- *Corresponding Author:
- Linshu Cheng
Department of Anesthesia, Shijiazhuang Matemity and Child Healthcare Hospital, Shijiazhuang, Hebei Province 050000, China
E-mail: Chenglinshu2699123@163.com
| This article was originally published in a special issue, “Drug Discovery and Repositioning Studies in Biopharmaceutical Sciences” |
| Indian J Pharm Sci 2024:86(4) Spl Issue “380-391” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
The limitation of traditional general anesthesia postoperative pain relief methods is that the efficacy is relatively single, lacks individualization, and is prone to overuse and adverse reactions. This article explored the efficacy and safety of butorphanol combined with multimodal image fusion technology in the treatment of postoperative agitation in children under general anesthesia, providing an effective method for clinical treatment of postoperative agitation in children under general anesthesia. This article collected general data and clinical manifestations of restless children after general anesthesia surgery, and observed and evaluates 40 children. These children, aged between 1 y and 6 y old, received general anesthesia and developed varying degrees of restlessness symptoms after surgery. Among them, 20 children (control group) received traditional single treatment methods, while the other 20 children (experimental group) used multimodal image fusion technology for imaging diagnosis of patients. This article summarized the application value of combined treatment with butorphanol based on diagnostic results, while observing the treatment effect and adverse reactions. The results showed that the average restlessness rate in the experimental group was 54.45 % lower than that in the control group. Compared with traditional single treatment methods, the combined use of multimodal image fusion technology and butorphanol can significantly improve the incidence of postoperative agitation in children with general anesthesia. The research results can provide clinical doctors with more intuitive and accurate diagnostic information, thereby more accurately formulating treatment plans and achieving personalized treatment.
Keywords
Multimodal image fusion, general anesthesia, postoperative agitation, butorphanol, adverse reactions
Postoperative agitation is a common complication of pediatric anesthesia, which often leads to a longer recovery period and causes great distress to medical staff. There are many treatment methods for restlessness after General Anaesthesia (GA) surgery, but due to the complex causes of restlessness in children, a single treatment method is difficult to achieve ideal therapeutic effects. Therefore, the comprehensive use of multiple treatment methods to treat different symptoms of restlessness after pediatric GA surgery is currently the main clinical treatment method. Multimodal image fusion is a kind of image information fusion with different sensors and different modes, which has broad application prospects. After GA surgery, appearing delirium is an early behavioral alteration. It is not yet known, though, if children who have appearing delirium can experience any negative behavioral effects after being released from the hospital. Kim et al.[1] looked at the connection between post-hospital behavioral changes and appearing delirium. 100 preschool children aged 2-7 underwent elective surgery at two tertiary university hospitals. He divided delirium scores into delirium specific scores, with high delirium scores representing severe appearing delirium. The main outcome measure is the total score of the behavioral examination form 1 w after surgery. Children with symptomatic delirium (n=58) had higher postoperative behavioral examination scores than those without symptomatic delirium (n=42), and an increase in delirium peak specificity score was associated with an increase in behavioral examination scores 1 w after surgery, while pain related scores, surgical type, pre medication, and age were not related. Children’s appearing delirium is a psychomotor illness that manifests in the early stages following anesthesia. While a current study does not clearly agree on how to treat it, dexmedetomidine and propofol have both been shown to be useful. Han et al.[2] evaluated the effectiveness of propofol and dexmedetomidine in treating delirium in children with GA in a prospective research. The patients ranged in age from 1 y to 14 y. Out of the 53 patients that took part in the research, 26 (49 %) were treated with dexmedetomidine, and 27 (51 %) were treated with propofol. The findings demonstrated that a single dosage intervention was 100 % successful for all patients in the dexmedetomidine group. Nineteen patients in the propofol group experienced dangerous delirium scores following their initial dosage, and there was no statistically significant difference in the recovery duration between the propofol and dexmedetomidine groups. Patients, their families, and clinical physicians experience severe distress when delirium occurs in children following GA. Nevertheless, not all of the Electroencephalogram (EEG) indicators for delirium prediction have been investigated. In a prospective, single-center observational study, Kim et al.[3] compared the relative power of low-frequency and high-frequency EEG during the development of delirium in children with and without delirium. The children in the study ranged in age from 2 y to 10 y old. He explored the linear relationship between relative power and the peak of delirium assessment score in children. The results showed that among 60 patients, 22 experienced delirium (delirium group) and 38 did not experience delirium (non-delirium group). The relative power of EEG in the delirium group was higher than that in the non-delirium group. Episodic delirium is a common complication in pediatric anesthesia, often occurring after short-term surgical procedures using volatile anesthetics and recovering rapidly. The goal of Jooma et al.[4] research is to characterize the prevalence of delirium and the risk variables that go along with it in kids who are getting selective dental surgery at a South African regional academic hospital while under general anesthesia. Using a consistent methodology to anesthetize patients, he performed a prospective descriptive research on healthy children between the ages of 2 y and 6 y. Evaluation includes delirium scores during intraoperative events and pediatric anesthesia in the recovery room. The results showed that 69.2 % of patients experienced anxiety during induction, and appearing delirium was common after dental surgery. Most children who came for dental surgery experienced anxiety during induction. Children with appearing delirium require more rehabilitation room interventions, but rarely require medication treatment[4]. Next, the paper analyzed the comprehensive therapeutic effect of multimodal image fusion technology combined with drug therapy on postoperative agitation in children with GA, in order to provide reference for the treatment of similar patients in the future.
Multimodal medical image fusion’s primary goal is to extract useful data by combining several images from various sources into a single image that can be used for more accurate diagnosis. Tirupal et al.[5] provided a detailed overview and comparative discussion of various existing medical image fusion algorithms. According to this study, several collaborative medical picture fusion strategies are beneficial for medical diagnosis and evaluation, even in the face of some open creativity and logical challenges. Additionally, efficient use of these techniques can enhance the effectiveness of image fusion algorithms. In the past decade, significant progress has been made in the field of multimodal medical image fusion. However, previous methods always had issues with color distortion, blurring, and noise. In order to resolve these problems, Li et al.[6] proposed a Laplace re decomposition framework suitable for multimodal medical picture fusion. Considering the diversity of redundant and complementary information, the concepts of overlapping and non-overlapping domains are presented. The experimental results show that this method performs better in both qualitative and quantitative aspects compared to other well-known fusion techniques. The act of combining visual data from any number of medical image inputs into a single fused image without distortion or detail loss is known as medical image fusion. However, there are problems with the fused image, like processing costs and fusion artifacts. The method for hybrid multimodal medical picture fusion was created with pathological research in mind. For a variety of medical image fusion applications, Rajalingam et al.[7] has created two algorithms based on hybrid multimodal medical image fusion technology. The suggested approach is superior in both qualitative and quantitative evaluation, according to experimental data. Multimodal medical image fusion has been widely applied in various clinical applications. Multimodal medical image fusion can provide experts with images of anatomical and physiological data, advancing diagnostic procedures. Previous researchers have proposed various models related to multimodal medical image fusion, but there is still a need to improve the efficiency of previous technologies. Using an improved monarch butterfly optimization technique, Subbiah et al.[8] presented an ideal threshold fusion model based on deep learning principles. This model determines the ideal threshold for fusion rules. According to the simulation findings, the suggested model performs well in terms of mutual information, spatial frequency, and edge quality. With the continuous development of technology, multimodal image fusion technology has become a widely used technology in the medical field, especially in image diagnosis, treatment, surgical operations, and other aspects.
Multimodal image fusion technology can integrate multiple image information, improve the diagnostic accuracy of postoperative agitation in children under general anesthesia, and assist doctors in formulating reasonable treatment plans. Butorphanol plays an important role in pain relief, but it also has certain adverse reactions, so there is an urgent need to find effective treatment methods.
Materials and Methods
Multimodal image fusion technology:
The integration and processing of multimodal data to accomplish more thorough and precise diagnosis, and treatment objectives is known as multimodal image fusion. X-rays, Computed Tomography (CT), Magnetic Resonance Imaging (MRI), and Positron Emission Tomography (PET) are just a few examples of the many imaging modalities available in modern medical imaging technologies. With unique benefits and drawbacks, every imaging method can offer a variety of imaging data. The fusion of multimodal pictures can produce complementary benefits, complementarity, and augmentation, improving the accuracy and reliability of diagnosis and therapy. However, single modality images do not always provide a complete picture of biological information[9,10]. The use of multimodal picture fusion technology has expanded in recent years, and people are progressively coming to understand its significance and worth.
Classification of multimodal image fusion technology:
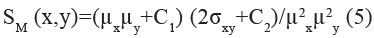
Image fusion: Image fusion is an important aspect of multimodal fusion technology. By merging image information from multiple sources, image fusion improves the overall quality, information content, and usability of the image. By overlaying or synthesizing multiple modal images, more comprehensive and accurate images can be obtained. This type of fusion technology mainly includes image fusion techniques based on weighted average and transformation. The principle of multimodal image fusion technology is shown in fig. 1.
As shown in fig. 1, the principle of multimodal image fusion technology is to decompose the source image into high-frequency and low-frequency coefficients, which are then fused into fusion coefficients through fusion rules, and then reconstructed into a fused image.
Image fusion is a technique for fusing multi-source image features. This system integrates multiple sources of information such as visible light, infrared and radar, which can obtain more comprehensive and multi-dimensional image information, and improve the recognition and analysis capabilities of targets[11,12]. In military applications, visible light images can obtain target morphology details, while infrared images can obtain target thermal image information at night or under adverse weather conditions. The fusion of the two can improve the accuracy and robustness of target recognition.
By setting the weight coefficient reasonably, the accuracy of target recognition can be improved by fully utilizing the thermal feature information of infrared images while preserving the details of visible light images:
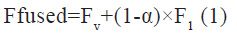
The fused features are represented by Ffused, with Fv and F1 representing the features of visible light and infrared images, respectively. The weight coefficients are represented by α, indicating the contribution of visible light images in the fusion. By adjusting the value of α, the relative importance of two source images in fusion can be flexibly controlled.
In practical applications, optimizing weights for different scenarios and sensor characteristics can effectively improve the quality and accuracy of fused images. After feature fusion, weight adjustment can be introduced to optimize the fusion results:
The final fusion result is represented by Ffinal, the noise term is represented by N, and the optimization weight coefficient is represented by β. By balancing the fusion results and noise terms, optimization of the final image can be achieved.
Image fusion technology also involves the optimization and display of image fusion results. When fusing, it is necessary to comprehensively consider factors such as the weight, sensitivity, and noise of each sensor, so as to remove redundant information as much as possible from the obtained image while maintaining important information. The optimized image not only improves the visual perception of the human eye, but also facilitates further processing and analysis of images by computer vision systems. Meanwhile, fusion technology can visually present multimodal information to users, enhancing their understanding and decision-making abilities.
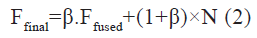
Feature fusion: In multimodal image fusion technology, feature fusion is a key link. Its purpose is to obtain more comprehensive, accurate and informative image fusion results by fusing image features of different sensors or modes. Feature fusion can be achieved by balancing feature contributions from different sensors. This can be represented by formula:
By adjusting the weight coefficients, feature fusion can focus more on specific original image information, making the final fused features more targeted and effective.
Decision fusion: By combining decision data from many sources, decision fusion is an essential stage in multimodal image fusion technology that aims to increase the precision and resilience of the system’s target or scene detection. The goal of decision fusion is to combine the outcomes of several modalities to create more thorough and dependable decisions, as well as to maximize the performance of multimodal fusion systems. Rule fusion and weighting can be used to achieve decision fusion. Rule fusion combines different modal judgments using logical processes and is based on established decision rules. This approach can increase the overall consistency and accuracy of decision-making by properly accounting for the link between various decisions.
Multimodal image fusion technology in the field of medical imaging:
Multimodal image fusion technology has been widely applied in the field of medical imaging, providing doctors with more comprehensive and accurate diagnostic information, effectively improving the quality and efficiency of medical services[13,14]. The application content of multimodal image fusion technology in the field of medical imaging is shown in fig. 2.
As shown in fig. 2, the application of multimodal image fusion technology in the field of medical imaging includes cancer diagnosis, brain disease diagnosis, cardiovascular disease diagnosis, and disease treatment.
Cancer diagnosis: By comprehensively integrating multimodal medical imaging data, more comprehensive and rich imaging information can be obtained. This comprehensive information can effectively improve the detection and recognition ability of tumor edges and internal tumor tissues, and improve the accuracy of cancer diagnosis.
Diagnosis of brain diseases: Doctors can identify the kind and severity of brain disorders by using the combination of multimodal medical imaging data to more accurately assess and detect aberrant changes in the structure of brain tissue.
Physicians can acquire more extensive brain imaging data by combining information from other imaging modalities, such as functional PET and structural MRI. With the aid of multimodal fusion technology, physicians may accurately diagnose a variety of brain disorders by gaining a better understanding of the patient’s condition and brain state (such as tumors, vascular diseases, and neurological diseases).
Cardiovascular disease diagnosis: More thorough information on the circulatory system can be obtained by integrating multimodal images, such as cardiac CT and MRI. While functional imaging shows the heart’s blood flow and metabolism, structural imaging can show the heart’s anatomical structure. When used in tandem, they can offer a thorough picture of the patient’s cardiovascular system status and facilitate an accurate evaluation of the anatomy and function of the heart.
Disease treatment: Fusing multimodal medical imaging data can improve the precision and effectiveness of medical services by giving patients access to more thorough and precise illness diagnosis information. Multimodal image fusion technology can also offer real-time treatment process monitoring and guidance in the interim. By combining photos taken at various intervals, medical professionals can monitor the disease’s course and effectiveness. Multimodal fusion technology can give high- resolution navigation images during surgery, assisting physicians in performing procedures more effectively and reducing collateral harm.
Results and Discussion
Butorphinol is a commonly used medicine for the treatment of moderate to severe chronic pain. Its pharmacological feature is that it has an analgesic effect by binding to opiate receptors. The opiate receptor agonist butorphinol can bind to the µ opiate receptor to produce a powerful analgesic effect. This receptor can inhibit neuronal excitability, reduce pain transmission, and relieve pain[15,16]. Butorphinol can exert sedative and anti-cough effects by activating the brainstem Kappa (κ)-opioid receptor, thereby achieving overall regulation of pain.
Pharmacodynamic studies have shown that butorphinol is specific to the µ-opiate receptor and can bind to the κ-opioid receptor to produce a powerful analgesic effect. This effect can block the pain conduction pathway, reduce neuronal excitability, and exert analgesic effects. In addition, butorphanol can also activate the κ-opioid receptor to produce sedative, anti-cough and other effects. Therefore, it is a chronic pain treatment method with comprehensive pharmacological effects[17,18].
In terms of pharmacokinetics, butorphanol’s drug metabolism mostly takes place in the liver, where it produces a variety of metabolites that have analgesic properties, however it is yet unknown how exactly this occurs. These metabolites are further converted into water-soluble metabolites in the body, which are then excreted from the body by the kidneys. Butorphanol has a longer half-life in the human body and can produce long-lasting analgesic effects, helping to reduce the frequency of medication. During the medication process, personalized adjustments to the dosage should be made based on the patient’s liver function to ensure safe and effective medication.
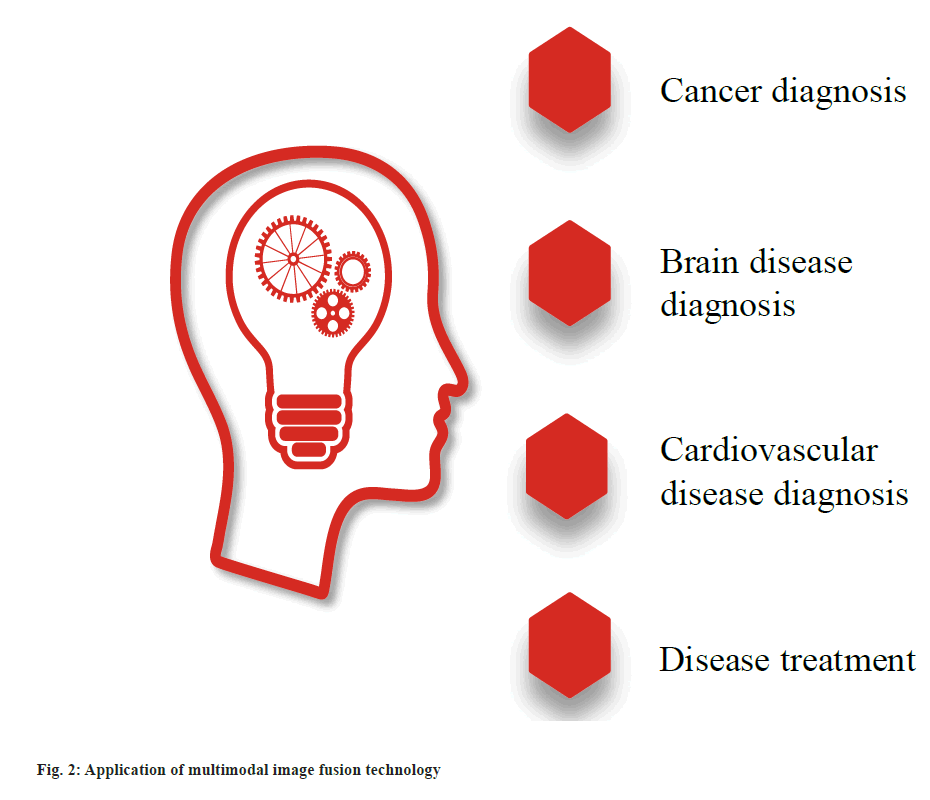
Butorphanol has become a commonly used method for postoperative pain relief under general anesthesia, especially playing an important role in postoperative pain control. Both showed similar performance in relieving postoperative pain, but patients with butorphanol had a higher respiratory rate than those with morphine. Compared to morphine, butorphanol has a lower risk of respiratory depression, making it a relatively safe method of general anesthesia. The molecular structure of butorphanol was shown in fig. 3.
As shown in fig. 3, O represents oxygen, H represents hydrogen, and N represents nitrogen. The analgesic effect of butorphanol may be influenced by dosage and route of administration. A study has found that intravenous injection of butorphanol exhibits better analgesic effects within 24 h after GA compared to oral administration of butorphanol. Therefore, when formulating a postoperative analgesia plan for GA, doctors should choose the appropriate dosage and administration method of butorphanol based on the patient’s condition and surgical type. This can maximize the analgesic effect, reduce adverse reactions, and provide experimental basis for the rational use of butorphanol in clinical treatment of postoperative pain.
Numerous researches have tried combining butorphanol with other medications to increase its analgesic efficacy. Studies have indicated that the synergy between butorphanol and dopamine can enhance the overall analgesic impact while lowering the dosage of other medications. It’s possible that butorphanol and dopamine work in concert. This may lessen adverse effects while enhancing the analgesic effect. This offers a fresh method for using multiple medication combinations to treat pain following GA and improve pain control’s balance.
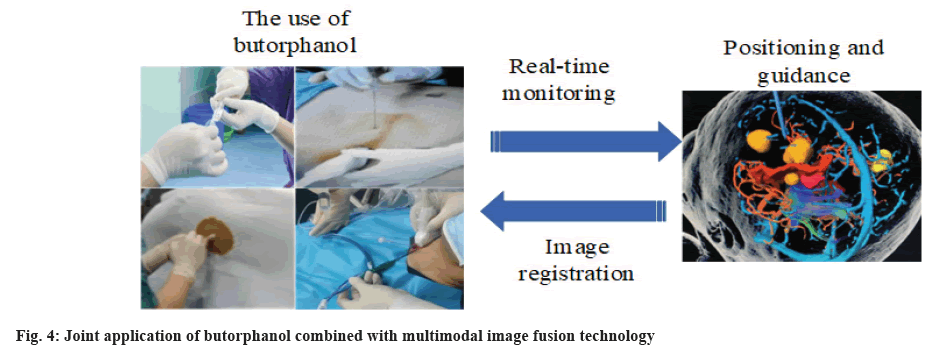
In pediatric GA, postoperative agitation is a frequent adverse event, particularly when tracheal intubation and propofol anesthesia are used during the surgical procedure[19,20]. Treatment with a combination of butorphanol and multimodal image fusion technologies was tried to lower the prevalence of postoperative agitation in children. The joint application was shown in fig. 4.
As shown in fig. 4, the most common application of butorphanol combined with multimodal image fusion technology is for localization and guidance.
Before the start of treatment, multimodal imaging data is collected by using different medical imaging devices such as structural MRI, functional MRI, and PET. These data can provide information on the structure and function of pain related brain regions. Multimodal image fusion technology can be used, utilizing computer vision and image processing techniques to fuse multimodal images. For this purpose, methods such as image registration and feature fusion can be used to achieve comprehensive and three-dimensional description of patient status[21,22].
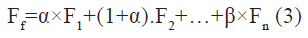
Mutual information is used to measure the degree of interdependence between two random variables and is widely used in image registration:
I (X;Y) is mutual information; p (x,y) is a joint probability distribution; p (x) and p (y) are marginal probability distributions, respectively.
The structural similarity index is an indicator used to measure the similarity between two images, which includes brightness, contrast, and structure:
Where, σxy is the standard deviation of x and y; C1 and C2 are constants used to stabilize the denominator.
By integrating multimodal imaging data, it can deeply analyze the mechanism of patient pain occurrence. By understanding abnormalities in neural activity, structure, and function, doctors can more accurately identify the sources and mechanisms of pain[23,24]. On this basis, scientific basis can be provided for the individualized treatment of butorphanol. This personalized treatment plan is expected to improve the effectiveness of treatment, reduce side effects and adverse reactions.
During the treatment process, multimodal image fusion technology is used to monitor the patient’s neurological status and pain areas in real-time. Doctors can dynamically adjust the treatment regimen of butorphanol based on patient subjective feedback and physiological indicators to achieve sustained pain relief[25,26]. Medical image processing software, device networking, and other technical techniques allow for real-time monitoring and feedback correction, allowing patients to obtain precise and personalized pain relief treatment. In light of these considerations, butorphanol in combination with multimodal image fusion technology integrates several data sources, generates personalized treatment plans, and continuously monitors patient reactions. This provides more complete and accurate support for clinical pain treatment, which improves patient outcomes and quality of life.
This exact method entails creating a spatial anatomical model of the child using multimodal imaging before surgery, placing an electrode on the child’s head, and initiating EEG monitoring. Depending on the findings of the EEG monitoring, the patient may get personalized analgesia (including a combination of butorphanol and other drugs) after surgery in addition to sedation, muscular relaxation, and other analgesic treatments.
The experimental subjects were children who developed restlessness after anesthesia surgery, and a total of 40 children who met the inclusion criteria were recruited. The basic information was shown in Table 1.
| Classification | Number of people | Percentage | |
|---|---|---|---|
| Age | 1-3 | 15 | 0.38 % |
| 4-6 | 25 | 0.63 % | |
| Liver and kidney function | Normal | 40 | 1 % |
| Abnormal | 0 | 0 % | |
| Whether other medications were used during surgery | Yes | 0 | 0 % |
| No | 40 | 100 % | |
| Drug allergy history | Yes | 0 | 0 % |
| No | 40 | 100 % | |
| Voluntary participation | Yes | 40 | 100 % |
| No | 0 | 0 % | |
Table 1: Basic Information of Children
As shown in Table 1, it can be observed that children are aged between (1-6) y old, with a higher proportion (62.5 %) aged (4-6) y old. The liver and kidney functions of children are all normal. No sedatives or other medications were used during the surgery, and there was no history of drug aller gies.
This article randomly divided the experimental subjects into two groups. The experimental group (20 cases) underwent butorphanol combined with multimodal image fusion technology. The control group (20 cases) received monotherapy without the use of butorphanol. Both groups were observed for 24 h after surgery, and their restlessness, analgesic effects, and side effects were monitored and evaluated in the operating room.
Butorphanol is currently a relatively safe and effective postoperative analgesic drug in clinical practice, but it has drawbacks such as short duration and limited efficacy of a single drug. Therefore, combining with other drugs or adopting personalized analgesic regimens may enhance the analgesic effect of butorphanol. At the same time, the use of multimodal imaging technology combined with butorphanol to achieve personalized analgesia reduces the incidence of postoperative agitation in children, improves patient satisfaction with analgesia, and has high clinical application value[27,28]. The incidence of restlessness in both groups within 5 d after surgery was shown in Table 2.
| Day and average | Control group | Experimental group |
|---|---|---|
| 1 | 74.48 % | 20.58 % |
| 2 | 68.85 % | 17.33 % |
| 3 | 71.21 % | 12.85 % |
| 4 | 73.56 % | 14.96 % |
| 5 | 62.91 % | 13.05 % |
| Average | 70.20 % | 15.75 % |
Table 2: Incidence of Restlessness (Multiple Choices)
As shown in Table 2, the average restlessness incidence rates of the control group and the experimental group at 5 d after surgery were 70.20 % and 15.75 %, respectively. It can be seen that the average restlessness rate in the experimental group is much lower than that in the control group, by 54.45 %.
By integrating multimodal imaging information and combining it with EEG monitoring results, it is possible to comprehensively understand the patient’s neurological status and the mechanism of pain occurrence. This offers a more accurate, individualized analgesic regimen for postoperative combination therapy involving multiple drugs and butorphanol. It is anticipated that this integrated treatment approach can be more successful in lowering the frequency of postoperative agitation in kids receiving general anesthesia and in giving kids safer, more comfortable postoperative care[29,30]. This novel approach to treatment offers fresh perspectives for postoperative pain management research.
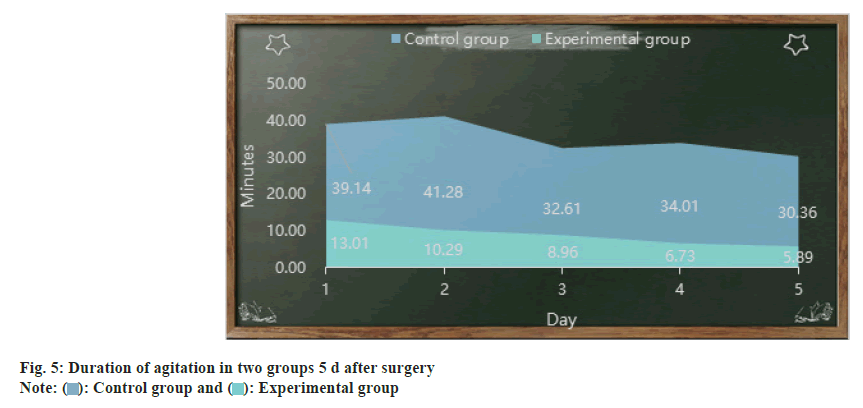
This article compares the duration of agitation between two groups 5 d after surgery, as shown in fig. 5 (the horizontal axis represents days, and the vertical axis represents minutes). As shown in fig. 5, the duration of agitation in the control group and experimental group on the 1st d after surgery was 39.14 min and 13.01 min, respectively. On the 5th d after surgery, the duration of agitation in the control group and experimental group was 30.36 min and 5.89 min, respectively. Overall, the duration of agitation in the experimental group was lower than that in the control group.
This article integrates multimodal images such as CT and MRI, combined with EEG monitoring, to comprehensively evaluate the patient’s neurological status and pain mechanisms. This makes it possible for butorphanol combined with other drugs to finely regulate pain, providing the possibility for individualized postoperative analgesic treatment.
This comprehensive treatment strategy cannot only achieve analgesic effects, but also significantly shorten the restlessness period after pediatric GA surgery. Multimodal imaging technology achieves precise personalized treatment, better suppresses neural excitability, reduces pain transmission, and reduces the incidence and duration of agitation. It has a positive significance in improving postoperative comfort, reducing postoperative discomfort, and promoting early recovery of patients, providing new ideas for improving the level of postoperative agitation management in pediatric general anesthesia.
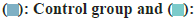
This article uses a 1-10 scale to assess agitation levels. An increased score corresponds to an increased level of agitation. Mild agitation is indicated by a score of 1-3, moderate agitation is indicated by a score of 4-6, and severe agitation is indicated by a score >6. In this article, two groups’ levels of restlessness 5 d following surgery are compared, as seen in fig. 6 (scores are represented on the vertical axis and distinct groups are represented on the horizontal axis).
As shown in fig. 6, the restlessness scores of the control group were all above 5 points, except for moderate restlessness on the 1st d, and severe restlessness on the remaining 4 d. The restlessness scores of the experimental group were all within 3 points, indicating that the experimental group was slightly restless.
Butorphanolone is a commonly used analgesic in clinical practice, and its efficacy is accurate. It binds to the μ and κ receptors in the central nervous system to control pain and sedate. Therefore, butorphanol is used as the main medication to treat postoperative agitation in children with GA. On this basis, multimodal image fusion technology can be used to comprehensively monitor physiological parameters such as EEG, cerebral blood flow, respiration, heart rate, etc., to further evaluate the degree of agitation and therapeutic effect of patients.
Similarly, a score of 1-10 is used to evaluate the analgesic effect, and the higher the score, the better the effect. A score of <6 indicates that the effect is not very good. The analgesic effects of the two groups 5 d after surgery are shown in Table 3. As shown in Table 3, the analgesic effect scores of both the control group and the experimental group decreased with the increase of postoperative days, and the analgesic effect continued to weaken. However, it can be found that the average analgesic effect score of the experimental group was 8.24 points, while the average analgesic effect score of the control group was only 5.41 points.
| Day and average | Control group | Experimental group |
|---|---|---|
| 1 | 7.11 | 8.9 |
| 2 | 6.65 | 8.57 |
| 3 | 4.89 | 8.08 |
| 4 | 4.33 | 7.91 |
| 5 | 4.06 | 7.72 |
| Average | 5.41 | 8.24 |
Table 3: Analgesic Effects of Two Groups 5 D after Surgery
Combination therapy not only relies on medication, but also combines advanced imaging techniques. Butorphanol can exert analgesic effects by activating opioid receptors. Multi-mode image fusion technology can obtain real-time neural state information, helping doctors adjust treatment plans more intelligently.
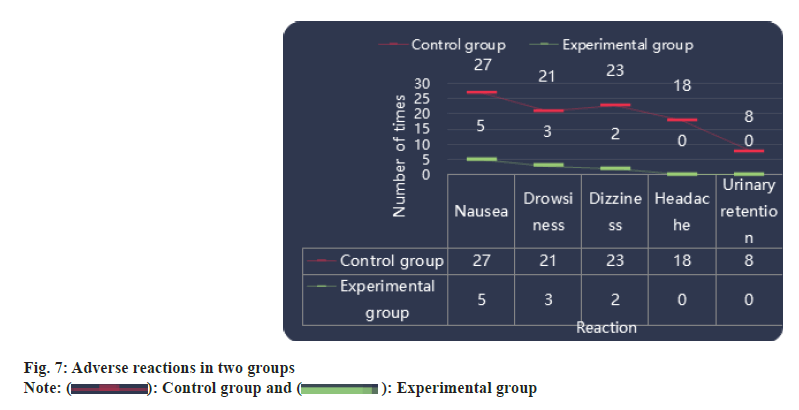
Adverse reactions including nausea, vomiting, drowsiness, dizziness, headache and urinary retention may occur after GA operation. This article counts the total times of these reactions 5 d after operation, as shown in fig. 7 (abscissa represents reactions, ordinate represents times). As shown in fig. 7, the experimental group experienced a total of 5 occurrences of nausea and vomiting within 5 d, which is also the highest number of adverse reactions. The control group had a total of 27 occurrences of nausea and vomiting within 5 d, which far exceeded the total occurrence of nausea and vomiting in the experimental group.
Multimodal image fusion technology cannot only provide patients with more comprehensive information, but also help doctors adjust the dosage and mode of administration more accurately, thereby achieving the best therapeutic effect. By implementing detailed personalized treatment plans, especially in pediatric patients, pain management and the risk of adverse reactions can be better balanced, as well as safer and more effective postoperative pain relief.
This article adopted multimodal imaging technology combined with butorphanol for the treatment of restlessness after pediatric GA surgery, and observed and evaluates its therapeutic effect. Multimodal image fusion technology is currently a hot topic in medical imaging research. By fusing different types of medical images, it can provide patients with more accurate and intuitive diagnostic information. Butorphanol is a sedative and antihypertensive drug widely used in general anesthesia for children. Multi-mode image fusion technology combined with butorphanol for the treatment of postoperative agitation in children under general anesthesia. It cannot only significantly improve postoperative agitation symptoms in children, but also provide more intuitive and accurate diagnostic information for medical personnel, so as to more accurately formulate treatment plans and implement personalized treatment. The promotion and application of this treatment plan is expected to provide new ideas and methods for the treatment of postoperative agitation in children with GA.
Funding:
This work was supported by Application of butorphanol, dezocine combined with ERAS and systematic analgesia management in pediatric anesthesia (Subject No: 20231638).
Author’s contributions:
Xiaonan Zhang and Yanhong Feng have contributed equally to this work.
Conflict of interests:
The authors declared no conflict of interests.
References
- Kim J, Byun SH, Kim JW, Kim JY, Kim YJ, Choi N, et al. Behavioral changes after hospital discharge in preschool children experiencing emergence delirium after general anesthesia: A prospective observational study. Pediatr Anesth 2021;31(10):1056-64.
[Crossref] [Google Scholar] [PubMed]
- Han X, Sun X, Liu X, Wang Q. Single bolus dexmedetomidine vs. propofol for treatment of pediatric emergence delirium following general anesthesia. Pediatr Anesth 2022;32(3):446-51.
[Crossref] [Google Scholar] [PubMed]
- Kim J, Lee HC, Byun SH, Lim H, Lee M, Choung Y, et al. Frontal electroencephalogram activity during emergence from general anaesthesia in children with and without emergence delirium. Br J Anaesth 2021;126(1):293-303.
[Crossref] [Google Scholar] [PubMed]
- Jooma Z, Perrie H, Scribante J, Kleyenstuber T. Emergence delirium in children undergoing dental surgery under general anesthesia. Pediatr Anesth 2020;30(9):1020-6.
[Crossref] [Google Scholar] [PubMed]
- Tirupal T, Mohan BC, Kumar SS. Multimodal medical image fusion techniques-A review. Curr Signal Transduct Ther 2021;16(2):142-63.
- Li X, Guo X, Han P, Wang X, Li H, Luo T. Laplacian redecomposition for multimodal medical image fusion. IEEE Trans Instrum Meas 2020;69(9):6880-90.
- Rajalingam B, Al-Turjman F, Santhoshkumar R, Rajesh M. Intelligent multimodal medical image fusion with deep guided filtering. Multimedia Syst 2022;28(4):1449-63.
- Subbiah Parvathy V, Pothiraj S, Sampson J. A novel approach in multimodality medical image fusion using optimal shearlet and deep learning. Int J Imaging Syst Technol 2020;30(4):847-59.
- Zhao N, Zeng J, Fan L, Zhang C, Wu Y, Wang X, et al. The effect of alfentanil on emergence delirium following general anesthesia in children: A randomized clinical trial. Pediatr Drugs 2022;24(4):413-21.
- Lee-Archer PF, von Ungern-Sternberg BS, Reade MC, Law KC, Long D. An observational study of hypoactive delirium in the post-anesthesia recovery unit of a pediatric hospital. Pediatr Anesth 2021;31(4):429-35.
[Crossref] [Google Scholar] [PubMed]
- Wu X, Liu Y, Li B, Zhou D, Cheng T, Ma T, et al. Safety of deep intravenous propofol sedation in the dental treatment of children in the outpatient department. J Dent Sci 2023;18(3):1073-8.
[Crossref] [Google Scholar] [PubMed]
- Chen LL, Lei YQ, Liu JF, Cao H, Yu XR, Chen Q. Application and effects of an early childhood education machine on analgesia and sedation in children after cardiothoracic surgery. J Cardiothorac Surg 2021;16(1):118.
[Crossref] [Google Scholar] [PubMed]
- Huang YL, Xu N, Huang ST, Wang ZC, Cao H, Yu XR, et al. Impact of music therapy on preoperative anxiety and degree of cooperation with anesthesia induction in children with simple congenital heart disease. J Perianesth Nurs 2021;36(3):243-6.
[Crossref] [Google Scholar] [PubMed]
- Deshpande P, Salcedo B, Haq C. Common sleep disorders in children. Am Fam Physician 2022;105(2):168-76.
[Google Scholar] [PubMed]
- Alantali K, Al-Halabi M, Hussein I, El-Tatari A, Hassan A, Kowash M. Changes in preschool children's oral health-related quality of life following restorative dental general anaesthesia. Br Dent J 2020;229(10):670-6.
[Crossref] [Google Scholar] [PubMed]
- Yu LS, Xie WP, Liu JF, Wang J, Cao H, Wang ZC, et al. A comparison of the outcomes of dexmedetomidine and remifentanil with sufentanil-based general anesthesia in pediatric patients for the transthoracic device closure of ventricular septal defects. J Cardiothorac Surg 2021;16:1-7.
[Crossref] [Google Scholar] [PubMed]
- Devi EA, Nagaprasad YR, Shiva PV, Nirmalan P. Incidence and risk factors for emergence delirium in children undergoing surgery under general anaesthesia-A prospective, observational study. Indian Anaesth 2023;67(8):725-9.
[Crossref] [Google Scholar] [PubMed]
- Baxter R, Merkel-Walsh R, Baxter BS, Lashley A, Rendell NR. Functional improvements of speech, feeding, and sleep after lingual frenectomy tongue-tie release: A prospective cohort study. Clin Pediatr 2020;59(9-10):885-92.
[Crossref] [Google Scholar] [PubMed]
- Liu B, Tang W, Li H, Liu R, Dong F, Guo Y, et al. Point-of-care detection of sevoflurane anesthetics in exhaled breath using a miniature TOFMS for diagnosis of postoperative agitation symptoms in children. Analyst 2022;147(11):2484-93.
- Huang L, Wang L, Peng W, Qin C. A comparison of dexmedetomidine and propofol on emergence delirium in children undergoing cleft palate surgery with sevoflurane-based anesthesia. J Craniofac Surg 2022;33(2):650-3.
[Crossref] [Google Scholar] [PubMed]
- Ignatiuk D, Schaer B, McGinley B. High flow nasal cannula treatment for obstructive sleep apnea in infants and young children. Pediatr Pulmonol 2020;55(10):2791-8.
[Crossref] [Google Scholar] [PubMed]
- Bitners AC, Arens R. Evaluation and management of children with obstructive sleep apnea syndrome. Lung 2020;198(2):257-70.
[Crossref] [Google Scholar] [PubMed]
- Feng Z, Shi X, Yan X, Zhu Y, Gu J, Zhu H, et al. Comparing the effects of dexmedetomidine vs. propofol on the treatment of emergence agitation in adult patients after general anesthesia: Study protocol for a randomized, superiority, controlled trial (DP-TEA Trial). Trials 2021;22:1-9.
[Crossref] [Google Scholar] [PubMed]
- Shi Y, Zhang X, Sun Y, Mei E, Wan X, Li T. Emergence agitation after the cleft lip or palate surgery in pediatric patients: A prospective study. J Stomatol Oral Maxillofac Surg 2021;122(6):539-43.
[Crossref] [Google Scholar] [PubMed]
- Huang YL, Lei YQ, Xie WP, Cao H, Yu XR, Chen Q. Effect of music therapy on infants who underwent mechanical ventilation after cardiac surgery. J Cardiac Surg 2021;36(12):4460-4.
[Crossref] [Google Scholar] [PubMed]
- Wu JP. Pediatric anesthesia concerns and management for orthopedic procedures. Pediatr Clin 2020;67(1):71-84.
[Crossref] [Google Scholar] [PubMed]
- Lin Z, Fang Y, Yan L, Lin Y, Liu M, Zhang B, et al. General vs. general anaesthesia combined with caudal block in laparoscopic-assisted Soave pull-through of Hirschsprung disease: A retrospective study. BMC Anesthesiol 2021;21:1-6.
[Crossref] [Google Scholar] [PubMed]
- Knaus ME, Koppera S, Lind MN, Cooper JN. Sociodemographic differences in care plans and time to treatment among children being considered for adenotonsillectomy. Otolaryngol Head Neck Surg 2022;166(6):1106-17.
[Crossref] [Google Scholar] [PubMed]
- Liu Q, Fu J, Yu Q, Gong W, Li P, Guo X. Laparoscopic surgery of intra‑abdominal lymphatic malformation in children. Exp Ther Med 2022;24(3):1-6.
[Crossref] [Google Scholar] [PubMed]
- Opfermann P, Marhofer P, Springer A, Metzelder M, Zadrazil M, Schmid W. A prospective observational study on the feasibility of subumbilical laparoscopic procedures under epidural anesthesia in sedated spontaneously breathing infants with a natural airway. Pediatr Anesth 2022;32(1):49-55.
[Crossref] [Google Scholar] [PubMed]
 Experimental group
Experimental group
 Experimental group
Experimental group



