- *Corresponding Author:
- P. V. Swamy
Department of Pharmaceutics, H. K. E. Society’s College of Pharmacy, Sedam Road, Gulbarga - 585 105, India
E-mail: vspadavala@rediffmail.com
| Date of Submission | 21 August 2006 |
| Date of Revision | 5 July 2007 |
| Date of Acceptance | 18 December 2007 |
| Indian J Pharm Sci, 2007, 69 (6): 836-840 |
Abstract
In the present work, orodispersible tablets of meloxicam were designed with a view to enhance patient compliance. A combination of super-disintegrants i.e., sodium starch glycolate- croscarmellose sodium or sodium starch glycolate-crospovidone were used along with directly compressible mannitol to enhance mouth feel. The prepared batches of tablets were evaluated for hardness, friability, drug content uniformity, wetting time, water absorption ratio and in vitro dispersion time. Based on in vitro dispersion time (approximately 10 s), two formulations (one from each batch) were tested for in vitro drug release pattern (in pH 6.8 phosphate buffer), short-term stability (at 45º for 3 w) and drug-excipient interaction (IR spectroscopy). Among the two formulations, the formulation prepared by direct compression method using 2% w/w sodium starch glycolate and 1.5% w/w croscarmellose sodium was found to be a better formulation (t 50% = 22 min) based on the in vitro drug release characteristics compared to conventional commercial tablet formulation (t 50% = 68 min). Short-term stability studies on the formulations indicated that there are no significant changes in drug content and in vitro dispersion time (P<0.05).
Keywords
Orodispersible tablets, meloxicam, sodium starch glycolate, crospovidone, croscarmellose sodium
Many patients express difficulty in swallowing tablets and hard gelatin capsules, tending to non-compliance and ineffective therapy [1]. Recent advances in novel drug delivery systems (NDDS) aim to enhance safety and efficacy of drug molecules by formulating a convenient dosage form for administration and to achieve better patient compliance. One such approach is orodispersible tablet [1-4]. Advantages of this drug delivery system include administration without water, accuracy of dosage, easy portability, alternative to liquid dosage forms, ideal for pediatric and geriatric patients and rapid onset of action. Meloxicam is an oxicam or enol carboxamide derivative. It is a nonsteroidal antiinflammatory drug (NSAID) with highly selective cyclo-oxygenase-2 (COX-2) inhibitory action. It is used in the treatment of rheumatoid arthritis, osteoarthritis, dental pain, and in the management of acute post-operative pain [5,6]. It was selected as drug candidate, as it is not available in such dosage form. Aim of the present study was to develop such a NDDS for meloxicam by simple and cost-effective direct compression technique.
Meloxicam and super-disintegrants were gift samples from Sun Pharma, Mumbai and Wockhardt Research Centre, Aurangabad, respectively. Directly compressible mannitol (Pearlitol SD200) was a generous gift from Strides Arcolabs, Bangalore. Microcrystalline cellulose (Loba Chemie Pvt. Ltd., Mumbai), colloidal silicon dioxide (Yucca Enterprises, Mumbai), magnesium stearate (CDH, Mumbai) were used. All other chemicals used were of Analytical Reagent grade.
Orodispersible tablets of meloxicam were prepared by direct compression [7] according to the formulae given in Table 1. All the ingredients were passed through #60 mesh separately. Then the ingredients were weighed and mixed in geometrical order and tablets were compressed using 8 mm normal concave punches to get tablets of 200 mg weight on a 16-station rotary tablet machine (Cadmach). A batch of 60 tablets was prepared for all the designed formulations.
| Ingredients (mg/tablet) | Formulation code | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| DC0 | DCC1 | DCC2 | DCC3 | DCC4 | DCC5 | DCP1 | DCP2 | DCP3 | DCP4 | DCP5 | |
| Meloxicam | 7.5 | 7.5 | 7.5 | 7.5 | 7.5 | 7.5 | 7.5 | 7.5 | 7.5 | 7.5 | 7.5 |
| Sodium pstarchglycolate | - | 2 | 4 | 8 | 12 | 16 | 2 | 4 | 8 | 12 | 16 |
| Cros-carmellose sodium | - | 2 | 3 | 4 | 5 | 6 | - | - | - | - | - |
| Cros-povidone | - | - | - | - | - | - | 6 | 6 | 8 | 8 | 8 |
| Pearlitol SD 200 | 20 | 20 | 20 | 20 | 20 | 20 | 20 | 20 | 20 | 20 | 20 |
| Aerosil | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| Magnesium stearate | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Sodium saccharin | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Flavour | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 4 |
| Micro- crystalline | |||||||||||
| cellulose | 164.5 | 160.5 | 157.5 | 152.5 | 147.5 | 142.5 | 156.5 | 154.5 | 148.5 | 144.5 | 140.5 |
Table 1: Composition of different batches of orodispersible tablets of meloxicam.
Twenty tablets were selected at random and weighed individually. The individual weights were compared with the average weight for determination of weight variation [8]. Hardness and friability of the tablets were determined by using Monsanto Hardness Tester and Roche friabilator respectively. For content uniformity test, ten tablets were weighed and powdered. The powder equivalent to 7.5 mg of meloxicam was extracted into methanol and liquid was filtered. The meloxicam content was determined by measuring the absorbance at 363.2 nm after appropriate dilution with methanol. The drug content was calculated using the standard calibration curve. The mean percent drug content was calculated as an average of three determinations [9]. For determination of wetting time and water absorption ratio [10], a piece of tissue paper folded twice was placed in a small Petri dish (internal diameter of 5 cm) containing 6 ml of water. A tablet was placed on the paper and the time required for complete wetting was measured. The wetted tablet was then weighed. Water absorption ratio ‘R’ was determined using the equation, R=100(Wb- Wa)/Wa, where, Wa is the weight of the tablet before water absorption and Wb is the weight of the tablet after water absorption. For determination of in vitro dispersion time, one tablet was placed in a beaker containing 10 ml of pH 6.8 phosphate buffer at 37±0.5º and the time required for complete dispersion was determined [11]. IR spectra of meloxicam and its formulations were obtained by KBr pellet method using Perkin-Elmer FTIR series (model-1615) spectrophotometer in order to rule out drug-carrier interactions.
In vitro dissolution of meloxicam orodispersible tablets was studied in USP XXIII type-II dissolution apparatus (Electrolab, Model-TDT 06N) employing a paddle stirrer at 50 rpm using 900 ml of pH 6.8 phosphate buffer at 37±0.5° as dissolution medium [12]. One tablet was used in each test. Aliquots of dissolution medium were withdrawn at specified intervals of time and analyzed for drug content by measuring the absorbance at 363 nm. The volume withdrawn at each time interval was replaced with fresh quantity of dissolution medium. Cumulative percent of meloxicam released was calculated and plotted against time. Short-term stability studies on the promising formulations (DCC2 and DCP2) were carried out by storing the tablets at 45±1° over a 3 w period. At intervals of one week, the tablets were visually examined for any physical changes, changes in drug content and in vitro dispersion time.
Orodispersible tablets of meloxicam were prepared by direct compression method employing combination of two super-disintegrants at a time (Table 1). Sodium starch glycolate (SSG), croscarmellose sodium (CCS) and crospovidone (CP) were used as super-disintegrants while microcrystalline cellulose (MCC) and directly compressible mannitol (Pearlitol SD200) were used as diluent and sweetening agent respectively. A total of ten formulations and a control formulation DC0 (without super-disintegrants) were designed. Preliminary studies with tablets containing only one super-disintegrant, viz., SSG (5% w/w) or CCS (3% w/w) or CP (4% w/w) displayed in vitro dispersion time of 67, 60 and 71 s, respectively. Hence it was decided to use a combination of two super-disintegrants so that orodispersible tablets with in vitro dispersion time of less than 15 s may be developed.
As the material was free flowing (angle of repose values <30° and Carr’s index <15), tablets obtained were of uniform weight (due to uniform die fill), with acceptable variation as per IP specifications i.e., below 7.5%. Drug content was found to be in the range of 97-101%, which is within acceptable limits. Hardness of the tablets was found to be 3.3 to 4 kg/ cm2. Friability below 1% was an indication of good mechanical resistance of the tablets. Water absorption ratio and wetting time, which are important criteria for understanding the capacity of disintegrants to swell in presence of little amount of water, were found to be in the range of 71 to 78% and 5 to 7 s respectively. Formulations DCC2 and DCP2 were found to be promising and displayed an in vitro dispersion time of approximately 10 s, which facilitates their faster dispersion in the mouth.
Among the tablet formulations employing various combinations of SSG (1-8% w/w) and CCS (1-3% w/w) as super-disintegrants, the formulation DCC2 containing 2% w/w SSG and 1.5% w/w CCS was found to be promising, and has shown an in vitro dispersion time of 10 s, wetting time of 5s and water absorption ratio of 76% when compared to the control formulation (DCo) which shows 125 s, 24 s and 69.4% values, respectively for the above parameters (Table 2). Further increase in the amount of super-disintegrants increases the in vitro dispersion time (up to 44 s for formulation DCC5), which can be attributed to the gelling effect of SSG at higher concentration [13,14].
| Test | Average weight* (mg) ± SD | Hardness* (kg/cm2) ± SD | Friability (%) | Percent drug content* ± SD | Wetting time* (s) ± SD | Water absorption ratio*(%) ± SD | In vitro Dispersion time* (s) ± SD |
|---|---|---|---|---|---|---|---|
| DC0 | 197 ± 0.002 | 4.0 ± 0.246 | 0.48 | 101.33 ± 0.577 | 24 ± 0.486 | 89.4 ± 0.214 | 125 ± 0.432 |
| DCC1 | 196 ± 0.001 | 3.5 ± 0.313 | 0.83 | 99.03 ± 0.776 | 5 ± 0.416 | 77.3 ± 0.654 | 14 ± 0.645 |
| DCC2 | 197 ± 0.002 | 3.5 ± 0.224 | 0.69 | 98.66 ± 0.231 | 5 ± 0.315 | 76.4 ± 0.586 | 10 ± 0.326 |
| DCC3 | 198 ± 0.002 | 3.4 ± 0.456 | 0.75 | 97.66 ± 0.471 | 7 ± 0.409 | 76.4 ± 0.209 | 25 ± 0.212 |
| DCC4 | 199 ± 0.002 | 3.5 ± 0.283 | 0.73 | 97.33 ± 0.618 | 6 ± 0.416 | 74.3 ± 0.224 | 38 ± 0.224 |
| DCC5 | 201 ± 0.002 | 3.3 ± 0.336 | 0.84 | 99.36 ± 0.980 | 5 ± 0.454 | 71.6 ± 0.287 | 44 ± 0.326 |
| DCP1 | 200 ± 0.001 | 3.5 ± 0.244 | 0.61 | 102.13 ± 0.659 | 7 ± 0.456 | 75.6 ± 0.324 | 26 ± 0.414 |
| DCP2 | 199 ± 0.002 | 3.3 ± 0.215 | 0.63 | 99.00 ± 0.374 | 7 ± 0.533 | 74.6 ± 0.313 | 11 ± 0.218 |
| DCP3 | 200 ± 0.002 | 3.4 ± 0.218 | 0.56 | 98.36 ± 0.679 | 6 ± 0.493 | 76.1 ± 0.354 | 18 ± 0.216 |
| DCP4 | 201 ± 0.001 | 3.5 ± 0.248 | 0.59 | 97.96 ± 0.124 | 5 ± 0.416 | 77.0 ± 0.246 | 26 ± 0.242 |
| DCP5 | 201 ± 0.002 | 3.5 ± 0.212 | 0.59 | 98.32 ± 0.840 | 5 ± 0.224 | 78.2 ± 0.315 | 29 ± 0.284 |
Table 2: Evaluation of orodispersible tablets
Among the tablet formulations employing various combinations of SSG (1-8% w/w) and CP (3-4% w/w) as super-disintegrants, the formulation DCP2 containing 2% w/w SSG and 3% w/w CP was found to be promising, and has displayed an in vitro dispersion time of 11 s, wetting time of 7 s and water absorption ratio of 75% when compared to the control formulation (DCo), which shows 125 s, 24 s and 69.4% values, respectively, for the above parameters (Table 2). Further increase in the amount of super-disintegrants increases the in vitro dispersion time (up to 29 s for formulation DCP5) due to the same reasoning as stated above.
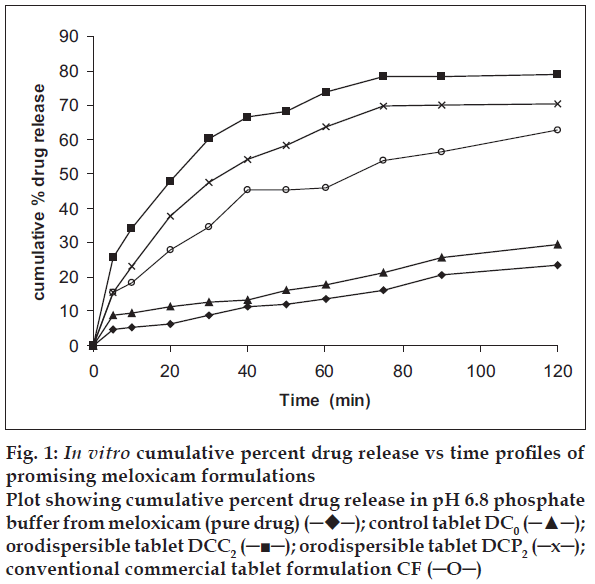
In vitro dissolution studies on the promising formulations (DCC2 and DCP2), the control (DCo) and commercial formulation (CF) along with the pure drug (meloxicam) were carried out in pH 6.8 phosphate buffer, and the various dissolution parameter values viz., percent drug dissolved in 10 min (D10), dissolution efficiency at 30 min (DE30 min)15, t50% and t70% are shown in Table 3, and the dissolution profiles depicted in fig. 1. This data reveals that overall, the formulation DCC2 has shown three-fold faster drug release (t50%=22 min) when compared to the marketed conventional tablet formulation of meloxicam (t50%=68 min) and released 12 times more drug than the control formulation in 10 min.
| Formulation code | D10 (%) | DE30 min (%) | t50% (min) | t70% (min) |
|---|---|---|---|---|
| MX | 5.46 | 5.23 | >120 | >120 |
| DC0 | 2.9 | 2.63 | >120 | >120 |
| DCC2 | 34.17 | 36.9 | 22 | 53 |
| DCP2 | 23.06 | 21.1 | 69 | > 120 |
| CF | 18.53 | 20.9 | 68 | > 120 |
Table 3: in vitro dissolution parameters in ph 6.8 phosphate buffer.
Figure 1: In vitro cumulative percent drug release vs time profiles of promising meloxicam formulations
Plot showing cumulative percent drug release in pH 6.8 phosphate buffer from meloxicam (pure drug) (─♦─); control tablet DC0 (─▲─); orodispersible tablet DCC2 (─■─); orodispersible tablet DCP2 (─x─); conventional commercial tablet formulation CF (─O─)
IR spectroscopy indicated that the drug is compatible with all the excipients. The IR spectrum of DCC2 showed all the characteristic peaks of meloxicam pure drug, thus confirming that no interaction of drug occurred with the components of the formulation. Short-term stability studies of the above formulation indicated that there were no significant changes in drug content and in vitro dispersion time at the end of a 3 w period (P<0.05).
References
- Seager H.Drug delivery productsand theZydis fast dissolving dosage forms. J Pharm Pharmacol1998;50:375-82.
- Chang RK, Guo X, Burnside BA, Couch RA. Fast dissolving tablets. Pharm Tech 2000;24:52-8.
- Dobetti L. Fast melting tablets: Developments and technologies. Pharm Tech 2001;(Suppl):44-50.
- Kuchekar BS, Arumugam V. Fast dissolving tablets. Indian J Pharm Edu 2001;35:150-2.
- Sweetman SC, editor. Martindale: The complete drug reference. 33rd ed., London: Pharmaceutical Press; 2002. p. 52-3.
- British Pharmacopoeia: The Department of Health, London: Social Services and Public Safety; 2001. p. 1064-5.
- Kucherkar BS, Badhan AC, Mahajan HS. Mouth dissolving tablets of salbutamol sulphate: A Novel drug delivery system. Indian Drugs 2004;41:592-8.
- Banker GS, Anderson NR. Tablets.In:Lachman L, Lieberman HA, Kanig JL, editors. The theory and practice of industrial pharmacy. 3rd ed. Mumbai: Varghese Publishing House; 1987. p. 293-9.
- Indian Pharmacopoiea: Controller of Publications, Government of India, New Delhi: Ministry of Health and Family Welfare; 1996. p. 735-6.
- Chaudhari PD, Chaudhari SP, Kolhe SR, Dave KV, More DM. Formulation and evaluation of fast dissolving tablets of famotidine. Indian Drugs 2005:42:641-9.
- Bi YX, Sunada H, Yonezawa Y, Danjo K. Evaluation of rapidly disintergranting tablets by direct compression method. Drug Develop Ind Pharm 1999;25:571-81.
- Bhagwati ST, Hiremath SN, Sreenivas SA. Comparative evaluation of disintegrants by formulating cefixime dispersible tablets. Indian J Pharm Edu 2005;39:194-7.
- Wade A, Weller PJ, editors. Handbook of pharmaceutical excipients. 2nded. London: The Pharmaceutical Press; 1994. p. 462-3.
- Bolhuis GK, Zuuman K, TeWienk GH. Improvement of dissolution of poorly soluble drugs by solid dispersion on superdisintegrant part 2: Choice of superdisintegrants and effect of granulation. Eur J Pharm Sci 1997;5:63-9.
- Khan KA. The concept of dissolution efficiency. J Pharm Pharmacol 1975;27:48-9.