- *Corresponding Author:
- S. Khan
Institute of Pharmaceutical Education and Research (IPER), Borgaon (Meghe), Shagufta Khan c/o H. R. Khan, House No. 116, Adarshnagar, P.O. Wadi, Nagpur - 440023, India
E-mail: shaguftakhan17@rediffmail.com
| Date of Submission | 22 March 2006 |
| Date of Revision | 27 June 2007 |
| Date of Acceptance | 12 September 2007 |
| Indian J Pharm Sci, 2007, 69 (5): 626-632 |
Abstract
In the present study strong cation exchange resin (Amberlite IRP69) was used to improve the physicochemical properties of ranitidine hydrochloride such as taste and bulk properties and to sustain dissolution rate. Drug-resin complexes were prepared using batch method. Drug loading was done under different processing conditions such as temperature, pH, drug-resin ratio, and drug concentration to get the optimum condition for resinate preparation. Resinate prepared under optimized condition was tested for taste, bulk properties and release rate. Degree of bitterness of ranitidine was found to reduce to zero after complexation with resin. Improvement in flow properties was also observed. Angle of repose for resinate was found to be 33.21 o as compared to 42.27 o for ranitidine HCl. Effect of dissolution medium and particle size on in vitro release of drug from resinate was also investigated. Resinate with drug to resin ratio of 2:3 and particle size >90 µm showed about 90% of drug release within 12 h. The orodispersible tablet formulated from the resinate containing 10% croscarmellose sodium disintegrated within 35 sec in oral cavity and showed similar dissolution profile as the resinate. Tablets were found stable after stability studies with no change in dissolution profile.
Keywords
Ranitidine HCl, rapid disintegrating tablets, strong cation exchange resin, taste masking
Ranitidine HCl is a H2 receptor antagonist that competitively inhibits the interaction of histamine with its receptors on gastric parietal cells. In virtue of this action, ranitidine HCl finds application in the treatment of acid peptic disorders ranging from heartburn to peptic ulcer and more severe conditions like Zolinger Ellison Syndrome1 and gastro esophageal reflux. However short biological half-life of ranitidine HCl (2-3 h)2 necessitate frequent (four times a day) administration of the drug in severe hyperacidic conditions like erosive esophagitis. Also, minimum effective concentration of ranitidine HCl is 100 ng/ml, but with conventional dosage forms concentration reaches to 500 to 600 ng/ml in blood. Such unnecessary fluctuations can be avoided by formulating this drug in sustained release dosage form.
Ranitidine HCl is also indicated in pediatrics for the treatment of gastric ulcer and gastro esophageal reflux. But its bitter taste limits easy administration to such patients thus reduces patient compliance. In order to abate the shortcomings associated with ranitidine HCl, the present study attempts to formulate a sustained release dosage form with the improvement in physicochemical properties of the drug and patient compliance using strong cation exchange resin, Amberlite IRP 69.
Materials and Methods
Ranitidine HCl was gifted by Arti Drugs, Mumbai, Amberlite IRP 69 was the gift sample from Rohm Haas Ltd., France, Crosscarmellose sodium (Vivasol) was gifted by Rettenmair and Sohne, Germany and microcrystalline cellulose (Avicel PH 101) was the gift sample by FMC Biopolymer, Ireland). All the other chemicals used in the study were of analytical grade.
Preparation of resinate
Resinate (drug-resin complex) were prepared using batch method [4]. The resin was added to the drug solution in different ratios and kept on magnetic stirrer till equilibrium was achieved. Amount of drug loaded in the resin was determined indirectly by measuring the amount remaining to be loaded in the solution spectrophotometrically at 313 nm. Drug loading was done under different processing conditions such as temperatures (5, 10, 25, and 60o), pH (0.75, 1.0, 1.5, 2.7, 5.6, 8.2, 10), drug resin ratios (1:2, 1:1, 2:1, 3:1, 2:3), and drug concentrations (2, 4, and 6 mg/ml) [5] to get the optimum condition for the maximum loading of the drug on the resinate. Further study was done only on resinate with maximum drug loading and the batch for the study was prepared by first dissolving 24 g of ranitidine base (26.88g of ranitidine hydrochloride) in 4000 ml of deionised water having pH adjusted to 1.5 with hydrochloric acid at a concentration of 6.0 mg/ml. The solution was then stirred with 36g of resin using magnetic stirrer for about 2 h at a temperature of 10±2o . Resinate was separated by filtration, washed 3 times with deionised water and dried at 60o (±2o) to constant weight. Drug content was determined indirectly by estimating the amount of unloaded drug remaining in the solution spectrophotometrically at 313 nm. (Double beam UV/Vis spectrophotometer UVPC2401 PC, Shimadzu Corporation, Singapore).
X-ray diffraction studies
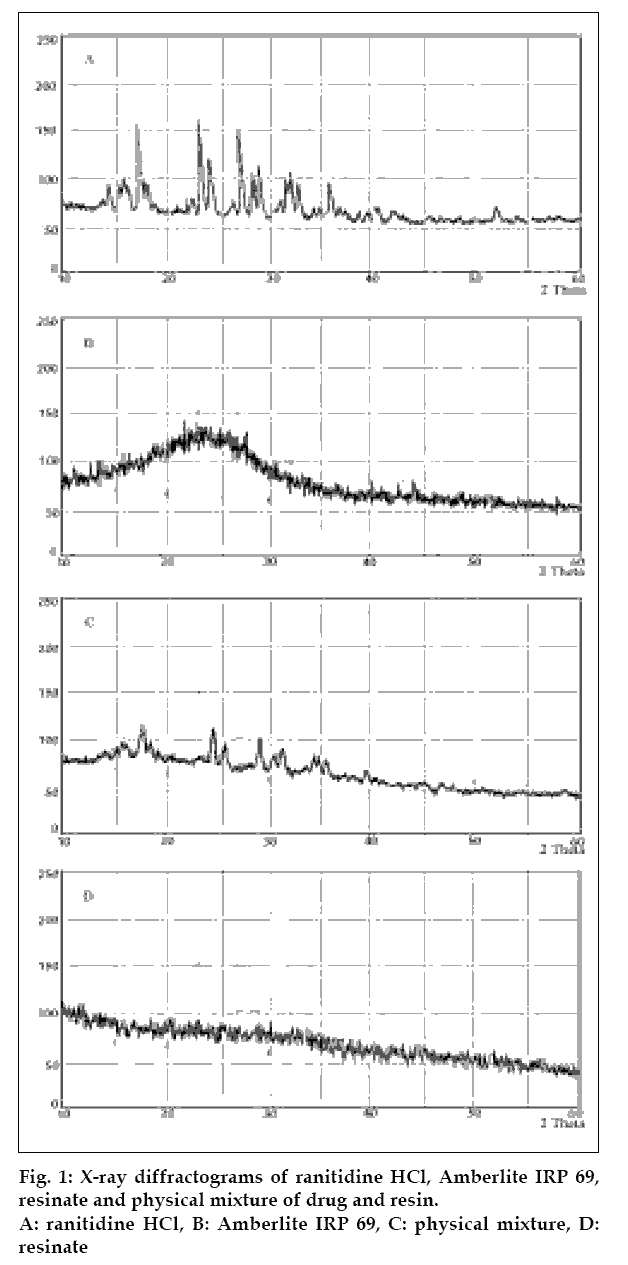
These studies were carried out to ascertain the formation of resinate. The X-ray diffractograms of ranitidine HCl, Amberlite IRP 69, physical mixture of ranitidine HCl with resin and resinate were obtained using X-ray diffractometer with Philips power generator with Cu Kα anode, 40 kv voltage and the current of 30 mA (fig. 1).
Drug content [5]
This study was carried out to determine the actual drug content per unit weight of the dry resinate. One hundred milligrams of resinate was stirred with 200 ml of 2 N NaCl for 2 h at 500-600 rpm on magnetic stirrer. The solution was replaced with a fresh 2 N NaCl solution (200 ml) and stirred for another 2 h and the procedure was repeated until no further drug was detected in solution. Total drug eluted was determined spectrophotometrically (313 nm). The drug content per 100 mg resinate is shown in Table 1.
| Particle size | Mean drug content (n=3)mg/100 mg resinate | +S.D. |
|---|---|---|
| Unaltered | 41.22 | 0.09 |
| < 75 µm | 41.97 | 0.11 |
| > 90 µm | 39.73 | 0.08 |
Table 1: Drug Content In Resinate Of Different Particle Size
Drug release in simulated salivary fluid (SSF)
Dissolution study of drug complex was done in SSF of pH 6.2 for an approximate estimation of drug release in the human saliva before doing actual volunteer study. Complex equivalent to 150 mg of ranitidine was taken in a 25-ml volumetric flask, to which 10 ml of SSF was added and shaken for 60 seconds on mechanical shaker. The amount of drug released was analyzed spectrophotometrically at 313 nm.
Taste evaluation
Taste evaluation was done by the time intensity method [6]. The sample equivalent to 150 mg ranitidine was held in the mouth of seven volunteers for 10 s. Bitterness was recorded immediately according to the bitterness intensity scale from 0 to 3; 3 being strongest, 2 being moderate, 1 being slight, 0.5 being threshold and 0 for no bitter taste. The readings were taken immediately and at several intervals over the period of 15 min (Table 2).
| Form of ranitidine HCl | Degree of bitterness after time | |||||
|---|---|---|---|---|---|---|
| 10 s | 1 min | 2 min | 5 min | 10 min | 15 min | |
| Pure drug | 3.00±0.51 | 2.86±0.53 | 2.57±0.55 | 2.14±0.25 | 1.14±0.34 | 1.00±0.54 |
| Resinate | 0.71±0.012 | 0.43±0.038 | 0.14±0.05 | 0 | 0 | 0 |
| Tablet | 0 | 0 | 0 | 0 | 0 | 0 |
Values are mean of seven observations ± SD
Table 2: Taste Evaluation Of Resinate
Bulk properties
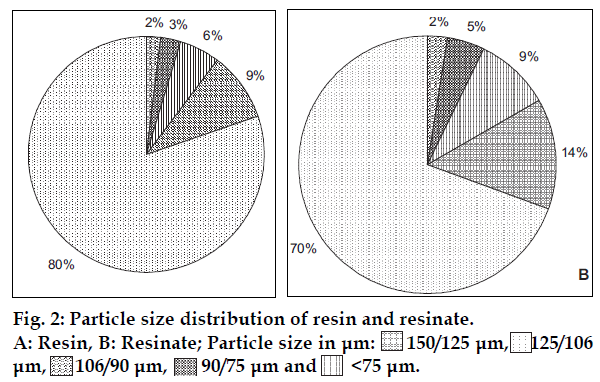
Pure drug, resin and resinate were evaluated for particle size distribution, bulk density, tapped density, compressibility index, Hausner ratio and angle of repose (fig. 2, Table 3).
| Physical property | Ranitidine HCl | Amberlite IRP 69 | Resinate |
|---|---|---|---|
| Bulk density (gm/cc) | 0.287±0.023 | 0.673±0.058 | 0.552±0.035 |
| Tapped density (gm/cc) | 0.403±0.085 | 0.925±0.056 | 0.698±0.067 |
| Compressibility index | 28.75±0.57 | 27.273±0.533 | 20.985±0.58 |
| Hausner ratio | 1.404±0.145 | 1.37±0.158 | 1.264±0.169 |
| Angle of repose (0) | 42.27±0.576 | 34.13±0.452 | 33.21±0.566 |
Results are the mean of three observations ± SD
Table 3: Comparison In Derived Properties Of Drug, Resin And Resinate
In vitro dissolution studies on resinate
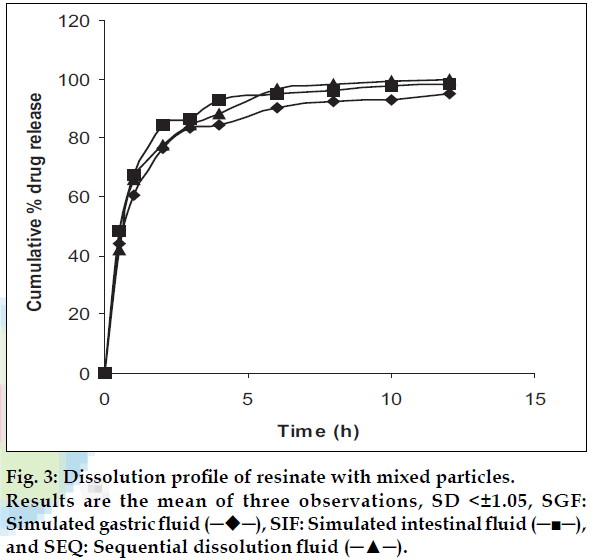
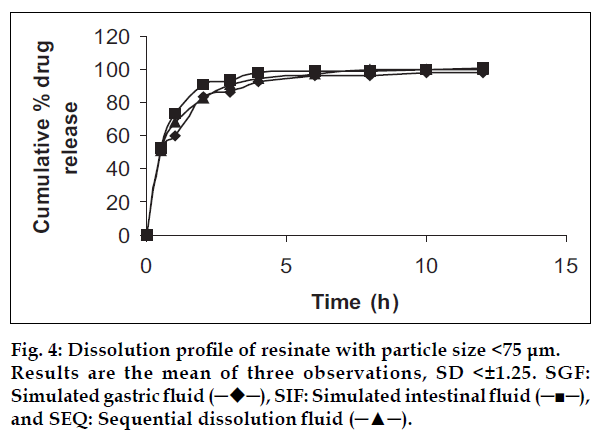
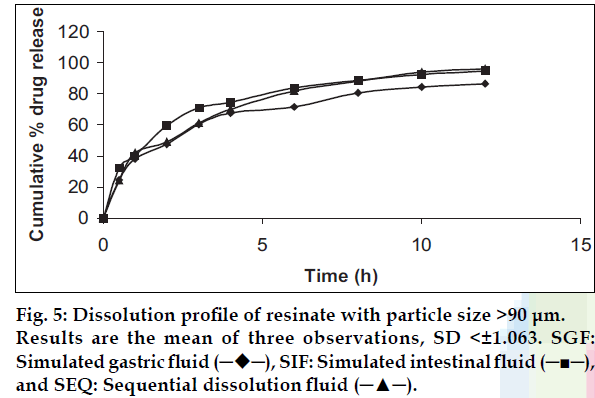
As per the particulate dissolution concept, particle size can be a useful tool to alter the dissolution rate of the drug. Hence this study was designed to learn if, the particle size alteration have the effect on rate of dissolution. Thus the study was conducted on resinates with different particle sizes i.e. <75 μm, >95 μm and resinate with mixed particles (without separation) in three dissolution media viz., simulated gastric fluid without enzymes (SGF), simulated intestinal fluid without enzymes (SIF) and sequential dissolution, for first 4 h in SGF and 8 h in SIF (figs. 3, 4 and 5). As a part of the same study, effect of different dissolution media on the rate and the extent of drug release were also studied. Dissolution study on resinate equivalent to one dose (156 mg ranitidine base calculated using formula for sustained release formulations) was carried out using USP dissolution apparatus (rotating paddle) with 900 ml of dissolution medium at 370.
Kinetics of release
The data obtained from dissolution studies were treated with different release equations for finding the mechanism and kinetics of release of Ranitidine HCl from ion exchange resin. Data was analyzed with following equations; first order release equation: Log Q = K1t, Higuchi’s square root of time equation: Q = KH t ½ and Korsmeyer Pappas equation: (Mt/M) = Km tn, where, Q is rate of drug release, Mt is drug released at time t and M the total amount of drug. K1and KH are first order and Higuchi square root of time-release rate constants. Km is a constant, which depends on the geometry of dosage form, and n is the diffusion exponent indicating the mechanism of release.
Comparison of the dissolution profile [7]
A simple model independent approach proposed by Moore in 1996 has got wide acceptance among regulatory bodies worldwide. It uses a difference factor (f1) and a similarity factor (f2) to compare dissolution profiles. The difference factor (f1) calculates the percent (%) difference between the two curves at each time point and is a measurement of relative error between the two curves;f1= {(Σt=1 n[Rt-Tt])/(Σt=1nRt)}×100, where n is the number of time points, Rt is the dissolution value of the reference batch at time t, and Tt is the dissolution value of the test batch at time t. The similarity factor (f2) is a logarithmic reciprocal square root transformation of the sum of squared error and is a measurement of similarity in the percent (%) dissolution between the two curves; f2 = 50×log{[1+(1/n)Σt=1 n(Rt-Tt)2]-0.5×100}. For curves to be considered similar, f1 values should be close to 0, and f 2 values should be close to 100. Generally, f1 values up to 15 (0 -15) and f2 values greater than 50 (50-100) ensure resemblance or equivalence of the two curves and thus, of the performance of the test and reference products. Factors f1 and f2 were used for assessing difference and similarity among dissolution profiles obtained with different dissolution media.
Formulation of orodispersible tablets
Resinate, MCC, aspartame and croscarmellose sodium (CCS) were mixed well than granulation was done using ethanol as a solvent for PVP-K30. Granules were dried at room temperature for 1 h followed by at about 50o for 15 min. in tray dryer. Two types of formulations were prepared, in one case (formulation B and D, Table 4) 50% of CCS was added during granulation while remaining 50% after granulation. However, in other two formulations (A and C) CCS was added once after the granulation. Granules were compressed using 12 mm standard concave punches on Cadmach single punch compression machine to the hardness of 4 to 5 kg/cm2. Tablets were tested for hardness, friability, weight variation, in vitro and in vivo disintegration time, taste (method similar to resinate particles, table 2) and in vitro release.
| Formulation | MCC(mg) | CCS(%) | Mode of CSS Incorporation | Resinate (mg) |
|---|---|---|---|---|
| A | 59.5 | 5 | E | 393 |
| B | 59.5 | 5 | I+E | 393 |
| C | 32.0 | 10 | E | 393 |
| D | 32.0 | 10 | I+E | 393 |
Formula per tablet PVR K-30 was added (60 mg per tablet) as binder aspartame and spearpoint added as sweetner and flavor, E: Extragranolar and I: Iotragranular
Table 4: Composition Of Orodispersible Tablets
Disintegration testing of orodispersible tablets
In vitro disintegration time was determined as described under procedure for uncoated tablets in USP. One tablet was placed in each of six tubes of the assembly. Apparatus was operated using water maintained at 37±2o as the immersion fluid. Time required for complete disintegration was noted for each tablet. Disintegration study in oral cavity was done on six healthy human volunteers, from whom informed consent was first obtained. After the mouth was rinsed with purified water, one tablet was held in the mouth and the time required for complete disintegration of tablet was recorded (Table 5).
| Formulation | A | B | C | D |
|---|---|---|---|---|
| Hardness kg/cm2, n=3 | 4.5±0.10 | 4.75±0.05 | 4.25±0.15 | 4.5±0.05 |
| Friability % | 0.25 | 0.11 | 0.39 | 0.28 |
| In vitro disintegration time (sec), n=6 | 71±1.41 | 82±2.00 | 31±1.47 | 30±1.47 |
| Disintegration time in oral cavity (sec), n=6 | 80±2.45 | 90±1.5 | 38±2.5 | 35±3.2 |
Results are mean±SD
In vitro drug release from tablets
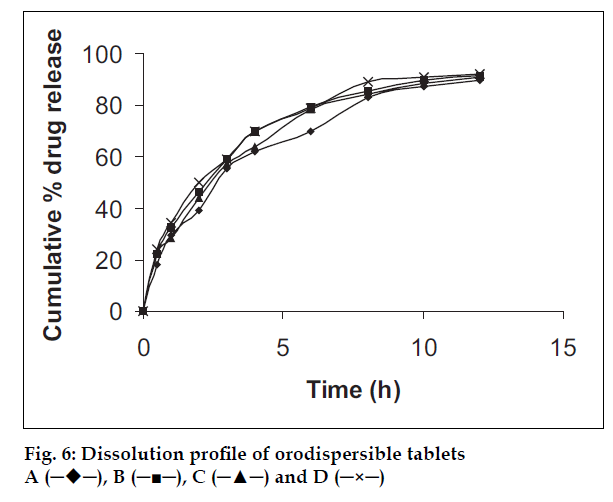
In vitro dissolution was carried out using USP paddle apparatus as described in previous section for dissolution of resinate. Dissolution was carried out in simulated gastric fluid without enzymes for first 4 h followed by 8 h in simulated intestinal fluid without enzymes (fig. 6).
Stability study
Optimized batch was tested for stability at 40o and 75% RH for the period of three months. Tablets were individually weighed and wrapped with aluminium foil and packed in black PVC bottle and put under above specified condition in humidity chamber for 6 months. After every month samples were analyzed for the in vitro drug release, weight gain and disintegration time.
Results and Discussion
All the parameters viz. temperature, pH, drug-resin ratio, and drug concentration affected either the rate or extent of loading of ranitidine HCl on Amberlite IRP 69. Temperature adversely affected the complexation, probably because of the decreased selectivity between the drug and binding sites on resin. This finding coincides with the report of Plazer-Vercammen8. Maximum drug loading was found at 10o. Higher drug loading per gram of the dry resin was found at lower pH values, specifically at pH 1.5. This suggests that the resin is bound to dimethylamino group, which is more ionized at lower pH values. Ranitidine has two pKa values, 8.2 and 2.7. A pKa of 8.2 is due to the dimethylamino group, which is expected to ionize at lower pH values. Lower loading was observed at higher pH values as less ionized drug might be available for complexation. Study on the effect of drug resin ratio suggests higher mg/g loading at a drug to resin ratio 1:1 and above; percent uptake of drug from solution was highest for the ratio 2:3. Drug concentration per ml of loading solution was found to affect the loading time and had no appreciable effect on the extent of uptake. Drug loading was faster at higher drug concentrations, probably because of efficient competition for binding sites with other ions in the solution. Thus higher drug concentration can be used to reduce the processing time and larger batches can be processed in relatively smaller vessels.
The XRD of the pure drug contained a number of sharp peaks, while the resin showed diffused peaks. The XRD of the physical dispersions showed simply the sum of the characteristic peaks of the pure drug and the diffused peaks of resin, whereas the characteristic peaks of the pure drug were found absent in X-ray diffractogram of the resinate regardless of presence of drug (fig. 1). Thus on the basis of diffractograms it can be said that the pure drug was crystalline and the resin was amorphous. However crystalline drug was found to convert into amorphous with monomolecular dispersion in resin as supported by the absence of peaks in resinate. These results coincide with those obtained by Akkaramongkolporn and co-workers [9] who studied change in molecular properties of propranolol upon binding with ion exchanger.
Only 1.5±0.26% drug release was observed in SSF from the drug-resin ratio 1:1. There was negligible release of drug from the complex because the pH of 6.2 and low cation concentration in the SSF were not able to break the drug-resin complex. This release was insufficient to impart taste as evidenced by the time intensity test for taste in human volunteers.
Time intensity study adopted for taste evaluation revealed considerable masking of the bitter taste of ranitidine HCl upon complexation with ion exchange resin, with the degree of bitterness just 0.71 after 10 s which ultimately reduced to 0 within 5 min only. These findings support a well-established property of ion exchange resin to mask the bitterness of amines [4,10,11].
Bulk properties including the flow of the drug were greatly improved as compared to the pure drug probably because of the monomolecular dispersion of the drug in free flowing resin beads, making resinate properties closely resembling that of the pure resin. Angle of repose of resinate (33.21o) was slightly superior to that of the resin (34.13o), probably due to the decreased percentage of fines (70%) in resinate as compared to the resin (80%), which is evident in fig. 3. Compressibility of resinate was found to improve as indicated by the low value of compressibility index (20.95) and Hausner ratio (1.263) as compared to the drug which showed compressibility index to be 28.75 and Hausner ratio equal to 1.404.
Dissolution of resinate in different media shows slightly faster dissolution in the simulated intestinal fluid without enzymes than simulated gastric fluid without enzymes, probably because of higher ionic strength of the intestinal fluid. Still these two dissolution profiles pass the test for similarity and can be considered equivalent as demonstrated by f1 (below 15) and f2 (above 50) factors. Effect of ionic strength of dissolution medium was also studied by Atyabi et al. [5] and found that the release rate of diclofenac from ion exchange resin increased with the increase in ionic strength of the dissolution media.
Particle size of resinate has tremendous impact on the dissolution rate, as more sustained release was observed with larger particles. There was a significant difference (P<0.05, based on Mann-Whitney, t test) in the dissolution profiles of resinate having <75 μm and that having >90 μm size. Along with cross-linking, particle size was reported to be an important factor in controlling the release of the drug from ion exchange resin by Burke et al [12]. Larger particle imposes hurdles in drug movement through the polymeric network requiring more time for deeply penetrated drug molecules to elute (fig. 5). Resinate with particle size >90 μm showed about 90% release in 12 h.
Mathematical treatment to the dissolution profiles shows first order release kinetics for resinate (R= 0.972, model selected by adopting F-test) with optimum particle size (>90 μm). Application of Korsmeyer Pappas equation to the data showed that the mechanism of release of ranitidine HCl from Amberlite IRP 69 matrix is governed by predominant Fickian diffusion (slope < 0.5).
Hardness and friability of all four formulations were within acceptable limits. The disintegration time was lowest for tablets with 10% croscarmellose sodium content (in vitro; 30 sec and in vivo; 35 sec). No appreciable difference was observed for both the modes of croscarmellose incorporation. Formulation D was selected as optimum and subjected to stability study. Orodispersible tablets were completely lacking bitter taste and were factually rated as pleasant due to presence of sweetening and flavoring agents. The dissolution profiles showed no appreciable difference with dissolution profile of resinate. Insignificant changes (p=0.9) in release profile and physical properties of formulation D was observed after stability study of 6 months.
In conclusion, taken together, it is concluded that strong cation exchange resin was successful in reducing the degree of bitterness of ranitidine HCl to zero and also improved the flow property of the drug, thus converting a drug to a form more convenient to process. This method of taste masking is very simple as compared to tedious and costly coating technique as it requires simple complexation followed by direct compression. Resinate with drug to resin ratio of 2/3 and particle size above 90 μm showed about 90% drug release after 12 h. Thus strong cation exchange resin can be used as a multifunctional excipient owing to its role in improving the physicochemical properties of ranitidine HCl and reducing the dosing frequency for better patient compliance.
Acknowledgements
Authors are thankful to R. S. I. C. Nagpur for XRD studies.
References
- Riley TN, DeRuiter J. In: Delgado N, Remers WA, editors., Wilson and Gisvold’s Textbook of Organic, Medicinal and Pharmaceutical chemistry, 10th ed. Lippincott–Raven: Philadelphia; 1998. p. 680.
- Drug Information for health care Professionals, Micromedex Thomson Healthcare, Englewood, Vol. I, 21st ed., 2001. p. 1659.
- Eyjolfsson, R., Drug Develop. Ind. Pharm., 2000, 26, 693.
- Avari, J.G. and Bhalekar, M., Indian Drugs, 2004, 41, 19.
- Atyabi, F., Koochak, M. and Dinarvand, R., J. Faculty Pharm., 2002, 10, 17.
- Borodkin, N. and Sundberg, P., J. Pharm. Sci., 1971, 60, 1523.
- Available from: http://www.fda.gov/cder/guidance.htm.
- Plaizier-Vercammen, J.A., Int. J. Pharm., 1992, 85, 45.
- Akkaramongkolporn, P., Terada, K. and Yonemochi, E., Drug Develop. Ind. Pharm., 2001, 27, 359.
- Borodkin, S. and Yunkar, M., J. Pharm. Sci., 1970, 59, 481.
- Fu Lu, M., Borodkin, S., Woodward, L., Li, P., Diesner, C., Hernandez, L. and Vadnere, M., Pharm. Res., 1991, 8, 706.
- Burke, M., Mendes, W. and Jambhekar, S., Drug Develop. Ind. Pharm., 1986, 12, 713.