- *Corresponding Author:
- S. Singh
Lovely School of Pharmaceutical Sciences, Lovely Professional University, Phagwara, Punjab, 144411, India
E-mail: saurabh.singh@lpu.co.in
| Date of Received | 22 December 2023 |
| Date of Revision | 26 June 2024 |
| Date of Acceptance | 24 December 2024 |
| Indian J Pharm Sci 2024;86(6):1958-1967 |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
Polycystic ovary syndrome is a diverse endocrine condition that affects approximately one in fifteen women worldwide. The excessive secretion of testosterone in females is the primary cause of the biggest endocrine disturbance and many women also experience unusual insulin activity. Polycystic ovarian syndrome affects several bodily functions, resulting in various health issues such as menstruation dysfunction, infertility, hirsutism, acne, obesity and metabolic syndrome. Women with this condition are more likely to develop type 2 diabetes and there is an increased risk of cardiovascular disease. The diagnostic characteristics of polycystic ovarian syndrome are hyperandrogenism, chronic anovulation, and polycystic ovaries after other illnesses that can cause similar symptoms have been ruled out. Various medicines are available in the market for the treatment of polycystic ovarian syndrome. To review this paper, different research engines such as Google Scholar, Science Direct and PubMed were utilized. Modern medicines for polycystic ovarian syndrome may alleviate symptoms, they do not address the root cause and may have negative side effects. To prevent recurrence, natural remedies and a healthy lifestyle are recommended for treatment. Polycystic ovaries syndrome can be corrected by using Ayurveda, Yoga and by adopting a balanced diet in our daily life. There is an important role of moonlight charged water also. 28 d that moon takes to revolve around sun is related with the 28 d of the menstrual cycle in females.
Keywords
Polycystic ovarian syndrome, polycystic ovarian disease, treatment with natural products, hyperandrogenism, infertility
Polycystic Ovary Syndrome (PCOS), is a condition that affects many young women. It is typically characterized by a combination of hyperandrogenism (an excess of male hormones) and chronic anovulation (a lack of ovulation) without any known underlying disorders of the pituitary or adrenal glands. This syndrome not only impairs fertility but also poses serious long-term health risks, including hormone imbalances, insulin resistance, metabolic syndrome, oxidative stress, chronic inflammation and epigenetic changes. These risks can lead to obesity, cardiovascular disease, diabetes, dermatological issues related to excess male hormones and potentially increased risk of cancer. While medications like metformin, antiestrogens and aromatase inhibitors are commonly used to treat PCOS and restore fertility, they do not address the other health risks associated with the condition and may cause unwanted side effects with long-term use.
Research has shown that 35 % of mothers and 40 % of sisters of patients with PCOS are likely to develop PCOS themselves. This indicates a higher risk of developing PCOS for adolescent sisters and daughters of women who have already been affected by this condition. Currently, the mode of inheritance of PCOS is not fully understood, as it may be more complex, similar to the cause of diabetes mellitus[1]. For some time, it has been established that ovarian hyperandrogenism is linked to conditions that are characterized by severe insulin resistance. However, in recent years, more attention has been given to women who have PCOS compared to those with traditional phenotypic disorders involving insulin resistance. Women with PCOS were found to have higher rates and intensities of hyperinsulinemia and insulin resistance when compared to weight-matched controls. Although impaired insulin sensitivity has been observed in both lean and obese women with PCOS, insulin resistance is more prominent in cases where there is a correlation between obesity and the disease. Hyperinsulinemia in women with PCOS appears to be caused by an increase in the production of insulin itself, rather than proinsulin and its split products[2].
Based on Ayurvedic beliefs, PCOS can be linked to Aarthava Kshaya. At the Osuki Ayurveda centre, a large number of subfertility patients were found to be suffering from PCOS. To evaluate the effectiveness of Ayurvedic treatment on subfertility caused by PCOS, a study was conducted. A total of 40 patients were chosen through purposive sampling. The treatment was conducted over 6 mo in three stages, according to the Ayurvedic principles of Shodhana, Shamana and Tarpana. The response to treatment was recorded and evaluated through symptomatic relief, Tran’s vaginal scan and Luteinizing Hormone (LH) and Follicle-Stimulating Hormone (FSH) hormone levels. The results showed that Ayurvedic treatment can successfully cure subfertility caused by PCOS[3].
Recent studies have shown that practising yoga can significantly improve the quality of life for adolescent females with PCOS. In one study, ninety teenage girls between the ages of 15-18 who met the Rotterdam criteria were randomly divided into two groups. The control group (n=35) engaged in complementary physical activities for 12 w, while the yoga group (n=37) participated in a holistic yoga program. After 12 w, the quality of life specific to PCOS was assessed. Results showed that the yoga program had a significant positive impact on improving the quality of life for adolescent females with PCOS. Recent studies have shown that practicing yoga can significantly improve the quality of life for adolescent females with PCOS. In one study, ninety teenage girls between the ages of 15-18 who met the Rotterdam criteria were randomly divided into two groups. The control group (n=35) engaged in complementary physical activities for 12 w, while the yoga group (n=37) participated in a holistic yoga program. After the 12 w, the quality of life specific to PCOS was assessed. Results showed that the yoga program had a significant positive impact on improving the quality of life for adolescent females with PCOS[4].
PREVALENCE
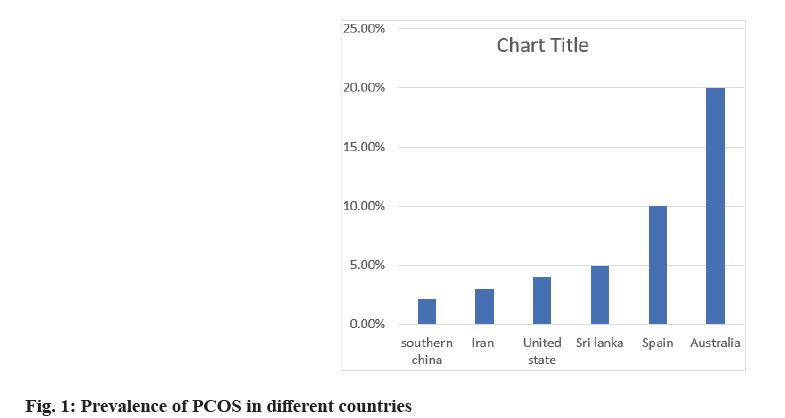
The prevalence of PCOS was observed to be 2.2 %, 3 % and 4 % in southern China, Iran and the United States, respectively. In Beijing, Palestine, Brazil, Sri Lanka, the United Kingdom (UK), Greece, and Spain, the prevalence rate ranged between 5 % and 10 %. However, the prevalence was higher (15 %-20 %) in Australia, Turkey, and Denmark. Different criteria being used resulted in varying prevalence rates. The Rotterdam criteria, which considers more extensive PCOS symptoms, such as polycystic ovaries and oligo or amenorrhea, is the most reliable diagnostic method. Studies that used the Rotterdam criteria as a diagnostic methodology reveal greater prevalence rates compared to the other two methodologies[5]. PCOS is a common condition that affects one out of every ten women globally in today's times. Before the late 1990s, there were limited studies on the prevalence of PCOS. You can find the prevalence of PCOS represented in Chart No. 1.
Materials and Methods
Academic search engines, Google Scholar, PubMed, and Scopus were utilized to find relevant literature. The databases were searched for terms related to PCOS, Cyst, infertility etc. This review study includes the benefits of Ayurvedic drugs, formulations and the use of yoga or a healthy lifestyle for treating PCOS.
The Root Cause of PCOS
PCOS occurs when the growth of a follicle in the ovarian cycle is disrupted due to a hormonal imbalance. As a result, the follicle does not rupture and release an egg, but instead remains inside the ovary and develops into cysts. This can occur multiple times in each reproductive cycle, hence the name "polycystic." In Ayurveda, any illness is considered an imbalance, and PCOS is categorized as a Kapha condition that affects the Aarthava dhatu organ and Artava vaha scrota passageway responsible for reproduction. When too much Kapha disrupts their normal flow, PCOS symptoms such as restricted movement, suppressed metabolism, and weight gain may arise. Poor nutrition and lifestyle choices, including mental stress, lack of exercise, and extended use of hormonal birth control pills, are the main causes of PCOS[4]. Numerous factors that are linked to obesity may have an impact on how well the hypothalamus and pituitary function.
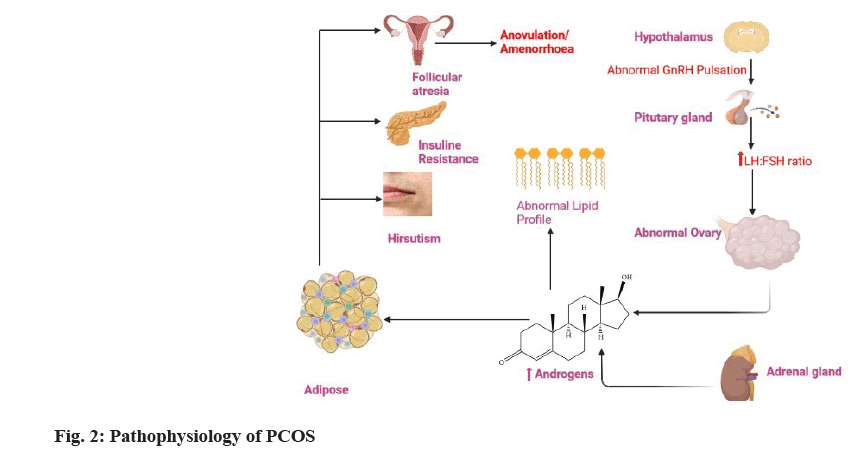
Research has found a connection between insulin resistance and/or hyperinsulinemia and issues with gonadotropin production in the hypothalamus. Obese mice with targeted insulin receptor pituitary knockouts showed restored and improved fertility, indicating a direct involvement of insulin action in PCOS. Although studying humans is difficult, there are other ways obesity can affect Hypothalamic-Pituitary-Ovarian (HPO) performance. Additionally, PCOS can also be induced by certain drugs, such as those used for epilepsy[6,7]. A study showed that 25 % of women with temporal lobe epilepsy also had PCOS, suggesting a link between the two conditions[8]. This finding supported a biological connection between the two diseases. In 1993, Isojarvi et al.[8] and colleagues presented the first scientific proof that the majority of reproductive-age women treated with Valproate (VPA) for epilepsy had PCOS and elevated testosterone blood levels, which are hallmarks of PCOS. The same results were also seen in a subset of Carbazepine-treated women, but to a lesser degree (CBZ). This study provided the novel idea that antiepileptic medication therapy may be more effective than epilepsy itself in treating. Pathophysiology is also discussed in fig. 1 and fig. 2.
Common Symptoms of PCOS
PCOS is a condition with various symptoms. It can cause irregular menstrual cycles, resulting in less frequent ovulation and either more or fewer periods. Some women with PCOS may not have periods at all for extended periods. Other symptoms include excess hair growth on the face or body, acne, hair loss, reduced fertility due to infrequent ovulation, and mood swings such as anxiety and despair[9]. Additionally, PCOS can lead to obesity, insulin sensitivity, and secondary disorders like miscarriage, elevated blood pressure, high cholesterol, type 2 diabetes or insulin resistance, and thyroid conditions. Ayurvedic treatment is available for PCOS.
Treatments of PCOS
Modern treatment:
Various medications can help increase insulin sensitivity, such as Metformin, which can enhance the body’s response to insulin. It can also reduce the production of glucose in the liver and improve glucose usage by muscles. Another medication, thiazolidinediones, like troglitazone, was taken off the market due to concerns about liver damage. Ovulation stimulants like clomiphene citrate can increase FSH levels in the blood, and gonadotrophins like LH and FSH can be used to treat PCOS, though overactive hyper stimulated syndrome may occur. Oral contraceptives can also help by suppressing LH and reducing androgen production[10]. Additionally, surgical methods like "wedge resection" of the ovaries have been linked to higher rates of ovarian and periadrenal adhesion, significant tissue loss, and premature ovaries[11].
Side effects of modern medicines:
If a woman is unable to ovulate naturally due to medical conditions like PCOS, clomiphene can be used to stimulate hormone release from the pituitary gland for inducing ovulation. However, it is not recommended for women with liver disease, abnormal vaginal bleeding, uncontrolled adrenal gland or thyroid disorders, or ovarian cysts not related to PCOS. Metformin and thiazolidinediones are two management strategies for metabolic disorders in women with PCOS. Metformin can cause gastrointestinal side effects, while thiazolidinediones are not recommended for non-diabetic women with PCOS due to potential cardiovascular side effects. Letrozole can be useful in PCOS as it reduces estrogen levels in postmenopausal women, inhibiting the development of some breast cancers that require estrogen to grow. Spironolactone is a diuretic that can be prescribed to treat hypokalaemia, hypertension, and heart failure, but it may cause symptoms of high potassium levels. For treating PCOS, ayurvedic medicine is a better alternative to modern medicines as it aims to balance a person’s overall health and capacity to recover from illness. The prakriti, which refers to a person's constitution, remains constant throughout their life and is affected by factors such as digestion and waste elimination. Table 1 displays the common side effects of modern medicines.
| S. no | Drugs | Dose | Side effects | Reference |
|---|---|---|---|---|
| 1 | Clomiphene | 50 mg | Bloating stomach or pelvic pain breast discomfort, uterine bleeding intermenstrual spotting menorrhagia | [13,14] |
| 2 | Letrozole | 2.5 mg | Bone fracture, arthralgia, oedema, Dizziness, Fatigue, Hypercholesterolemia osteoporosis and flushing | [13], [15] |
| 3 | Metformin. | 500 mg | Lactic acidosis, diarrhoea, nausea, vomiting and flatulence | [13] |
| 4 | Ethinyl estradiol | 0.15 mg to 1.5 mg | Heart attack, hypertension, Blood clot, swelling | [13] |
| 5 | Spironolactone | 50 mg per day to 100 to 200 mg per day | Hyperkalaemia, nausea, breast tenderness | [16] |
Table 1: Side Effect of Modern Medicines
PCOS Ayurvedic management:
Ayurveda offers a comprehensive approach to managing PCOS. The primary goal of individualized care is to cure the underlying cause of the disease and restore the body’s natural balance. The guidelines for Ayurvedic PCOS therapy include body detoxification with Ayurveda, strengthening and revitalizing the female reproductive system, correcting hormonal imbalances, and managing insulin resistance and obesity. Panchakarma is the primary line of treatment for PCOS. After a thorough assessment, an Ayurveda specialist creates a customized regimen. Panchakarma eliminates toxins from the reproductive system, including the uterus, ovaries, fallopian tubes, and vagina, addressing the underlying cause of the disease. Common techniques for panchakarma include Virechana (therapeutic purgation), Uttar vasti (uterovaginal enema), and vast (colonic enema). Once the panchakarma is complete, specific herbs and operations are used to revitalize and bring the female reproductive system into balance.
Ayurvedic medicines contain a substance called phytoestrogen, which has been proven to reduce insulin resistance and inflammation. It is important to have a balanced diet for overall health, as per the principles of Ahara and Vihar. Irregularities in diet can disrupt the doshas, leading to various gynaecological issues and infertility. It can also result in dhatu loss, affecting hormones and causing irregular periods. An unhealthy diet can hinder the implantation of a zygote and the nutrition of a fertilised egg. Weight loss can be achieved by following the principles of Ahara, Vihar, and Pathya/ apathy[10]. It is highly recommended to strictly follow the dincharya and ritucharya ways of living. The yoga poses listed below can aid in weight loss and lowering blood sugar levels, such as Kapalbhati, Mandukasan, and Anuloma-Viloma. Exercise, or vyayam, can increase muscle sensitivity to insulin, which accounts for 80 % of the body's glucose uptake. Aushadh, which are herbs like Gurmar, Jambu, Tarwar, and Guduchi, can reduce kapha, improve insulin, balance hormones, and eliminate obstructions. Early detection and ongoing management of PCOS are critical in preventing longterm problems. Ayurvedic recommendations for PCOS treatment include Virechana (Detoxification), Nasya, Shirodhara, and uttarbasti, as well as dietary and lifestyle changes. At Shathayu Ayurveda, we take a methodical approach to disease treatment and design a unique course of care for each patient based on their symptoms. There are various Ayurvedic formulations available for treating PCOS, including Basti. Women with amenorrhea, scanty menstruation, no ovulation or ineffective ovulation, or recurring abortion may benefit from Anuwasana basti. Yapana basti can aid infertile couples in becoming pregnant by performing both the cleansing and oleation procedures. There are various treatments available for ovarian cysts, such as guduchyadi rasayana basti and satvaryadi anuvasana basti. Kanchnar Guggulu contains katu-madhura rasa, usna virya, and katu vipaka, which can help reduce the size of cysts in the ovaries and prevent them from growing further by aiding in mama and medo dhatu lekhana.
The Ayurveda medicines and mixtures that help treat PCOS are Shatavari-Asparagus racemosus Crataeva Nurvala and Varuna Terminalia chebula, or haritaki, Piper longum-Pippali Aegle marmelos in Bilva, Premna integrifolia-Agni mantra, Punarvana is a kind of Boerhavia, Tinospora indicia, or guduchi, Plumbago zeylanica Chitraka, Sushmita-Ginger Ayurvedic remedy Punarvadi Kashaya, Shatavari Gulam Varunadi Kashaya, Chitrakadi Vati, Triphala Guggulu[1]. Being ruksh in guna, Kanchnar Guggulu and old Guggulu both reduce fat as a result of lekhan activity. They are, respectively, pitta-kapha shamak and vata-kapha shamak. Methi (fenugreek, Trigonella foenumgraecum) lowers blood sugar levels during fasting. Karela (bitter gourd, Momordica charantia) lowers fasting and postprandial blood sugar and appears to increase tissue sensitivity to insulin. Ashwagandha (Withania somnifera) eases the stress of amenorrhea and infertility. Shatawari (Asparagus racemosus) balances and strengthens the menstrual system. Marich (Black pepper, Piper nigrum), which contains a high amount of the antioxidant chromium picolinate (200-400 mcg/ day), can help to balance blood sugar levels. Classical Ayurvedic formulations are mentioned in Table 2[12-19] and Ayurvedic drugs are mentioned in Table 3.
| S. no. | Ayurvedic formulations | Compositions | Dose | Mechanism of action | Reference |
|---|---|---|---|---|---|
| 1 | Kanchnara Guggulu | Kanchanara, Shunthi , Marica , Pippali, Haritaki, Vibhitaki, Amalali, Varuna, Ela, Twak, Patra, Guggulu | 750 mg-1 gm | Detoxification | [12], [13] |
| 2 | Pushpadhanva Rasa | Ras sindhoor , Nag bhasma, Vanag bhasma and Loha bhasma, Abhrak bhasma and Bhavana dravya like Dhatura and Bhang etc. | 125 mg-250 mg | All the ingredients possess Deepan, Pachana, Swabhava- helps to correct aganimanda and amma formation thus by reliving Srotorodha | [12], [14] |
| 3 | Nashtapushpantaka Rasa | Rasendra,Gandhaka, loha, Vanga, Soubhagya, Rajata,Abhraka, Tamra, Daru, Jivanti, Kushta, Brihati, kakamachi, Nakta, Taleesa, vetragra, shvadamstra, Vrushaka, Bala, saindhava, Madhuka Danti,Lavanga,Vamshalochana, Rasna, Gokshurabeeja | 1-2 tablespoon once or twice | All the contents are ushna, so it helps to increases the digestive fire and the uttama ahararasa is generated so this leads to uttam dhatu utpatti | [12], [15] |
| 4 | Rajah Pravartani Vati | Aloe vera, Kaseesa, Tankana, Ramatha | 125 mg-250 mg | By reducing pain intensity and pain duration | [12], [16] |
| 5 | Aarogyavardhini Vati | Sudha parada, Sudha gandhaka, Loha bhasma, Abharaka bhasma, Tamra bhasma, Triphala, Shilajatu, Pura-Guggulu, Chitramool, Tikta, Neem swarasa | 500 mg-1 gm per day | It has styptic property and hence useful in arresting bleeding | [12], [17] |
| 6 | Chaturbeeja Choorna | Methika, Chandrashura, Kala ajaji, Yavanika | 1-2 gm | Chaturbeeja Churna has Snigdha Guna and Ushna Virya with Vata-Kaphahara Dosha-karma which pacified the vitiated Vata Dosha mainly due to Ushna Virya | [12], [18] |
| 7 | Varunadi Kashaya | Varuna, Sairyaka, Shatavari, Dahana, Morata, Biolwa, Vishanika, Brihati, Bhadra, karanja, pootikaranja, Jaya, Pathya, Bahalapallava, Darbha, Rujakara | 15-20 ml | Medanashanam, Gulmanashan | [12], [19] |
| 8 | Yogbasti with Pushpadhnva Rasa and Phalagrita | Puspadhanaya rasa: Ras sindhoor, Nag bhasma, Vanag bhasma and Loha bhasma, Abhrak bhasma and Bhavana dravya like Dhatura and Bhang etc. Phalagrita: Vacha, Manjista, Kushta, Tagra, Triphala ,Haritaki, Vibhitaki, Amla, Haridra, daruharidra, Madhuka, Meda, Dipyaka, Katukarohini, Payasya, Kakoli Vaijigandha, Shatavari, Hingu, Sharkara, Ghrita, Kshara | Half of kala basti | Nourishes the reproductive system and detoxifies it at the same time. | [19] |
| 9 | Triphla Kwatha | Amla, Vibhitaki, Haritaki | 10-20 ml | Reducing inflammation by reducing free radicals | [19] |
| 10 | Uttarbasti along with oral dugs like Ashoka, Manjistha etc. | Ashoka, Manjistha etc. | Uttar Basti to be given in urinary passage should be 750 ml. For Uttar Basti in vaginal passage the quantity should be ~1500 ml | It removes the blockage of tubal lumen by directly acting on obstruction mechanically and restores the normal function of tubal cilia by stimulating | [19] |
Table 2: Classical Ayurvedic Formulations
| S. no. | Drugs | Botanical name | Family | Part used | Mechanism of action |
|---|---|---|---|---|---|
| 1 | Fennel | Foeniculum vulgare | Umbelliferae | Seeds | Bring down inflammation and control insulin resistance. |
| 2 | Guduchi | Tinospora cordifolia | Menispermaceae | Stem | Revitalizing body tissues and lowering insulin resistance. |
| 3 | Aloe vera | Aloe barbadensis | Liliaceae | Leaf Pulp | Regularizing menstrual cycles and promote normal menstruation. It also normalizes hormonal imbalance. |
| 4 | Shatavari | Asparagus racemosus | Asparagaceae | Tuberous roots. | Helps in controlling high levels of insulin due to PCOS, due to its phytoestrogen or natural plant-based estrogen levels. |
| 5 | Shatapushpa | Anethum sowa Kurz | Umbelliferae | Aromatic leaves and seeds | Helps to grow eggs naturally and helps to split follicles naturally. |
| 6 | Kachanar | Bauhinia variegata | Fabaceae | Bark and Flower | Balance Kapha and promotes the healthy function of Agni (digestive fire) because of its Kapha balancing nature. Altogether, it helps improve the function of the ovaries. |
| 7 | Guggulu | Commiphora mukul | Burseraceae | Oleo gum resin | Guggul contains plant steroids that lower cholesterol and triglycerides. One of these substances also decreases the redness and swelling |
| 8 | Meshshringi | Gymnema sylvestre | Asclepiadaceae | Leaves and extracts | Reduction in absorption of glucose, stimulation of pancreatic beta cell growth and insulin release from beta cells Beta cell supplementation |
| 9 | Haridra | Curcuma longa | Zingiberaceae | Rhizome | It act as blood purifier and anti-inflamatory agents. |
| 10 | Karela | Momordica charantia | Cucurbitaceae | Fruit and seeds | It is rich in vitamin C. It enhances sensitivity of body tissue for insulin. |
| 11 | Maricha | Piper nigrum | Piperaceae | Seeds and fruits | It is use full in treating Colon toxins, prolonged indigestion and Gastric problems |
| 12 | Yastimadhu | Glycyrrhiza glabra | Fabaceae | Root | Metabolism of androgen and it has been found that the block of 17-hydroxysteroid dehydrogenase and of 17-20 lipase will trigger serum testosterone reduction. Thus, hirsutism and PCOS profit from liquorice |
| 13 | Yastimadhu | Glycyrrhiza glabra | Fabaceae | Root | Metabolism of androgen and it has been found that the block of 17-hydroxysteroid dehydrogenase and of 17-20 lipase will trigger serum testosterone reduction. Thus, hirsutism and PCOS profit from liquorice |
| 14 | Jatamansi | Nardostachys jatamansi | Valerianaceae | Roots and the rhizomes | Shows antiandrogenic effect |
Table 3: Ayurvedic Drugs for PCOS
Dietary Advice for PCOS
Losing weight by making dietary and lifestyle changes, as well as incorporating exercise, can lead to decreased testosterone levels, increased insulin sensitivity, reduced hyperinsulinemia, improved menstrual cycles, and enhanced fertility. Avoid consuming artificial sweeteners and sugary foods, and limit salt intake during menstruation. Increase your consumption of fruits and vegetables and opt for whole grains, which contain the entire grain. Non-vegetarians can choose protein-rich foods like fresh salmon, organic chicken, and organic eggs. To maintain healthy blood glucose levels, include whole grains and legumes in your diet. To improve your health, it's important to limit your intake of saturated fats. These fats can be found in deep-fried foods, chicken, red meat, and commercially prepared snacks. It’s also crucial to manage your stress levels, as stress can throw your hormones out of balance. Avoid consuming foods high in saturated fat and refrain from napping after meals or during the day. Additionally, make sure to drink plenty of water-aim for 1.5 to 2 l of filtered water each day to keep your body hydrated. It’s recommended to exercise moderately for 45 min every day, incorporating pranayama exercises that involve alternating nasal breathing, pilates for PCOS, and yoga to tone your reproductive system. Women can also benefit from moonlight charged water on an empty stomach and practising poses such as Dhanurasana, Uttanpadasana, Badhakonasana, Ushtrasana, vrikshasana, and Vajrasana to establish a regular and healthy menstrual cycle. By engaging in these daily practices, including the butterfly stretch and pranayama, women can balance their hormones and improve their overall health. A low carbohydrate diet is helpful for those with PCOS. The Glycemic Index (GI) is a measure of how quickly carbohydrates and sugars in food are broken down and absorbed into the bloodstream. Foods that cause a rapid and significant increase in blood sugar have a high GI, while those that cause a slower, smaller increase have a lower GI. Table 4 provides information on the carbohydrate and GI levels of different foods.
| Food group | Low GI | Intermediate GI | High G |
|---|---|---|---|
| Fruit and vegetables | Apple, dried apricots, grapes, berries, salad, orange, Vegetables | Bananas, melon, raisins, sultanas | Watermelon, parsnips, pumpkin, swede, dates |
| Milk and dairy | Milk and yoghurts | Ice cream | |
| Breakfast cereals | Porridge, Oatibix, Allbran, Natural, Muesli | Weetabix, Puffed and Shredded Wheat, Bran flakes | Rice Krispies, Coco, Pops, cornflake |
| Breads | Multigrain, granary, heavy fruit loaf, chapattis | Pitta bread, rye and wholemeal bread, Ryvita | White bread, bagels, French’s |
| Grains and pulses | Beans, lentils, chickpeas | Couscous, mille | |
| Snack foods | Banana cake, popcorn, nuts and seeds, chocolate (especially dark), oatcakes | Muffins, digestives, rich tea, crisps, rice cakes | All sweets, morning coffee biscuits, doughnut, iced cakes, wafers |
Table 4: Dietary Advice for PCOS
Exercise
In the practice of yoga, Patanjali outlined eight steps or limbs that are all equally important. These steps include Yama, which focuses on self-regulation, Niyama for practice, Asana for meditation posture, Pranayama for breath control and expansion, Pratyahara for sensory withdrawal, Dharana for concentration, Dhyana for meditation, and Samadhi for achieving a higher state of meditation. Incorporating yoga into your routine can greatly aid in managing PCOS, diabetes, hypertension, and thyroidism. This holistic approach to health can assist in preventing future health concerns. Moreover, yoga is a cost-effective and long-term solution that can work alongside traditional medical care. Ultimately, practicing yoga can help improve your cardiovascular and respiratory function and support you in managing any health issues you may have.
There are various ways to practice yoga, with different types of asanas that can be beneficial for PCOS. Some examples include 10 min of Surya Namaskara (Sun Salutation), poses like Cobra Pose (Bhujangasana) and Bow Pose (Dhanurasana), and standing asanas. Each asana should be done for 1 min. Additionally, pranayama exercises like Kapal Bhati, Relaxing Pose like Savasana for 10 min, and meditation by pronouncing OM can also help with improving the state of PCOS. It would be beneficial for schools, colleges, and universities to provide yoga education to prevent girls from suffering from problems like PCOS. Yoga can also assist with other health problems. The Table 5 provides a list of exercises.
| S. no. | Exercise | Age group | Time period | Benefits | References |
|---|---|---|---|---|---|
| 1 | Butterfly pose | Child -old | 1 min | Build muscle strength, prevent obesity, and grow healthy reproductive organs | [18] |
| 2 | Dhanurasan (Bow pose) | Adult | 1 min | Obesity, and grow healthy reproductive organs | [18] |
| 3 | Balasana | Adult | 1 min | Maintain health | [18] |
| 4 | Bhujanga asana (Cobra Pose) | Adults | 1 min | Good for joints | [18] |
| 5 | Chakichalanasana | Child-adult | 1 min | Good for muscles | [18] |
| 6 | Locust Pose (Salabhasana) | Child-adult | 1 min | Maintained of health | [19] |
| 7 | Parsva-konasana (Twisted angle pose ) | Child-adult | 1 min | Maintained of health | [19] |
| 8 | Halasana (Plough pose) | Child-adult | 1 min | Make body flexible | [19] |
| 9 | Malasana(Garland pose) | Child-adult | 1 min | Maintained of health | [19] |
| 10 | Baddha-konasana (fixed angle Pose) | Child-adult | 1 min | Make body elastic and flexible | [19] |
TABLE 5: EXERCISE FOR PCOS
Conclusion
PCOS is a condition where the ovaries produce high levels of androgens (male hormones) such as testosterone. This results in increased levels of LH and decreased levels of FSH. This causes the follicles to not produce a mature egg, leading to irregular menstruation and anovulatory cycles. Early diagnosis and long-term management of PCOS are necessary to prevent future complications. Ayurvedic treatment for PCOS includes Virechana (Detoxification), Nasya, Shirodhara and Uttar Basti along with diet and lifestyle modifications. Shathayu Ayurveda provides a personalized treatment plan based on individual symptoms to effectively treat PCOS.
Conflict of interest:
The authors declared no conflict of interests.
References
- Kahsar-Miller MD, Nixon C, Boots LR, Go RC, Azziz R. Prevalence of Polycystic Ovary Syndrome (PCOS) in first-degree relatives of patients with PCOS. Fertil Steril 2001;75(1):53-8.
[Crossref] [Google Scholar] [PubMed]
- Rojas J, Chávez M, Olivar L, Rojas M, Morillo J, Mejías J, et al. Polycystic ovary syndrome, insulin resistance, and obesity: Navigating the pathophysiologic labyrinth. Int J Reprod Med 2014;2014(1):719050.
[Crossref] [Google Scholar] [PubMed]
- Siriwardene SD, Karunathilaka LA, Kodituwakku ND, Karunarathne YA. Clinical efficacy of Ayurveda treatment regimen on Subfertility with PCOS. Ayu 2010;31(1):24-7.
- Nidhi R, Padmalatha V, Nagarathna R, Amritanshu R. Effect of yoga program on quality of life in adolescent polycystic ovarian syndrome: A randomized control trial. Appl Res Quality Life 2013;8:373-83.
- Deswal R, Narwal V, Dang A, Pundir CS. The prevalence of polycystic ovary syndrome: A brief systematic review. J Hum Reprod Sci 2020;13(4):261-71.
[Crossref] [Google Scholar] [PubMed]
- Legro RS. Obesity and PCOS: Implications for diagnosis and treatment. Semin Reprod Med 2012;30(6):496-506.
[Crossref] [Google Scholar] [PubMed]
- Herzog AG, Seibel MM, Schomer D, Vaitukaitis J, Geschwind N. Temporal lobe epilepsy: An extrahypothalamic pathogenesis for polycystic ovarian syndrome? Neurology 1984;34(10):1389-93.
[Crossref] [Google Scholar] [PubMed]
- Isojarvi J, Laatikainen TJ, Pakarinen AJ, Juntunen K, Myllyla VV. Polycystic ovaries and hyperandrogenism in women taking valproate for epilepsy. New Engl J Med 1993;329(19):1383-8.
[Crossref] [Google Scholar] [PubMed]
- Tomlinson JA, Pinkney JH, Evans P, Millward A, Stenhouse E. Screening for diabetes and cardiometabolic disease in women with polycystic ovary syndrome. Br J Diabetes Vasc Dis 2013;13(3):115-23.
- Mishra D, Sinha MU. Ayurvedic management of polycystic ovarian syndrome (infertility Queen). J Res Educ Indian Med 2008;14(1):33-40.
- Stein IF, Leventhal ML. Amenorrhea associated with bilateral polycystic ovaries. Am J Obstetr Gynecol 1935;29(2):181-91.
- Sharma P, Sharma U, Sharma S. An effort to understand PCOS in Ayurveda context. Infertility 2016;3(2):630-3.
- Deshpande D, Asokan V. A Review on Pushpadhanva Rasa in Vandhyatva (Anovulatory Factor of Infertility). World J Pharm Life Sci 2019;5(8):221-4.
- Pal S, Ramamurthy A, Mahajon B. Arogyavardhini Vati: A theoretical analysis. J Sci Innov Res 2016;5(6):225-7.
- Khot BM, Chikhale VR. A clinical study to evaluate the efficacy of yogbasti and yogbasti with herbo mineral compounds in the management of PCOS. World J Pharm Res 2015;4(8):1634-40.
- Savita R. Magdum Vijaykumarswamy G, Hiremath A. Conceptual review on a unique pancha karma therapy Uttar Basti. Eur J Pharm Med Res 2021;8(1):2394-3211.
- Monika K, Bhawana B, Daulatkar KK, Polycystic Ovarian Syndrome: management with Ayurvedic prospective, Int J Res Indian Med 2021;5(4):2456-4435.
- Ravina Y, Ashish M. Comparative study of Vamana-Virechana Karma and Kanchnar Guggulu in management of polycystic ovarian syndrome. JETIR 2022;9(3):2349-5162.
- Kalleian EA, Eserian JK, Garcia YM, Cavalcanti MR, Suen KP, Bhavanani AB, et al. Clinical roundup: selected treatment options for depression. Altern Complement Ther 2014;20(1):52-9.