- *Corresponding Author:
- Zhenxing Wang
Department of Cardiovascular Medicine, Affiliated Hospital of Nanjing University of Chinese Medicine, Hanzhong, Nanjing 210023, China
E-mail: 202050092@njucm.edu.cn
| This article was originally published in a special issue, “Emerging Therapeutic Interventions of Biopharmaceutical Sciences” |
| Indian J Pharm Sci 2024:86(3) Spl Issue “254-262” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
To investigate the effects of irbesartan hydrochlorothiazide combined with recombinant human brain natriuretic peptide on cardiac function, immune function and intestinal flora in subjects with acute heart failure. 100 subjects with acute heart failure admitted to our hospital from March 2021 to March 2022 were divided into 50 subjects in each group according to different intervention methods. The monotherapy group was handled with conventional therapy, and the combination therapy group was handled with irbesartan hydrochlorothiazide combined with recombinant human brain natriuretic peptide, clinical efficacy, cardiac function, serum myocardial enzymes, cardiac troponin I, immunological functioning, change of intestinal flora and adverse reactions in two groups were contrasted. The monotherapy group vs. the total effective rate of the combination therapy group was higher (92.00 % vs. 74.00 %) (p<0.05). The monotherapy group vs. left ventricular ejection fraction in the combination therapy group was notably higher (p<0.05). Left ventricular end diastolic diameter, left ventricular end systolic diameter and serum creatine kinase, creatinine kinase myocardial band, aspartate transaminase, lactate dehydrogenase, troponin I levels were notably lower than those in the monotherapy group (p<0.05). Comparing the intestinal flora of the two groups, the abundance of Bacteroides in the combination therapy group was notably increased vs. the monotherapy group (p<0.05). The abundance of Fusobacterium, Actinomyces, Proteus and Firmicutes was notably lower than that of the monotherapy group (p<0.05). There was no notable difference in the incidence of adverse reactions between the two groups (p>0.05). Irbesartan hydrochlorothiazide combined with recombinant human brain natriuretic peptide can improve the therapeutic effect of acute heart failure, improve the subject’s cardiac function, reduce the myocardial injury, improve the body immunity, and regulate the intestinal flora structure, so as to promote the subject’s recovery.
Keywords
Heart failure, irbesartan hydrochlorothiazide, recombinant human brain natriuretic peptide, cardiac function, immunity, intestinal flora
Heart failure is a clinical syndrome caused by abnormal cardiac structure and (or) function, including chronic heart failure and acute heart failure, of which the latter is more critical, and is one of the main reasons for subjects over 65 y old to stay in hospital[1,2]. According to the report[3], the incidence rate of heart failure among people over 35 y old in China is about 1.3 %, which has increased in recent years, bringing heavy disease burden to the country. The main clinical manifestations of acute heart failure are pulmonary congestion/edema, decreased cardiac output, hypoperfusion of tissues and organs, and even cardiogenic shock, respiratory failure, etc.,[4,5]. The early therapy of acute heart failure is mainly to stabilize hemodynamics, correct hypoxia and maintain organ perfusion. Later, symptomatic therapy is carried out according to the etiology. Common drugs include vasodilators, diuretics, positive inotropic drugs, etc., but the effect is average[6].
Irbesartan hydrochlorothiazide is a new type of angiotensin II receptor antagonist, in which hydrochlorothiazide can activate renin-angiotensin system and sympathetic nervous system, reduce blood pressure level while lowering blood potassium; irbesartan has strong diuretic effect, quickly corrects symptoms of heart failure, and is mainly used for the therapy of hypertension[7]. Subjects with heart failure were accompanied by increased plasma B-Type Natriuretic Peptide (BNP). Studies have shown that recombinant human Brain Natriuretic Peptide (rhBNP) can play a series of effects after binding with its receptor, such as expanding blood vessel, reducing blood pressure, filling left ventricle and maintaining heart function effectively. It can be used alone or in combination[8,9]. In addition, a study has shown that irbesartan can regulate body immunity and improve vascular endothelial function[10]. BNP has immunomodulatory function in unidirectional mixed lymphocyte reaction[11]. Recent study has found that there are many links between intestinal microbiota and their metabolites and immune system[12]. At the same time, the changes of intestinal flora in patients with cachexia will lead to the disturbance of intestinal barrier function, resulting in the increase of bacterial toxin translocation and systemic inflammation[13]. A study has found that heart failure is closely related to changes in intestinal flora, but the specific mechanism is unknown[14].
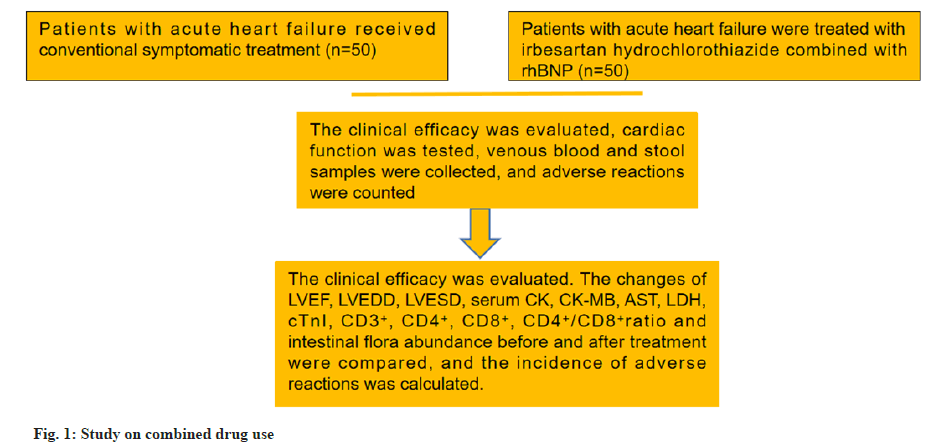
In view of this, this study took subjects with acute heart failure as the research object, to explore the therapeutic effect of irbesartan hydrochlorothiazide combined with rhBNP and its influence on the heart function, immune function and intestinal flora of subjects as shown in fig. 1.
Materials and Methods
General information:
This was a double-arm cohort trial with repeated measurements from March 2021 to March 2022. In this retrospective analysis trial, the eligibility and exclusion criteria of subjects were evaluated according to the inclusion situation. After screening, the participants were assigned according to the intervention method. This study was approved by Nanjing University of Chinese Medicine Ethics Committee (Approval No: 2023-KY-106-02).
Inclusion criteria: The age was 18 y to 80 y; conformed to the diagnostic criteria related to acute heart failure[15], and it was left heart failure; New York Heart Association (NYHA) classification ≥grade II and the clinical data was complete.
Exclusion criteria: Patients with other types of heart failure or congenital heart disease; patients with severe liver and kidney dysfunction; patients with concurrent severe infection or blood system disease; patients with malignant tumors; patients with severe neurological disease and patients who did not tolerate the therapy drug.
Therapy methods:
The monotherapy group was given routine symptomatic therapy such as mask oxygen inhalation, Electrocardiogram (ECG) monitoring, cardiotonic therapy, diuresis, etc. The combination therapy group added irbesartan hydrochlorothiazide tablets (GYZZ H20058709, Zhejiang Huahai Pharmaceutical Co., Ltd., irbesartan 150 mg+hydrochlorothiazide 12.5 mg/tablet, Zhejiang, China) and rhBNP (GYZZ S20050033, Chengdu Nordicam Biopharmaceutical Co., Ltd., 0.5 mg/500 U/bottle, Chengdu, China). Irbesartan hydrochlorothiazide tablets were taken orally. The dose was 162.5 mg/time and 1 time/d. RhBNP was injected intravenously with 1.5 μg/ kg dose, completed in 3~5 min, and then pumped continuously according to 7.5 ng/(kg/min) for 3 d-7 d.
Observation indicators:
Cardiac function: The cardiac function of the subjects was tested by color Doppler ultrasound (Philips iu22, Amsterdam, Netherlands). The indexes include Left Ventricular Ejection Fraction (LVEF), Left Ventricular End Diastolic Diameter (LVEDD), and Left Ventricular End Systolic Diameter (LVESD).
Serum myocardial enzymes and cardiac Troponin I (cTnI) levels: 5 ml of venous blood was collected before and after therapy, and serum samples and cell samples were collected after centrifugation. The levels of serum Creatine Kinase (CK), CKMyocardial Band (CK-MB), Aspartate Transaminase (AST), Lactate Dehydrogenase (LDH) and cardiac cTnI were detected with an automatic biochemical analyzer (Hitachi 7020, Prang Medical, Beijing, China).
Immunological functioning: The above cell samples were selected, and the levels of Cluster of Differentiation 3+ (CD3+), CD4+, and CD8+ were detected by flow cytometry, and the ratio of CD4+/ CD8+ was calculated[16].
Change of intestinal flora: The stool samples of subjects before and after therapy were collected, and the fecal bacteria Deoxyribonucleic Acid (DNA) were extracted. Bacteroides, Fusobacterium, Actinomycetes, Proteus and Firmicutes were detected by gene sequencing.
Adverse reactions: The adverse reactions such as hypotension and headache were compared between the two groups.
Efficacy evaluation criteria:
Remarkable effect: The clinical symptoms and signs basically disappeared vs. those before therapy, and the improvement level of cardiac function ≥grade II or recovered to grade I. In effective, the clinical symptoms and signs are relieved vs. those before therapy, and the improvement grade of cardiac function was grade I. In ineffective, the clinical symptoms and signs were not improved or aggravated vs. those before therapy, and the cardiac function grade was not improved.
Remarkable efficiency+effective efficiency=total effective efficiency
Data statistics:
Statistical Package for the Social Sciences (SPSS) 24.0 software (IBM, Amonk, New York, United States of America (USA)) was selected as the analysis software to analyze the data. The measurement data conformed to the normal distribution and had the same variance. It was described by (x±s) and tested by t-value. Counting data were described by (n, %) and tested by Chi-square (χ2)/Fisher exact probability method. The standard of statistically notable difference was p<0.05.
Results and Discussion
There were 26 males and 24 females with the age of 51 y~78 y, average (67.25±7.39) y. In NYHA classification; 11 cases of grade II, 25 cases of grade III and 14 cases of grade IV; in past medical history; 17 cases of hypertension, 8 cases of coronary heart disease and 13 cases of diabetes. In monotherapy group; 28 males and 22 females were there and age was 48 y~79 y, average (68.31±7.55) y; NYHA classification with 14 cases of grade II, 24 cases of grade III, 12 cases of grade IV. In past medical history; 15 cases of hypertension, 10 cases of coronary heart disease and 12 cases of diabetes. There were no significant differences in general data between the two groups (p>0.05) (Table 1).
| sdfa | Combination therapy group | Monotherapy group | χ2/t | p |
|---|---|---|---|---|
| Gender | ||||
| Male | 26 | 28 | 0.161 | 0.288 |
| Female | 24 | 22 | ||
| Age | 67.25±7.39 | 68.31±7.55 | 0.709 | 0.479 |
| NYHA classification | ||||
| Grade II | 11 | 14 | 0.534 | 0.765 |
| Grade III | 25 | 24 | ||
| Grade IV | 14 | 12 | ||
| Past medical history | ||||
| Hypertension | 17 | 15 | 2.45 | 0.294 |
| Coronary heart disease | 8 | 10 | ||
| Diabetes | 13 | 12 | ||
Table 1: General Information in Two Groups
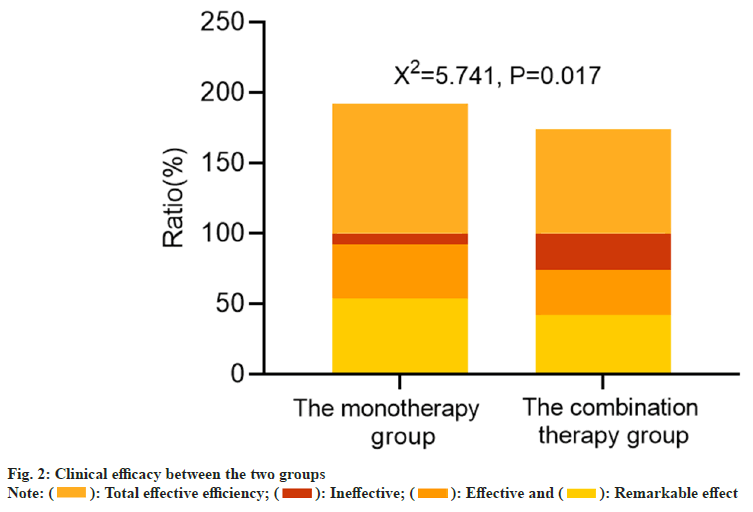
In the combination therapy group, the ineffective rate was 8.00 %, whereas 26.00 % in the monotherapy group vs. the total effective rate of the monotherapy group (74.00 %), the total effective rate of the combination therapy group (92.00 %) was higher (p<0.05). As corroborated in Table 2 and fig. 2.
| Category | n | Remarkable effect | Effective | Ineffective | Total effective efficiency |
|---|---|---|---|---|---|
| Combination therapy group | 50 | 27 (54.00) | 19 (38.00) | 4 (8.00) | 46 (92.00) |
| Monotherapy group | 50 | 21 (42.00) | 16 (32.00) | 13 (26.00) | 37 (74.00) |
| χ2 | 2.885 | 3.099 | 11.481 | 5.741 | |
| p | 0.089 | 0.078 | <0.001 | 0.017 |
Table 2: Clinical Efficacy (N, %)
Before therapy, there was no difference in LVEF, LVEDD and LVESD between the two groups (p>0.05). After therapy, the LVEF in both groups were higher than baselines with statistical significances, LVEDD and LVESD were lower (all p<0.05) as shown in Table 3.
| Category | n | LVEF (%) (mm) | LVEDD (mm) | LVESD (mm) | |||
|---|---|---|---|---|---|---|---|
| Before therapy | After therapy | Before therapy | After therapy | Before therapy | After therapy | ||
| Combination therapy group | 50 | 36.59±6.45 | 47.03±7.25a | 61.58±9.43 | 51.74±7.81a | 56.35±8.11 | 48.87±6.50a |
| Monotherapy group | 50 | 36.71±6.30 | 41.86±7.34a | 62.01±9.22 | 55.96±8.04a | 55.79±8.35 | 52.61±6.77a |
| t | 0.094 | 3.543 | 0.231 | 2.662 | 0.340 | 2.818 | |
| p | 0.925 | 0.001 | 0.818 | 0.009 | 0.734 | 0.006 | |
Note: ap<0.05 vs. the same group before therapy. In the combination therapy group, LVEF ap<0.001, LVEDD ap<0.001 and LVESD ap<0.001. In the monotherapy group, LVEF ap<0.001, LVEDD ap<0.001 and LVESD ap=0.039
Table 3: Cardiac Function Indexes (X̄±S)
Before therapy, there was no difference in serum CK, CK-MB, AST, LDH and cTnI levels between the two groups (p>0.05). After therapy, the above indexes in both groups were lower than baselines with statistical significances (all p<0.05). And the decrease in the combination therapy group was greater (p<0.05) as shown in Table 4.
| Category | n | CK (U/l) | CK-MB (U/l) | AST (U/l) | LDH (U/l) | cTnI (ng/ml) | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Before therapy | After therapy | Before therapy | After therapy | Before therapy | After therapy | Before therapy | After therapy | Before therapy | After therapy | ||
| Combination therapy group | 50 | 220.15±30.42 | 134.88±15.70a | 14.63±1.97 | 8.29±1.53a | 53.68±7.20 | 29.01±4.56a | 308.57±48.31 | 168.33±32.64a | 0.24±0.07 | 0.11±0.03a |
| Monotherapy group | 50 | 221.67±31.82 | 195.26±18.30a | 14.55±2.08 | 10.86±2.24a | 52.79±7.34 | 36.45±5.39a | 310.20±50.15 | 217.63±41.75a | 0.25±0.08 | 0.16±0.05a |
| t | 0.244 | 17.707 | 0.197 | 6.699 | 0.612 | 7.452 | 0.166 | 6.578 | 0.665 | 6.063 | |
| p | 0.808 | <0.001 | 0.844 | <0.001 | 0.542 | <0.001 | 0.869 | <0.001 | 0.508 | <0.001 | |
Note: ap<0.05 vs. the same group before therapy. In the combination therapy group, CK ap<0.001, CK-MB ap<0.001, AST ap<0.001, LDH ap<0.001 and cTnI ap<0.001. In the monotherapy group, CK ap<0.001, CK-MB ap<0.001, AST ap<0.001, LDH ap<0.001 and cTnI ap<0.001
Table 4: Levels of Serum Myocardial Enzymes and cTni (X̄±S)
Before therapy, there was no difference in CD3+, CD4+, CD8+ and CD4+/CD8+ ratio between the two groups (p>0.05). After therapy, CD3+, CD4+, CD8+ and CD4+/CD8+ ratio in both groups were higher than baselines with statistical significances, CD8+ was lower (all p<0.05). And the change range of the combination therapy group was greater (p<0.05) as shown in Table 5.
| Category | n | CD3+ (%) | CD4+ (%) | CD8+ (%) | CD4+/CD8+ | ||||
|---|---|---|---|---|---|---|---|---|---|
| Before therapy | After therapy | Before therapy | After therapy | Before therapy | After therapy | Before therapy | After therapy | ||
| Combination therapy group | 50 | 48.26±4.31 | 56.74±6.48a | 32.85±3.54 | 38.41±3.80a | 28.01±2.56 | 22.45±1.92a | 1.17±0.30 | 1.71±0.35a |
| Monotherapy group | 50 | 49.55±4.22 | 53.14±6.05a | 32.29±3.38 | 35.94±3.61a | 27.83±3.40 | 25.37±2.16a | 1.16±0.32 | 1.42±0.33a |
| t | 1.512 | 2.871 | 0.809 | 3.332 | 0.299 | 7.145 | 0.161 | 4.263 | |
| p | 0.134 | 0.005 | 0.421 | 0.001 | 0.766 | <0.001 | 0.872 | <0.001 | |
Note: ap<0.05 vs. the same group before therapy. In the combination therapy group, CD3+ ap<0.001, CD4+ ap<0.001, CD8+ ap<0.001 and CD4+/CD8+ ap<0.001. In the monotherapy group, CD3+ ap<0.001, CD4+ ap<0.001, CD8+ ap<0.001 and CD4+/CD8+ ap<0.001
Table 5: Immune Function Indexes (X̄±S)
Before therapy, there was no difference in the abundance of intestinal flora between the two groups (p>0.05). After therapy, the abundance of intestinal Bacteroides in both groups were higher than baselines with statistical significances, the abundance of Fusobacterium, Actinomyces, Proteus and Firmicutes was lower (all p<0.05). And the change range of the combination therapy group was more notable (p<0.05) (Table 6).
| Category | n | Bacteroides | Fusobacterium | Actinomyces | Proteus | Firmicutes | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Before therapy | After therapy | Before therapy | After therapy | Before therapy | After therapy | Before therapy | After therapy | Before therapy | After therapy | ||
| Combination therapy group | 50 | 28.74±3.15 | 45.86±6.20a | 0.93±0.18 | 0.72±0.13a | 14.36±2.90 | 6.53±1.74a | 8.73±1.59 | 6.39±1.20a | 63.15±5.78 | 29.36±4.15a |
| Monotherapy group | 50 | 28.26±3.30 | 33.08±4.27a | 0.95±0.17 | 0.84±0.15a | 14.22±2.75 | 10.05±1.96a | 8.80±1.55 | 7.26±1.44a | 63.40±6.03 | 48.95±4.27a |
| t | 0.744 | 12.004 | 0.571 | 4.275 | 0.248 | 9.497 | 0.223 | 3.282 | 0.212 | 23.264 | |
| p | 0.459 | <0.001 | 0.569 | <0.001 | 0.805 | <0.001 | 0.824 | 0.001 | 0.833 | <0.001 | |
Note: ap<0.05 vs. the same group before therapy. In the combination therapy group, Bacteroides ap<0.001, Fusobacterium ap<0.001, Actinomyces ap<0.001, Proteus ap<0.001 and Firmicutes ap<0.001. In the monotherapy group, Bacteroides ap<0.001, Fusobacterium ap<0.001, Actinomyces ap<0.001, Proteus ap<0.001 and Firmicutes ap<0.001
Table 6: Abundance of Intestinal Microflora (X±S, %)
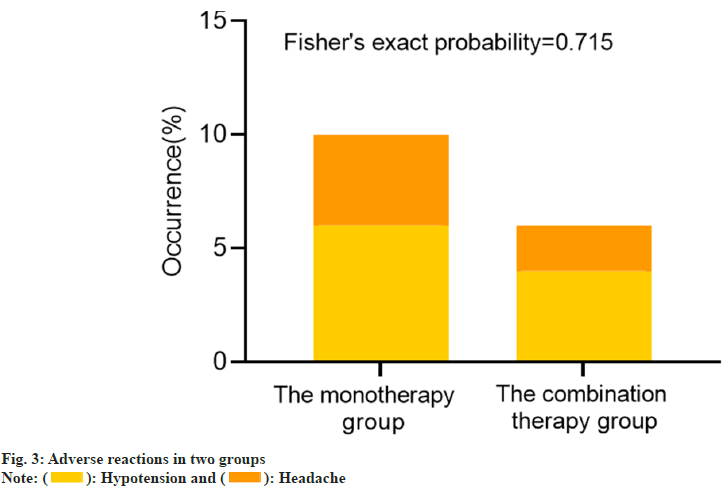
During the therapy, 3 subjects in the combination therapy group had hypotension, 2 subjects had headache symptoms, and the incidence of adverse reactions was 10.00 % (5/50). In the monotherapy group, there were 2 cases of hypotension and 1 case of headache, respectively. The incidence of adverse reactions was 6.00 (3/50). The comparison between groups corroborated that there was no difference in the incidence of adverse reactions (Fisher’s exact probability=0.715) (fig. 3).
The vast majority of cardiovascular diseases will eventually develop into heart failure, and its prevalence rate will increase year by year with the growth of age. With the aggravation of the aging process in China, heart failure has become an important disease burden in China, seriously affecting the development of society[17,18]. There are many inducements for heart failure, such as myocardial injury, heart valve disease, mechanical obstruction, excessive resistance or volume load, etc. Among them, acute myocardial ischemia, acute poisoning, acute heart valve dysfunction, severe infection, etc., are the main causes of acute left heart failure, while acute right heart failure is relatively rare in clinical practice[19]. For acute left heart failure, the clinical therapy strategy is to evaluate the respiratory, circulatory and conscious state and provide supportive therapy[20].
The results of this study corroborated that the total effective rate of the combination therapy group was notably higher than that of the monotherapy group, and LVEF of the combination therapy group was notably higher than that of the monotherapy group, LVEDD and LVESD were notably lower than that of the monotherapy group, it shows that irbesartan hydrochlorothiazide combined with rhBNP can improve the clinical efficacy of acute left heart failure, reduce cardiac load and improve cardiac function. Based on the pathological characteristics of acute heart failure, diuretics, positive inotropic drugs and vasodilators are mainly used in clinical therapy, which can alleviate the symptoms of heart failure and stabilize the condition, but the prognosis is not notably beneficial[21]. Obviously, conventional supportive therapy can no longer meet the needs of subjects with acute heart failure. Elevated BNP level is a recognized plasma marker for clinical diagnosis of heart failure. The study shows that BNP is mainly synthesized by cardiomyocytes and stored in myocardial secretory granules in the form of precursors[22]. Once the ventricular wall tension increases and the myocardium is damaged, it will be released, some of which will be decomposed into active BNP and the other into inactive N-terminal BNP, resulting in an increase in plasma BNP concentration, and the more serious the degree of heart failure, the higher the BNP concentration. On the other hand, BNP has the effects of diuresis, vasodilation, natriuretic, inhibition of sympathetic nerve and renin-angiotensin-aldosterone system, and can be used in the therapy of heart failure[23]. Previous studies have confirmed that intravenous drip of rhBNP can improve the clinical symptoms of subjects and reduce the risk of rehospitalization in subjects with short-term heart failure[24,25]. As a compound preparation, irbesartan hydrochlorothiazide has the dual effects of irbesartan and hydrochlorothiazide, which cannot only dilate blood vessels and reduce ventricular wall tension, but also resist hypotension and reduce blood potassium level[26]. rhBNP combined with irbesartan and hydrochlorothiazide can play a synergistic therapeutic effect, and the effect is more notable. Myocardial zymogram and cTnI are serum markers for evaluating myocardial injury[27]. In this study, the lower levels of serum CK, CK-MB, AST, LDH and cTnI in the combination therapy group also corroborated that the combination of them was more effective in the therapy of acute heart failure, which could improve the cardiac function of subjects and promote the recovery of myocardial injury.
Through the analysis of the incidence characteristics of heart failure in the elderly, this disease is related to the deterioration of cardiovascular structure and function, or to the decrease of immune function[28]. In recent years, more and more evidence shows that the immune system plays an important role in the occurrence and development of heart failure. Abnormal T cell subsets can cause ventricular remodeling and aggravate the process of heart failure[29]. Intestinal microflora refers to microorganisms living in human intestine, including beneficial bacteria, harmful bacteria and neutral bacteria. Under normal circumstances, their number and types are in dynamic balance. If the balance is damaged, many diseases will occur, including heart failure[30,31]. This study found that after therapy, the CD3+, CD4+, CD4+/CD8+ ratio and the abundance of Bacteroides in the combination therapy group were notably higher than those in the monotherapy group, while CD8+, the abundance of Fusobacterium, Actinomyces, Proteus and Firmicutes was notably lower than that in the monotherapy group. It is suggested that irbesartan hydrochlorothiazide combined with rhBNP can improve immune function and regulate intestinal flora balance in subjects with acute heart failure. Inflammatory response is another important mechanism leading to heart failure. rhBNP and irbesartan hydrochlorothiazide can reduce the inflammatory response, and their immune enhancement effect on the body may be related to reducing the expression of proinflammatory factors[32,33]. Yu et al.[34] have suggested that the synthesis and secretion of adhesion molecules and chemokines in subject’s body with coronary heart disease complicated with heart failure increased. Probiotic intervention can regulate intestinal flora, increase myocardial hypoxia tolerance, increase cardiac output, reduce inflammation. It also suggests that reducing inflammation can improve intestinal flora[35]. In this study, it was found that there was no difference in the incidence of adverse reactions between the two groups, indicating that the combination of drugs had higher safety, which was consistent with the results of previous safety studies[36,37].
To sum up, for subjects with acute heart failure, the combination of irbesartan hydrochlorothiazide and rhBNP is more effective on the basis of routine therapy, which can improve subject’s cardiac function, increase body immune function, and regulate the balance of intestinal flora, which is worthy of clinical application. However, the number of cases in this study is small, the observation time is short, and the specific mechanism of heart failure and intestinal flora has not been discussed, which needs to be demonstrated by large sample size and multicenter research.
Irbesartan hydrochlorothiazide combined with rhBNP can improve the therapeutic effect of acute heart failure, improve the subject’s cardiac function, reduce the myocardial injury, improve the body immunity, and regulate the intestinal flora structure, so as to promote the subject’s recovery.
Conflict of interests:
The authors declared no conflict of interests.
References
- Wang X. Incidence and prevention of chronic diseases in China: Literature review in the last 5 years. Int J General Pract 2022;1:57-70.
- McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Bohm M, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur J Heart Failure 2021;42(36):3599-726.
[Crossref] [Google Scholar] [PubMed]
- Hao G, Wang X, Chen Z, Zhang L, Zhang Y, Wei B, et al. Prevalence of heart failure and left ventricular dysfunction in China: The China hypertension survey, 2012-2015. Eur J Heart Fail 2019;21(11):1329-37.
[Crossref] [Google Scholar] [PubMed]
- Mueller C, McDonald K, de Boer RA, Maisel A, Cleland JG, Kozhuharov N, et al. Heart failure association of the European society of cardiology practical guidance on the use of natriuretic peptide concentrations. Eur J Heart Fail 2019;21(6):715-31.
[Crossref] [Google Scholar] [PubMed]
- Roberts E, Ludman AJ, Dworzynski K, Al-Mohammad A, Cowie MR, McMurray JJ, et al. The diagnostic accuracy of the natriuretic peptides in heart failure: Systematic review and diagnostic meta-analysis in the acute care setting. BMJ 2015;350:h910.
[Crossref] [Google Scholar] [PubMed]
- Kurmani S, Squire I. Acute heart failure: Definition, classification and epidemiology. Curr Heart Fail Rep 2017;14(5):385-92.
[Crossref] [Google Scholar] [PubMed]
- Price S, Platz E, Cullen L, Tavazzi G, Christ M, Cowie MR, et al. Expert consensus document: Echocardiography and lung ultrasonography for the assessment and management of acute heart failure. Nat Rev Cardiol 2017;14(7):427-40.
[Crossref] [Google Scholar] [PubMed]
- Fang J, Zeng W. A meta-analysis of the clinical efficacy of rhBNP in treating patients with acute myocardial infarction and heart failure. Am J Transl Res 2021;13(4):2410.
[Google Scholar] [PubMed]
- Moura B, Aimo A, Al-Mohammad A, Flammer A, Barberis V, Bayes-Genis A, et al. Integration of imaging and circulating biomarkers in heart failure: A consensus document by the biomarkers and imaging study groups of the heart failure association of the European society of cardiology. Eur J Heart Fail 2021;23(10):1577-96.
[Crossref] [Google Scholar] [PubMed]
- Zhou T, Huang X, Cai X, Xie L. Combined treatment of irbesartan and diltiazem ameliorates endothelium dependent vasodilatation in hypertensives. Clin Exp Hypertens 2017;39(7):612-8.
[Crossref] [Google Scholar] [PubMed]
- de Bold ML, Etchepare A, Martinuk A, de Bold AJ. Cardiac hormones ANF and BNP modulate proliferation in the unidirectional mixed lymphocyte reaction. J Heart Lung Transpl 2010;29(3):323-6.
[Crossref] [Google Scholar] [PubMed]
- Zhou B, Yuan Y, Zhang S, Guo C, Li X, Li G, et al. Intestinal flora and disease mutually shape the regional immune system in the intestinal tract. Front Immunol 2020;11:575.
[Crossref] [Google Scholar] [PubMed]
- Gao J, Guo X, Wei W, Li R, Hu K, Liu X, et al. The association of fried meat consumption with the gut microbiota and fecal metabolites and its impact on glucose homoeostasis, intestinal endotoxin levels, and systemic inflammation: A randomized controlled-feeding trial. Diabetes Care 2021;44(9):1970-9.
[Crossref] [Google Scholar] [PubMed]
- Feng SJ, Yang S, Lin HT, Li M, Ran LJ, Xin YY. Enhancement of the denitrification in low C/N condition and its mechanism by a novel isolated Comamonas sp. YSF15. Environ Pollut 2020;256:113294.
[Crossref] [Google Scholar] [PubMed]
- Heart failure group of cardiology branch of Chinese medical association, heart failure professional committee of Chinese medical doctor association, and editorial committee of Chinese journal of cardiology Chinese guidelines for diagnosis and therapy of heart failure 2018. Chin J Heart Fail Cardiomyopathy 2018;46(10):760-89
- Batra A, Smith AC, Feehally J, Barratt J. T-cell homing receptor expression in IgA nephropathy. Nephrol Dialysis Transpl 2007;22(9):2540-8.
[Crossref] [Google Scholar] [PubMed]
- Pratima, Sharm M. Application of medical big data in clinical medicine. Int J Gen Pract 2023;3(4):241-55.
- Upadhya B, Kitzman DW. Heart failure with preserved ejection fraction: New approaches to diagnosis and management. Clin Cardiol 2020;43(2):145-55.
[Crossref] [Google Scholar] [PubMed]
- Pivetta E, Goffi A, Nazerian P, Castagno D, Tozzetti C, Tizzani P, et al. Lung ultrasound integrated with clinical assessment for the diagnosis of acute decompensated heart failure in the emergency department: A randomized controlled trial. Eur J Heart Fail 2019;21(6):754-66.
[Crossref] [Google Scholar] [PubMed]
- Zeymer U, Bueno H, Granger CB, Hochman J, Huber K, Lettino M, et al. Acute cardiovascular care association position statement for the diagnosis and treatment of patients with acute myocardial infarction complicated by cardiogenic shock: A document of the acute cardiovascular care association of the European society of cardiology. Eur Heart J Acute Cardiovasc Care 2020;9(2):183-97.
[Crossref] [Google Scholar] [PubMed]
- Messina A, Longhini F, Coppo C, Pagni A, Lungu R, Ronco C, et al. Use of the fluid challenge in critically ill adult patients: A systematic review. Anesth Analg 2017;125(5):1532-43.
[Crossref] [Google Scholar] [PubMed]
- Torres-Courchoud I, Chen HH. B-type natriuretic peptide and acute heart failure: Fluid homeostasis, biomarker and therapeutics. Rev Clin Esp 2016;216(7):393-8.
[Crossref] [Google Scholar] [PubMed]
- Streb W, Mitręga K, Szymała M, Podolecki T, Kalarus Z. Usefulness of N-terminal-pro B-type natriuretic peptide as a heart failure marker in patients undergoing percutaneous left atrial appendage occlusion. Kardiol Pol 2018;76(1):166-72.
[Crossref] [Google Scholar] [PubMed]
- Starling RC, Hernandez AF, Armstrong PW, Dickstein K, Gennivois D, Hasselblad V, et al. Clinical outcomes at 180 days in the ASCEND-HF trial: Double-blind, placebo-controlled, multicenter acute study of clinical effectiveness of nesiritide in subjects with decompensated heart failure. J Cardiac Fail 2011;17(11):971.
[Crossref] [Google Scholar] [PubMed]
- Feng X, Wu Y, Meng Y, Wei Y. Efficacy and safety of intravenous recombinant human brain natriuretic peptide in patients with severe heart failure: A prospective multicenter clinical study. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue 2017;29(6):520-4.
[Google Scholar] [PubMed]
- Ma XG, Wang WQ, Wu SL. Clinical Observation of irbesartan hydrochlorothiazide combined with sodium nitroprusside for injection in the therapy of acute heart failure. J Chengde Med Univ 2021;38(4):298-301.
- Grodin JL, Butler J, Metra M, Felker GM, Voors AA, Mcmurray JJ, et al. Circulating cardiac troponin I levels measured by a novel highly sensitive assay in acute decompensated heart failure: Insights from the ASCEND-HF trial. J Cardiac Fail 2018;24(8):512-9.
[Crossref] [Google Scholar] [PubMed]
- Li SJ. Advances in epidemiology, pathophysiology and prognosis of senile heart failure. Chin J Geriatr Cerebrovasc Dis 2021;23:318-20.
[Crossref] [Google Scholar] [PubMed]
- Dharmarajan K, Dunlay SM. Multimorbidity in older adults with heart failure. Clin Geriatr Med 2016;32(2):277-89.
[Crossref] [Google Scholar] [PubMed]
- Zile MR, Baicu CF, S. Ikonomidis J, Stroud RE, Nietert PJ, Bradshaw AD, et al. Myocardial stiffness in patients with heart failure and a preserved ejection fraction: Contributions of collagen and titin. Circulation 2015;131(14):1247-59.
[Crossref] [Google Scholar] [PubMed]
- Triplett OA, Xuan J, Foley S, Nayak R, Tolleson WH. Immunomagnetic capture of big six Shiga toxin-producing Escherichia coli strains in apple juice with detection by multiplex real-time PCR eliminates interference from the food matrix. J Food Protection 2019;82(9):1512-23.
[Crossref] [Google Scholar] [PubMed]
- Yang H, Song Z, Jin H, Cui Y, Hou M, Gao Y. Protective effect of rhBNP on intestinal injury in the canine models of sepsis. Int Immunopharmacol 2014;19(2):262-6.
[Crossref] [Google Scholar] [PubMed]
- Li Q, Huang Y, Liu P, Yuan H, Zhao J. Effect of Tripterygium wilfordii polyglycoside tablets on serum inflammatory factors and T cells in patients with chronic nephritis. Am J Transl Res 2021;13(7):8385.
[Google Scholar] [PubMed]
- Yu H, Dong AQ, Zhao Y. Changes in intestinal flora in patients with coronary heart disease and heart failure and effects of probiotics interventions. Mil Med Sci 2021;45(6):443-8.
- Kim SK, Guevarra RB, Kim YT, Kwon J, Kim H, Cho JH, et al. Role of probiotics in human gut microbiome-associated diseases. J Microbiol Biotechnol 2019;29(9):1335-40.
[Crossref] [Google Scholar] [PubMed]
- Mebazaa A, Motiejunaite J, Gayat E, Crespo-Leiro MG, Lund LH, Maggioni AP, et al. Long-term safety of intravenous cardiovascular agents in acute heart failure: Results from the European society of cardiology heart failure long-term registry. Eur J Heart Fail 2018;20(2):332-41.
[Crossref] [Google Scholar] [PubMed]
- Li L, Liang X. Effect of metoprolol combined with irbesartan hydrochlorothiazide on BNP and LVEF in elderly patients with severe heart failure. Chin Clin Med J 2020;48(2):152-5.