranged, with cell rupture and necrosis, inflammatory cell infiltration, and myocardial fiber rupture; however, the histological changes were alleviated in the Chinese and Mongolian medicine groups to varying degrees.
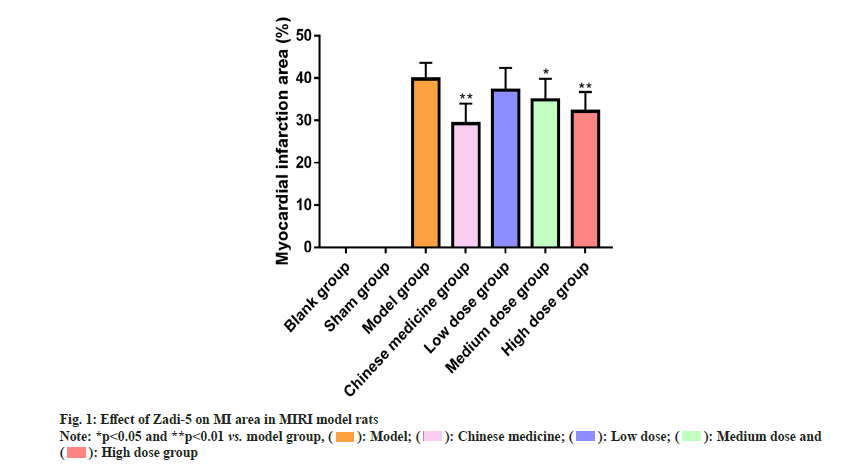
Effect of Zadi-5 on MI area in MIRI model rats was studied. MI area of the model group increased statistically compared to the blank and sham operation groups (p<0.05). Chinese medicine group and Mongolian medicine high and medium dose groups showed markedly reduced MI area (p<0.05); however, low-dose Zadi-5 had no significant effect on the MI area (p>0.05) (fig. 1).
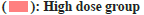
Further, the influence of Zadi-5 on serum AST, LDH and LDH-1 contents in MIRI model rats was studied. Serum AST, LDH, and LDH-1 contents were statistically elevated in the model group vs. blank and sham operation groups (p<0.05). Serum AST, LDH, and LDH-1 of rats in the Chinese medicine group and Mongolian high and medium medicine dose groups statistically decreased (p<0.05), but their levels were barely changed in the Mongolian medicine low dose group (p>0.05) (fig. 2).
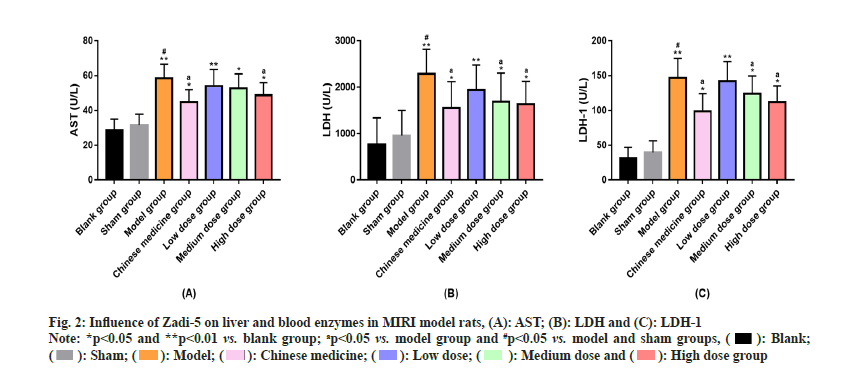
Similarly, the impact of Zadi-5 on BAX and Bcl-2 proteins in myocardial tissue of MIRI model rats was evaluated. Marked rise in BAX protein expression and an evident reduction in Bcl-2 protein expression were determined in the model group compared to the blank and sham operation groups (p<0.05). Chinese medicine group and Mongolian medicine high and medium dose groups showed higher Bcl-2 protein expression and lower BAX protein expression in the myocardial tissue than the model group (p<0.05); Bcl-2 protein expression was also elevated in the myocardium of rats in Mongolian medicine low dose group compared to the model group (p<0.05), but the BAX protein expression differed slightly (p>0.05) (fig. 3).
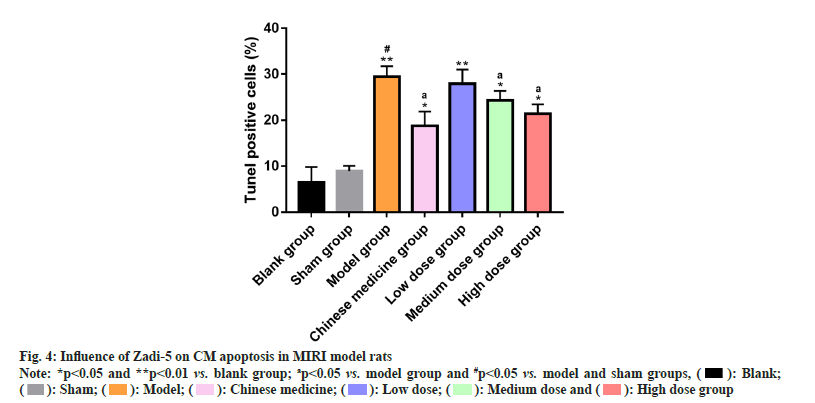
Subsequently, the influence of Zadi-5 on CM apoptosis in MIRI model rats was assessed where the model group had an elevated CM apoptosis rate than the blank and sham operation groups (p<0.05). In comparison with the model group, CM apoptosis rate in the Chinese medicine group rats and Mongolian medicine high and medium dose groups statistically decreased (p<0.05); however, in Mongolian medicine low dose group was not statistically affected (p>0.05) (fig. 4).
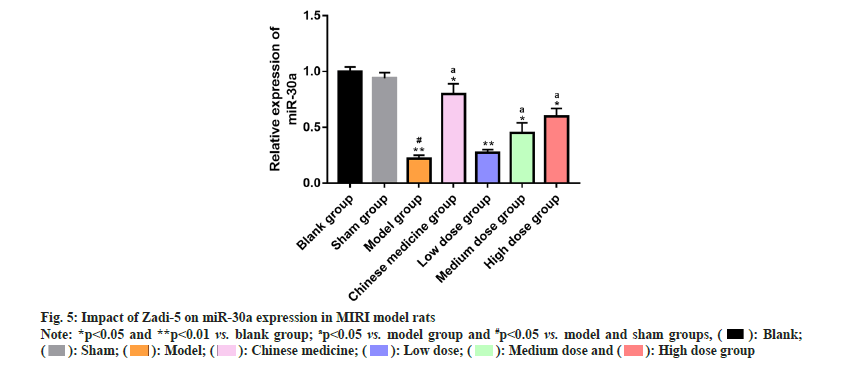
Finally, the impact of Zadi-5 on miR-30a expression in MIRI model rats was evaluated which depicted statistically decreased miR-30a expression in the model group compared to blank and sham operation groups (p<0.05). In comparison with the model group, miR-30a expression in rats of the Chinese medicine group and Mongolian medicine high and medium dose groups increased statistically (p<0.05), while that of the low dose Mongolian medicine group showed a non-significant increasing trend (p>0.05) (fig. 5).
There is a positive correlation between the risk of acute MI and age, preferably in people >65 y, who are likely to develop shock, atrial fibrillation, cardiac rupture and heart failure than younger patients[14]. MIRI is closely associated with acute MI, which progressively induces systemic inflammatory response that leads to multi-organ dysfunction[15]. Treatment of related disorders is primarily focused on preventing or ameliorating damage caused by reperfusion, which requires a better understanding of the mechanisms associated with MIRI in order to better develop therapies[16].
There have also been some studies on the mechanism of cardioprotection action of Mongolian medicine in MIRI. For example, in the research of Huang et al.[17], Anshen-Buxin-Liuwei pill alleviated CM hypoxia/ reoxygenation injury through the mitochondrial pathway, which has certain potential in the treatment of ischemic cardiovascular diseases. Similarly, as reported by Yang et al.[18], Shaosha-7 is effective in ameliorating arrhythmia and pathological changes, reducing infarct area, regulating myocardial injury and inflammation-related indicators in MIRI model rats, with certain anti-MIRI therapeutic effects. Furthermore, Sun et al.[19] pointed out that Sanwei- Tanxiang powder can play a cardioprotective role in MIRI rats and H9c2 cardiomyoblast cells by mediating the PI3K/Akt/Forkhead box O (FoxO) 3a pathway. In this study, the MIRI model rats were constructed successfully and exhibited typical pathological features of MIRI at both the myocardial tissue and cellular levels. After intervention with Chinese medicine, i.e., compound Danshen dripping pills and various doses (0.4 g/kg, 0.8 g/kg and 1.6 g/kg) of Mongolian medicine (Zadi-5), some MIRI pathological features were effectively reversed. In a proteomics and metabolomics study, intervention with Mongolian medicine Zadi-5 in MIRI model rats validly alleviated MI, enhanced cardiac function, reduced cardiac fibrosis and relieved myocardial injury. The mechanism was related to its regulation of the Extracellular Matrix (ECM)-receptor interaction and Transforming Growth Factor (TGF)-Beta (β)1/ Suppressor of mothers against decapentaplegic homolog 2 (Smad2) signaling[20]. Liu et al.[21] also reported that the mechanism of Zadi-5 on cardiac remodeling in MIRI model rats was associated with the regulation of cardiac metabolism and downregulation of Hypoxia Inducible Factor (HIF)-1 Alpha (α) expression. In this study, the MI area of MIRI model rats increased abnormally. However, the MI area statistically reduced after the intervention of compound Danshen dripping pills and medium and high dose groups of Zadi-5 medicine, suggesting that at least 0.8 g/kg of Zadi-5 can help significantly inhibit MI; serum AST, LDH and LDH-1 can reflect myocardial injury[22]. Through this study, we found that at least 0.8 g/kg of Zadi-5 can significantly reduce serum contents of AST, LDH and LDH-1 in rats, demonstrating that this dose was effective in inhibiting myocardial injury. In terms of apoptosis, MIRI model rats exhibited an abnormal increase in the CM apoptosis rate, rise in BAX protein expression in myocardial tissue and a reduction in Bcl-2 protein expression. All the above abnormal manifestations were significantly alleviated after intervention with compound Danshen dripping pills and medium and high dose groups of Zadi-5, indicating that 0.8 g/kg of Zadi-5 can significantly inhibit apoptosis and play a cardioprotective role. Finally, we found that the above therapeutic effects of Zadi-5 may be related to its up-regulation of miR-30a expression in MIRI rats. miR-30a is known to participate in a number of regulatory mechanisms in MIRI, which can alleviate myocardial apoptosis in MIRI rats by reducing autophagy[23]; miR-30a may also be involved in modulating the cardioprotective effect of osthole on MIRI[24]. In the study by Wang et al.[25], miR-30a can also participate in the DNA Methyltransferase 3B (DNMT3b)-dependent activation of Hypoxia Postconditioning (HPostC), thus protecting the aged CMs and reducing MIRI, which can be used as a potential therapeutic target for ischemic MI to a certain extent.
In short, Zadi-5 (at least 0.8 g/kg) has a certain anti- MIRI therapeutic effect and its mechanism may be related to Zadi-5-induced increase in miR-30a expression in MIRI rats, playing cardioprotective role by inhibiting lipid peroxidation of the myocardial cell membrane and alleviating apoptosis in a genetically regulated manner. Our findings may provide more options for MIRI treatment and understanding of the mechanisms involved.
Funding:
This study was supported by “Effects of Mongolian Medicine Anshen Buxin Liuwei Pill on Intestinal Microecology in Rats with Myocardial Ischemia Model of Coronary Heart Disease” (Grant No: myxylxk202108) and “A Study on the Integration of Chinese, Mongolian and Tibetan Medicine in the Qing Dynasty based on Mongolian Medical Classics” (Grant No: YLXKZX-NYD-004).
Conflict of interests:
The authors declared no conflict of interests.
References
- Tian H, Zhao X, Zhang Y, Xia Z. Abnormalities of glucose and lipid metabolism in myocardial ischemia-reperfusion injury. Biomed Pharmacother 2023;163:1-11.
[Crossref] [Google Scholar] [PubMed]
- Liu Y, Li L, Wang Z, Zhang J, Zhou Z. Myocardial ischemia-reperfusion injury: Molecular mechanisms and prevention. Microvasc Res 2023;149:1-10.
[Crossref] [Google Scholar] [PubMed]
- He J, Liu D, Zhao L, Zhou D, Rong J, Zhang L, et al. Myocardial ischemia/reperfusion injury: Mechanisms of injury and implications for management. Exp Ther Med 2022;23(6):1-13.
[Crossref] [Google Scholar] [PubMed]
- Cai W, Liu L, Shi X, Liu Y, Wang J, Fang X, et al. Alox15/15-HpETE aggravates myocardial ischemia-reperfusion injury by promoting cardiomyocyte ferroptosis. Circulation 2023;147(19):1444-60.
[Crossref] [Google Scholar] [PubMed]
- Bell RM, Yellon DM. There is more to life than revascularization: Therapeutic targeting of myocardial ischemia/reperfusion injury. Cardiovasc Ther 2011;29(6):67-79.
[Crossref] [Google Scholar] [PubMed]
- Wang Q, Zuurbier CJ, Huhn R, Torregroza C, Hollmann MW, Preckel B, et al. Pharmacological cardioprotection against ischemia reperfusion injury-the search for a clinical effective therapy. Cells 2023;12(10):1-14.
[Crossref] [Google Scholar] [PubMed]
- Matos LC, Machado JP, Monteiro FJ, Greten HJ. Understanding traditional Chinese Medicine therapeutics: An overview of the basics and clinical applications. Healthcare 2021;9(3):1-17.
[Crossref] [Google Scholar] [PubMed]
- Yu E, Amri H. China's other medical systems: Recognizing Uyghur, Tibetan, and Mongolian traditional medicines. Glob Adv Health Med 2016;5(1):79-86.
[Crossref] [Google Scholar] [PubMed]
- Bromage S, Daria T, Lander RL, Tsolmon S, Houghton LA, Tserennadmid E, et al. Diet and nutrition status of Mongolian adults. Nutrients 2020;12(5):1-14.
[Crossref] [Google Scholar] [PubMed]
- Li J, Wang C, Song L, Cai S, Li Z, Tu Y. The potential mechanism of Wuwei Qingzhuo San against hyperlipidemia based on TCM network pharmacology and validation experiments in hyperlipidemia hamster. Evid Based Complement Alternat Med 2020;1-15.
[Crossref] [Google Scholar] [PubMed]
- Qu S, Bao J, Ao W, Bai L, Borjigidai A. Mongolian medicine: History, development and existing problems. Chin Herb Med 2022;14(3):345-55.
[Crossref] [Google Scholar] [PubMed]
- Luo C, Zhao W, Liu S, Luo M, Fan T, Zhao Y, et al. Animal-and mineral-based medicines in Gansu-Ningxia-inner Mongolia region PR China: A cross-cultural ethnobiological assessment. Front Pharmacol 2023;14:1-12.
[Crossref] [Google Scholar] [PubMed]
- Wu R, Zu W, Wu L, Su S, Su N, Qi L, et al. Behavioral and network pharmacology-based analyses for the traditional Mongolian medicine Zadi-5 in a rat model of depression. J Vis Exp 2023;192:1-11.
[Crossref] [Google Scholar] [PubMed]
- Rich MW. Epidemiology, clinical features, and prognosis of acute myocardial infarction in the elderly. Am J Geriatr Cardiol 2006;15(1):7-11.
[Crossref] [Google Scholar] [PubMed]
- Algoet M, Janssens S, Himmelreich U, Gsell W, Pusovnik M, van den Eynde J, et al. Myocardial ischemia-reperfusion injury and the influence of inflammation. Trends Cardiovasc Med 2023;33(6):357-66.
[Crossref] [Google Scholar] [PubMed]
- Li X, Liu M, Sun R, Zeng Y, Chen S, Zhang P. Protective approaches against myocardial ischemia reperfusion injury. Exp Ther Med 2016;12(6):3823-9.
[Crossref] [Google Scholar] [PubMed]
- Huang YJ, Tong HY, Huang XJ, Xiao XC, Dong Y, Iqbal MS. Anshen-Buxin-Liuwei pill, a Mongolian medicinal formula could alleviate cardiomyocyte hypoxia/reoxygenation injury via mitochondrion pathway. Mol Biol Rep 2022;49(2):885-94.
[Crossref] [Google Scholar] [PubMed]
- Yang XJ, Wang Y, Zhao M. Effects of Mongolian medicine Shaosha-7 on myocardial ischemia/ reperfusion injury of rats. Zhongguo Ying Yong Sheng Li Xue Za Zhi 2021;37(4):380-4.
[Crossref] [Google Scholar] [PubMed]
- Sun YH, Bu R, Wang YW, Hu YC, Wang XM, Dong X, et al. Validation of efficacy and mechanism of Sanwei-Tanxiang powder in improving myocardial ischemia reperfusion injuries. Sci Rep 2021;11(1):1-12.
[Crossref] [Google Scholar] [PubMed]
- Yan T, Zhu X, Zhang X, Jia X, Liu J, Wang X, et al. The application of proteomics and metabolomics to reveal the molecular mechanism of Nutmeg-5 in ameliorating cardiac fibrosis following myocardial infarction. Phytomedicine 2022;105:1-15.
[Crossref] [Google Scholar] [PubMed]
- Liu T, Yan T, Jia X, Liu J, Ma R, Wang Y, et al. Systematic exploration of the potential material basis and molecular mechanism of the Mongolian medicine Nutmeg-5 in improving cardiac remodeling after myocardial infarction. J Ethnopharmacol 2022;285:1-17.
[Crossref] [Google Scholar] [PubMed]
- Pareja M, Sánchez O, Lorita J, Soley M, Ramírez I. Activated epidermal growth factor receptor (ErbB1) protects the heart against stress-induced injury in mice. Am J Physiol Regul Integr Comp Physiol 2003;285(2):455-62.
[Crossref] [Google Scholar] [PubMed]
- Xu YQ, Xu Y, Wang SH. Effect of exosome-carried miR-30a on myocardial apoptosis in myocardial ischemia-reperfusion injury rats through regulating autophagy. Eur Rev Med Pharmacol Sci 2019;23(16):7066-72.
[Crossref] [Google Scholar] [PubMed]
- Liu S, He Y, Shi J, Liu L, Ma H, He L, et al. Downregulation of miRNA-30a enhanced autophagy in osthole-alleviated myocardium ischemia/reperfusion injury. J Cell Physiol 2019;619-21.
[Crossref] [Google Scholar] [PubMed]
- Wang Y, Hao Y, Zhang H, Xu L, Ding N, Wang R, et al. DNA hypomethylation of mir-30a mediated the protection of hypoxia postconditioning against aged cardiomyocytes hypoxia/reoxygenation injury through inhibiting autophagy. Circ J 2020;84(4):616-25.
[Crossref] [Google Scholar] [PubMed]