- *Corresponding Author:
- Dongyan Wang
The Second Affiliated Hospital of Heilongjiang University of Traditional Chinese Medicine,
Harbin,
Heilongjiang 150000,
China
E-mail: zhenjiuzqs@163.com
| This article was originally published in a special issue, “Novel Therapeutic Approaches in Biomedicine and Pharmaceutical Sciences” |
| Indian J Pharm Sci 2021:83(6) Spl Issue “180-190” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
To evaluate the clinical effect and effectiveness of acupuncture therapy in the treatment of insomnia patients, so as to provide better evidence based services, benefit patients and promote it in clinical practice. Chinese databases were searched: China National Knowledge Infrastructure, Chinese Scientific Journals Full text Database, Wanfang data knowledge service platform; English databases were searched: PubMed, Cochrane Library, Embase. Stata 15.1 and RevMan 5.4.1 software were used for statistical analysis. A total of 22 randomized controlled trials (1572 cases) were included, including 780 in the experimental group and 792 in the control group. An analysis showed that the effective rate of acupuncture treatment for insomnia was better than that of Western medicine treatment and the combined effect odds ratio=1.23, 95 % confidence interval [1.17, 1.29]. Pure acupuncture group in Pittsburgh sleep quality experienced surpasses the Western medicine group evaluation combined effect of weighted mean difference=2.04, 95 % confidence interval [1.62, 2.46], p<0.01; In each score of Pittsburgh sleep quality index, sleep quality weighted mean difference=-0.27, 95 % confidence interval [-0.40, -0.13], p<0.01, time to fall asleep weighted mean difference=-0.21, 95 % confidence interval [-0.37, -0.06], p<0.01, sleep efficiency weighted mean difference=-0.30, 95 % confidence interval [-0.42, -0.19], p<0.01, sleep disorder weighted mean difference=-0.22, 95 % confidence interval [-0.41, -0.04], p<0.01, hypnotic drugs weighted mean difference=-0.79, 95 % confidence interval [-1.01, -0.57], p<0.01, daytime function weighted mean difference=-0.39, 95 % CI [-0.59, -0.19], p<0.01. All of the acupuncture groups were better than the Western medicine groups. In the sleep time weighted mean difference=-0.30, 95 % confidence interval [-0.05, 0.18], p=0.73, there was no statistical significance between the acupuncture group and the Western medicine group. Pure acupuncture has more advantages than Western medicine in the treatment of insomnia and it is suitable for clinical promotion.
Keywords
Acupuncture, insomnia, systematic evaluation, meta-analysis
Insomnia is a disease characterized by frequent failure to get normal sleep. It is clinically manifested as having difficulty in falling asleep, sleeping lightly, being unable to fall asleep after waking up, having a broken sleep and so on, and being sleepless all night in severe cases. Sleep deprivation may also affect the cognitive, emotional and other functions, with such symptoms as dizziness, headache, fatigue, memory loss and emotional instability. In addition, negative emotions such as anxiety and depression, climacteric syndrome and other conditions can also result in insomnia. According to the Traditional Chinese Medicine (TCM), insomnia occurs when a pathogen invades Zang-fu organs, causing defensive qi flow on the exterior instead of entering the interior. Despite a certain effect in the treatment of insomnia, the Western medicine used is mainly sedative drugs, most of which have adverse reactions such as addiction and withdrawal syndrome [1], and their discontinuation may easily lead to a rebound or even aggravation of symptoms. Compared with Western medicine, acupuncture is easier to operate in the treatment of sleep-related diseases, and has such advantages as significant curative effect, few adverse reactions and high safety, which thus is suitable for clinical promotion and application [2]. However, the author has not found the Meta-analysis of acupuncture vs. Western medicine in the treatment of insomnia in domestic and foreign literature. Therefore, metaanalysis was used in this paper to study the difference of effective rate and Pittsburgh Sleep Quality Index (PSQI) between acupuncture and Western medicine in the treatment of insomnia, so as to provide evidence- based medicine for this issue and promote more high quality randomized controlled trials in China and foreign countries.
Materials and Methods
Inclusion criteria:
Study type: All Randomized Controlled Trials (RCTs) where acupuncture therapy was used for the treatment of insomnia were performed according to the randomized control requirements and the languages were Chinese and English.
Subjects: Subjects should meet the diagnostic criteria of Chinese and Western medicine for insomnia, have no serious organic diseases, and be in all gender and age groups and in any course of disease.
Interventions: The experimental group was treated with acupuncture; the control group was treated with Western medicine. The acupuncture treatment included routine acupuncture, electroacupuncture, eye acupuncture and so on. Patients were treated in any course.
Outcome indicators: Effective rate; PSQI.
Exclusion criteria:
Non-randomized controlled trial; Multiple therapies were combined in the treatment groups; The control group was not treated with Western medicine alone; There was only abstract and the full text could not be extracted; The experimental design and outcome indicators were not met; The treatments and procedures were not clear; The scale evaluation was improper or the data were unclear and could not be extracted.
Search strategy:
English databases, including PubMed, Cochrane Library and Embase and Chinese databases, including China National Knowledge Infrastructure (CNKI), China Science and Technology Journal Full-Text Database (CQVIP) and Wanfang Data Knowledge Service Platform (WangFang Data), were searched by computer. The search followed the Patient, Intervention, Comparison And Outcomes (PICOS) principle; the research time was from the establishment of the database to March 2021. To avoid omissions, references of the included literature were viewed manually.
Literature selection:
First, literature to be searched was merged and deduplicated using NoteExpress. Then, two evaluators independently read the title and abstract, and read the full text, extracted the data and evaluated the quality after including the preliminarily selected literature. The two evaluators crosschecked their results. In case of any discrepancy, the two evaluators could discuss and decide after carefully reading the full text and if necessary, a third evaluator could assist in the decision.
Data extraction:
The extracted data included author’s name and publication time of literature, research methods, information of included sample (age, gender and course of disease of patients), intervention plan and methods (therapy and acupoint selection), outcome indicators and other contents.
Literature quality evaluation:
The risk of bias of the included literature was evaluated by the bias risk evaluation manual recommended by Cochrane collaboration, including-Selection bias: Random sequence generation and allocation concealment; Performance bias: Blinding of participants and personnel; Detection bias: Blinding of outcome assessment; Follow-up bias: Integrity of outcome data; Reporting bias: Selective reporting; other bias. Two evaluators evaluated each article of literature one by one and made the decisions of “yes” (low risk of bias), “no” (high risk of bias) and “unclear” (lack of information or uncertainty about the bias). Finally, the two evaluators crosschecked their results, and in case of any discrepancy, they could decide through discussion or seek the assistance of a third evaluator. If all the above items are of low risk, the risk of bias is low, representing the low risk of bias; if more than two (not including two) items are not described or the subjects cannot be contacted, the risk of bias is unclear, representing unclear risk of bias; if one or more items are of high risk, the risk of bias is high, representing high risk of bias. The funnel plot was used to evaluate the publication bias of the included literature.
Statistical methods:
Stata 15.1 and RevMan 5.4.1 software provided by Cochrane library were used for analysis. According to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) principle, the included literature data were analyzed for heterogeneity (I2), where I2≤50 % suggested that there was no obvious heterogeneity among the studies and fixed effect model was used for analysis; I2>50 % suggested that there was heterogeneity among the studies, and random effect model was used, and sensitivity analysis or subgroup analysis was performed for the source of heterogeneity. The included binary variables were expressed by Odds Ratio (OR) as the effect magnitude and 95 % Confidence Interval (CI); the included continuous variables were expressed by Weighted Mean Difference (WMD) as the effect magnitude and 95 % CI. If enough literature was included for the outcome indicators, funnel plots were made to analyze the publication bias. If the study was further conducted, Begg’s and Egger’s tests were conducted to further detect the publication bias.
Literature selection results:
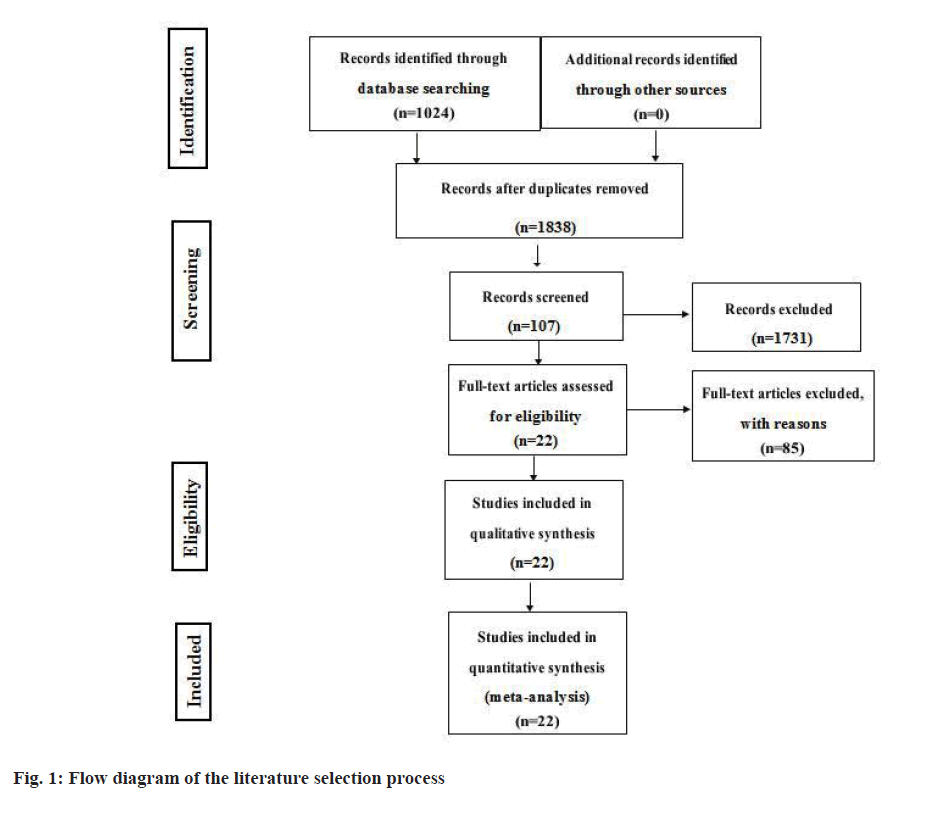
A total of 2572 articles of literature were preliminarily included, including 576 English articles and 1996 Chinese articles. Then, 734 articles were removed after duplicate checking, 1731 articles were removed after reading titles and abstracts, and 85 articles were removed after further reading the full text. Finally, 22 articles of randomized controlled trials were included for meta-analysis. Results are shown in fig. 1.
Characteristics of included literature:
A total of 22 articles of literature were included [3,4], including 7 thesis [3-10], 14 periodical articles [11,24] and 1 conference article [9]. All the articles were about randomized controlled trials. The experimental group was treated with acupuncture and the control group was treated with Western medicine. Patients were in any age and gender group and any course of disease. A total of 1572 patients were included, with 780 patients in the experimental group and 792 patients in the control group. Effective rate was selected as the outcome indicator in 21 articles [3-24], Pittsburgh Sleep Quality Index (PSQI) in 22 articles [4-24], Chinese medicine symptom complex score in 2 articles [5-10] and adverse reaction in 2 articles [6,10]. Details are shown in Table 1 and Table 2.
| Included study | Sample size (male/female) | Age (x?±s, year) | Baseline comparability | Insomnia type | Insomnia course (x?±s) | Outcome indicator | |||
|---|---|---|---|---|---|---|---|---|---|
| T | C | T | C | T | C | ||||
| Ren et al.[23] | 30 (11/19) | 29 (11/18) | 56.8±9.14 | 56.2±8.69 | Comparable | Insomnia with heart-spleen deficiency | (52.1±11.2) d | (54.5±12.1) d |  |
| Liu et al.[14] | 45 (23/22) | 45 (21/24) | 36.74±9.31 | 35.66±8.99 | Comparable | Insomnia with heart-spleen deficiency | (25.3±7.6) m | (25.9±10.3) m |  |
| Liu et al.[15] | 96 | 95 | 21-70 | 23-68 | Comparable | Insomnia | (3-32) m | (4-34) m |  |
| Wu et al.[10] | 27 (11/16) | 27 (12/15) | 42.26±13.39 | 39.15±13.09 | Comparable | Insomnia | (8.37±5.34) y | (7.30±4.94) y |  |
| Zhou et al. [16] | 30 (12/18) | 30 (14/16) | 49.1±16.7 | 48.7±15.4 | Comparable | Insomnia with heart-kidney imbalance | (14.0±10.5) m | (14.1±10.4) m |  |
| Zhou et al.[6] | 37 (9/28) | 36 (17/29) | 19-72; Mean: 40.81 | Comparable | Primary insomnia | 2 m-18 y; Mean: 4.52 y |  |
||
| Zhang et al.[11] | 30 (16/14) | 30 (19/11) | 35.1±12.9 | 37.4±14.5 | Comparable | Insomnia | (13.3±6.7) m | (10.5±5.1) m |  |
| Xu et al.[13] | 45 (17/28) | 45 (15/30) | 49.11±3.62 | 49.50±4.01 | Comparable | Insomnia | (4.83±3.79) m | (4.40±3.01) m |  |
| Li et al.[9] | 30 (16/14) | 30 (12/18) | 44.80±11.12 | 43.67±10.72 | Comparable | Insomnia | (4.60±1.61) m | (4.38±1.40) m |  |
| Li et al.[3] | 30 (11/20) | 30 (12/18) | 59.50±8.11 | 58.20±7.83 | Comparable | Middle and elderly aged insomnia | (9.52±4.66) y | (8.93±4.73) y |  |
| Li et al.[17] | 64 (20/44) | 64 (21/43) | 51.0±12.5 | 45.1±12.4 | Comparable | Chronic insomnia | (18.6±1.33) m | (19.1±1.28) m |  |
| Yang et al.[4] | 31 | 31 | 50.45±3.50 | 48.97±2.88 | Comparable | Perimenopausal insomnia | ≥30 d |  |
|
| Yin et al.[7] | 30 (13/17) | 30 (11/19) | 43.43±13.52 | 46.80±12.95 | Comparable | Insomnia | (19.87±7.21) m | (19.9.±6.70) m |  |
| Tang et al.[24] | 34 (18/16) | 31 (17/14) | 58.25±9.31 | 59.68±8.73 | Comparable | Insomnia after stroke | (28.64±10.36) d | (30.18±8.55) d |  |
| Wang et al.[20] | 33 (14/19) | 30 (12/18) | 73±6 | 73±6 | Comparable | Senile insomnia | (15.0±7.1) m | (15.1±7.3) m |  |
| Wang et al.[8] | 30 (13/17) | 30 (12/18) | 44.67±8.36 | 45.13±9.82 | Comparable | Simple insomnia | 9.3±4.80 | 9.5±4.41 |  |
| Bai et al.[21] | 30 (13/17) | 30 (14/16) | 38.36±13.52 | 39.23±13.14 | Comparable | Insomnia | (46.89±16.32) d | (43.35±15.94) d |  |
| Su et al.[5] | 30 (20/10) | 30 (18/12) | 18-60 | Comparable | Insomnia with deficiency syndrome | 1 m-20 y |  |
||
| Xie et al.[18] | 43 (22/21) | 40 (21/19) | 56.94±9.83 | 58.15±12.20 | Comparable | Insomnia after stroke | (34.93±13.41) d | (37.57±14.92) d |  |
| Zhou et al.[19] | 30 (19/11) | 30 (17/13) | 54.32±6.09 | 54.15±6.26 | Comparable | Insomnia | (57.90±9.37) d | (57.74±9.51) d |  |
| Zhou et al.[12] | 23 (13/10) | 23 (12/11) | 38.2±3.9 | 37.3±3.5 | Comparable | Insomnia | (29.1±5.5) m | (28.6±5.1) m |  |
| Hao et al.[22] | 27 (13/14) | 27 (12/15) | 57.7±8.25 | 58.02±7.96 | Comparable | Insomnia after stroke | (8.68±3.05) d | (8.97±2.83) d |  |
Note:  Effective rate;
Effective rate; Pittsburgh Sleep Quality Index (PSQI);
Pittsburgh Sleep Quality Index (PSQI);  Rheology test;
Rheology test; Hamilton Anxiety Scale (HAMA);
Hamilton Anxiety Scale (HAMA); Hamilton Depression Scale (HAMD);
Hamilton Depression Scale (HAMD); Compliance evaluation;
Compliance evaluation;  Chinese medicine symptom complex score;
Chinese medicine symptom complex score; Evaluation of Mattress Sleep Monitoring System;
Evaluation of Mattress Sleep Monitoring System;  SPIEGEL Scale Score;
SPIEGEL Scale Score; Athens Insomnia Scale (AIS);
Athens Insomnia Scale (AIS);  Self-Rating Scale of Sleep (SRSS);
Self-Rating Scale of Sleep (SRSS);  Treatment Emergent Symptom Scale (TESS)
Treatment Emergent Symptom Scale (TESS)
| Included study | Therapy (experimental) | Acupoint (experimental) | Therapy (control) | Course of treatment |
|---|---|---|---|---|
| Ren et al.[23] | Acupuncture for nourishing spleen and heart | Zusanli, Pishu, Shenmen, Sanyinjiao, Xinshu, Neiguan | Eszopiclone 1-3 mg/d | 4 w |
| Liu et al.[14] | Electroacupuncture | Taiyang, Sishencong, Zusanli, Sanyinjiao | Diazepam 5 mg/d | 10 d |
| Liu et al.[15] | Acupuncture from 3 pm to 7 pm | Sishencong, Anmian, Shenmen, Sanyinjiao, Taixi | Estazolam 1 mg/d | 24 d |
| Wu et al.[10] | Jin tri-points | Dingshen-Needle, Depression Three-Needle (Sishen-Needle, Neiguan, Sanyinjiao) | Surazepam 1-2 mg/d | 4 w |
| Zhou et al. [16] | Acupuncture for regulating mentality and supplementing kidney | Shangxing, Yintang, Baihui, Sishencong, Neiguan and Shenmen, Sanyinjiao, Taixi | Estazolam 1 mg/d | 4 w |
| Zhou et al.[6] | Scalp seven needles combined with primary collaterals and acupoints | Baihui, Sishencong, Anmian | Alprazolam 0.4 mg/d | 4 w |
| Zhang et al.[11] | Routine acupuncture | Feishu, Pishu, Ganshu, Xinshu, Shenshu | Stilnox 10 mg/d | 4 w |
| Xu et al.[13] | Eye acupuncture intraorbital method | Upper jiao, Hepatic region, Splenic region, Renal region, Middle jiao | Eszopiclone 1 mg/d | 2 w |
| Li et al.[9] | Routine acupuncture | Baihui, Neiguan, Shenmen, Sishencong | Estazolam 1 mg/d | 4 w |
| Li et al.[3] | Routine acupuncture | Shenmen, Baihui, Sishencong, Fengchi, Anmian | Estazolam 1 mg/d | 4 w |
| Li et al.[17] | Routine acupuncture | Shenmen, Neiguan, Sanyinjiao | Oxazepam 7.5-15 mg/d | 4 w |
| Yang et al.[4] | Routine acupuncture | Anmian, Geshu, Taichong, Ganshu (bilateral), Baihui, Sishencong | Estazolam 0.5-1 mg/d | 4 w |
| Yin et al.[7] | Routine acupuncture | Neiguan, Waiguan, Shenmen, Sanyinjiao | Estazolam 1 mg/d | 4 w |
| Tang et al.[24] | Routine acupuncture | Shenting, Benshen, Shenmen | Estazolam 2 mg/d | 4 w |
| Wang et al.[20] | Routine acupuncture | Shenmen, Sanyinjiao, Anmian, Baihui, Sishencong | Surazepam 1 mg/d; Oryzanol 20 mg/tid | 4 w |
| Wang et al.[8] | Tongyuan therapy | Wuzangshu, Baihui, Yintang, Tianshu, Guanyuan, Qihai | Estazolam 1mg/d | 4 w |
| Bai et al.[21] | Electroacupuncture | Shenmai, Zhaohai, Fuyang, Pucan, Jiaoxin, Rangu, Qingming | Estazolam 1 mg/d | 4 w |
| Su et al.[5] | Routine acupuncture | Shenmen, Zhizheng, Taibai, Fenglong | Estazolam 2 mg/d | 4 w |
| Xie et al.[18] | Routine acupuncture | Sanyinjiao, Shenmen, Sishencong, Shenting and the auricular point Shenmen | Estazolam 2 mg/d | 4 w |
| Zhou et al.[19] | Point opening according to midnight-noon ebb-flow | Sishencong, Baihui | Zopiclone 7.5 mg/d | 4 w |
| Zhou et al.[12] | Routine acupuncture | Anmian, Sishencong, Shenmen, Sanyinjiao, Zhongwan | The dose of the routine Western medicine An Mian increased gradually | 30 d |
| Hao et al.[22] | Acupoint matching with specimen | Zusanli, Guanyuan, Hegu, Baihui | Estazolam 0.5-1 mg/d | 4 w |
Table 2: Table of Literature Characteristics
Quality evaluation of included literature:
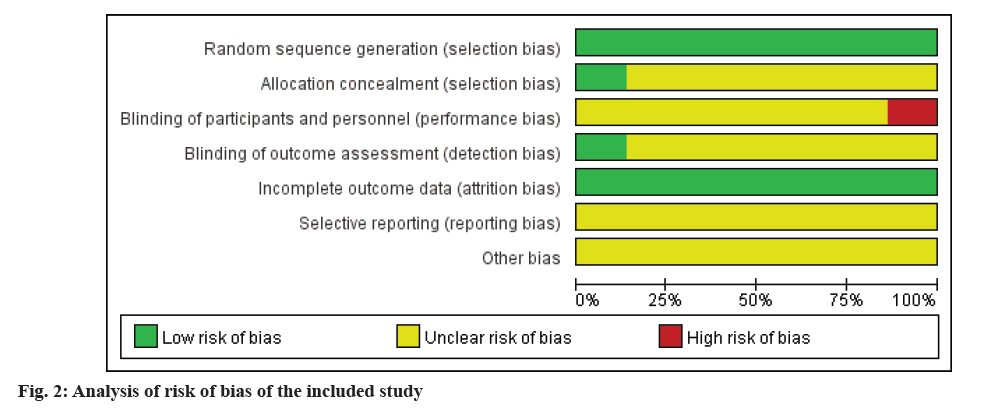
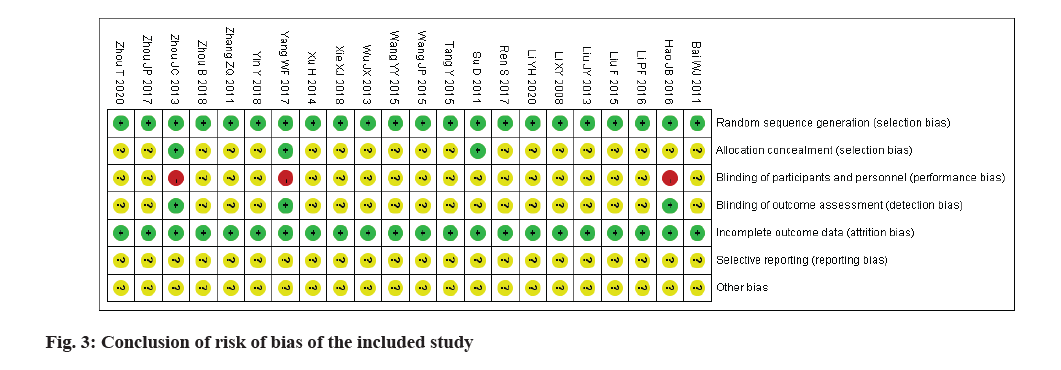
All the 22 articles of literature included were randomized using random number table; baseline information was reported in the 22 articles of literature and all factors were comparable; allocation concealment was mentioned in 3 articles [4-6], suggesting that sealed envelopes were used to conceal the allocation; blinding was used in 3 articles [4,6,22] and no double blind was used in them; no intentional analysis was used in all the included articles of literature; there was no selective reporting in all the included articles of literature; no other bias was mentioned in all the included articles of literature. RevMan 5.4 software provided by Cochrane was used and the specific bias evaluation analysis and percentage are shown in fig. 2 and fig. 3.
Meta-analysis of acupuncture vs. Western medicine in the treatment of insomnia:
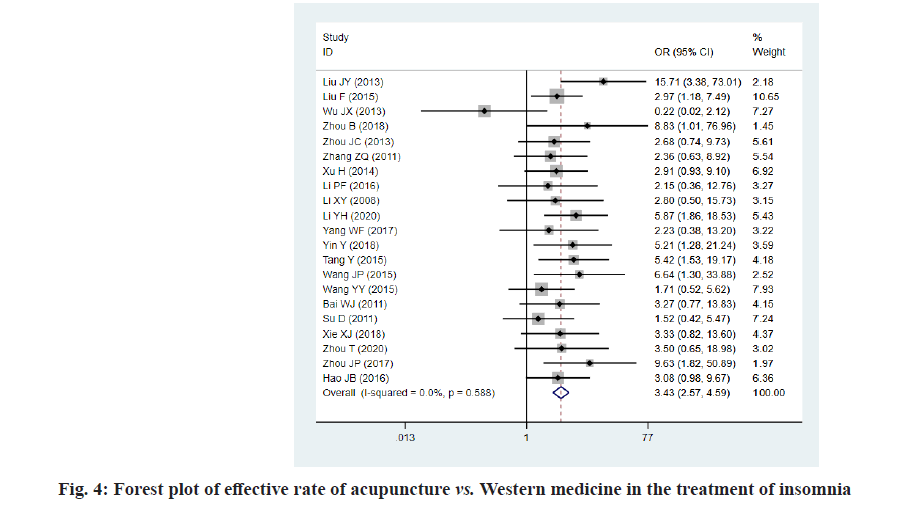
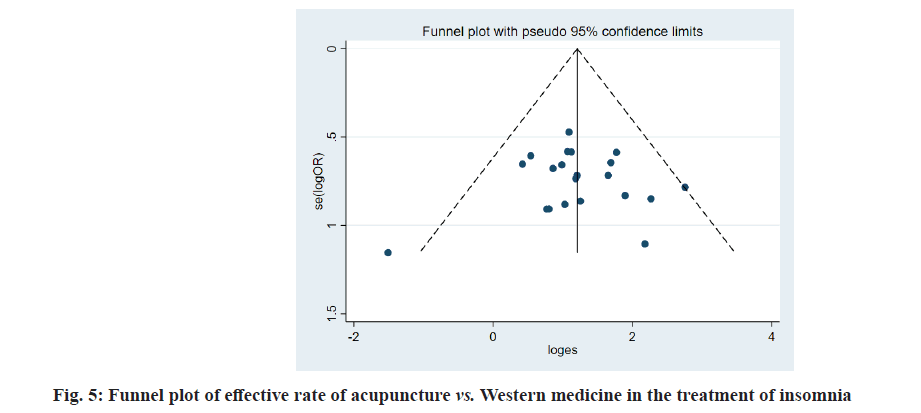
Effective rate: In the 22 articles of literature included, effective rate was used as the outcome indicator in 22 articles; heterogeneity test showed that I2=43.2 % (I2≤50 %), suggesting that there was no obvious heterogeneity among the studies and the fixed effect model was used for analysis. The pooled effect sizes were OR=1.23, 95 % CI [1.17, 1.29] and p<0.01. 0.01<p<0.05 suggested that there was significant difference, or the clinical effective rate of acupuncture vs. Western medicine in the treatment of insomnia had high statistical significance. The analysis results (fig. 4) suggested that the effective rate of acupuncture in the treatment of insomnia was better than that of Western medicine. The funnel plot (fig. 5) showed that the sample results were asymmetrically distributed around the population effect, suggesting that there was large bias. At the same time, Begg’s and Egger’s tests were conducted and the results were p=0.002/p=0.005, suggesting that there was publication bias. Then, the effect of publication bias on the results was further discussed (characteristic of this bias detection method: Indicators with less than 7 included studies were not tested) by trim and filling method and the low effect suggested that the results had good authenticity.
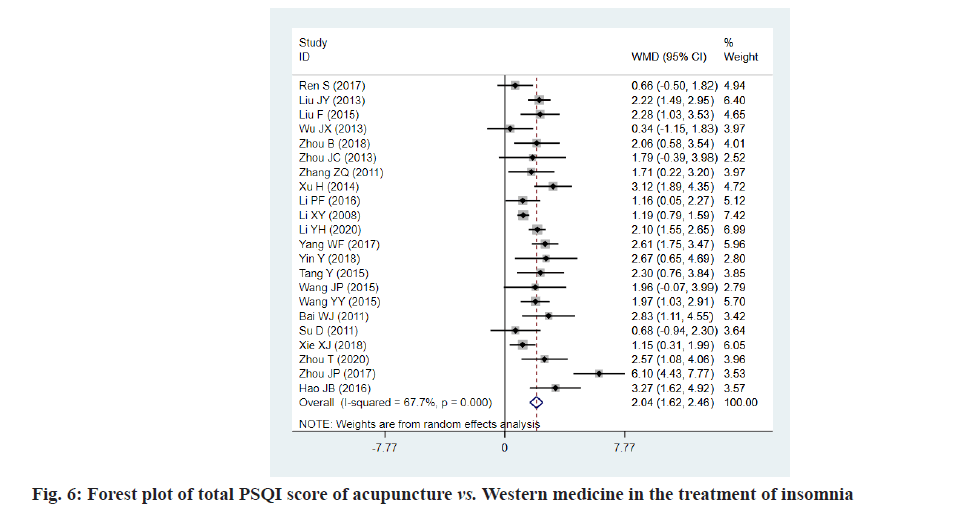
PSQI score: In all the 22 articles of literature included [3-24], PSQI score was used as the outcome indicators. A total of 1572 cases were included, with 780 cases in the experimental group and 792 cases in the control group. Heterogeneity test showed that I2=67.7 % (I2>50 %), suggesting that there was heterogeneity and random effect model was used, and sensitivity analysis or subgroup analysis was performed for the source of heterogeneity. The pooled effect sizes were WMD=2.04, 95 % CI [1.62, 2.46] and p→0, and p<0.01 suggested highly significant difference. The analysis results (fig. 6) suggested that the PSQI score of acupuncture in the treatment of insomnia was better than that of Western medicine. Begg’s and Egger’s tests were conducted and the results showed that p=0.481/ p=0.084, suggesting that there was small bias.
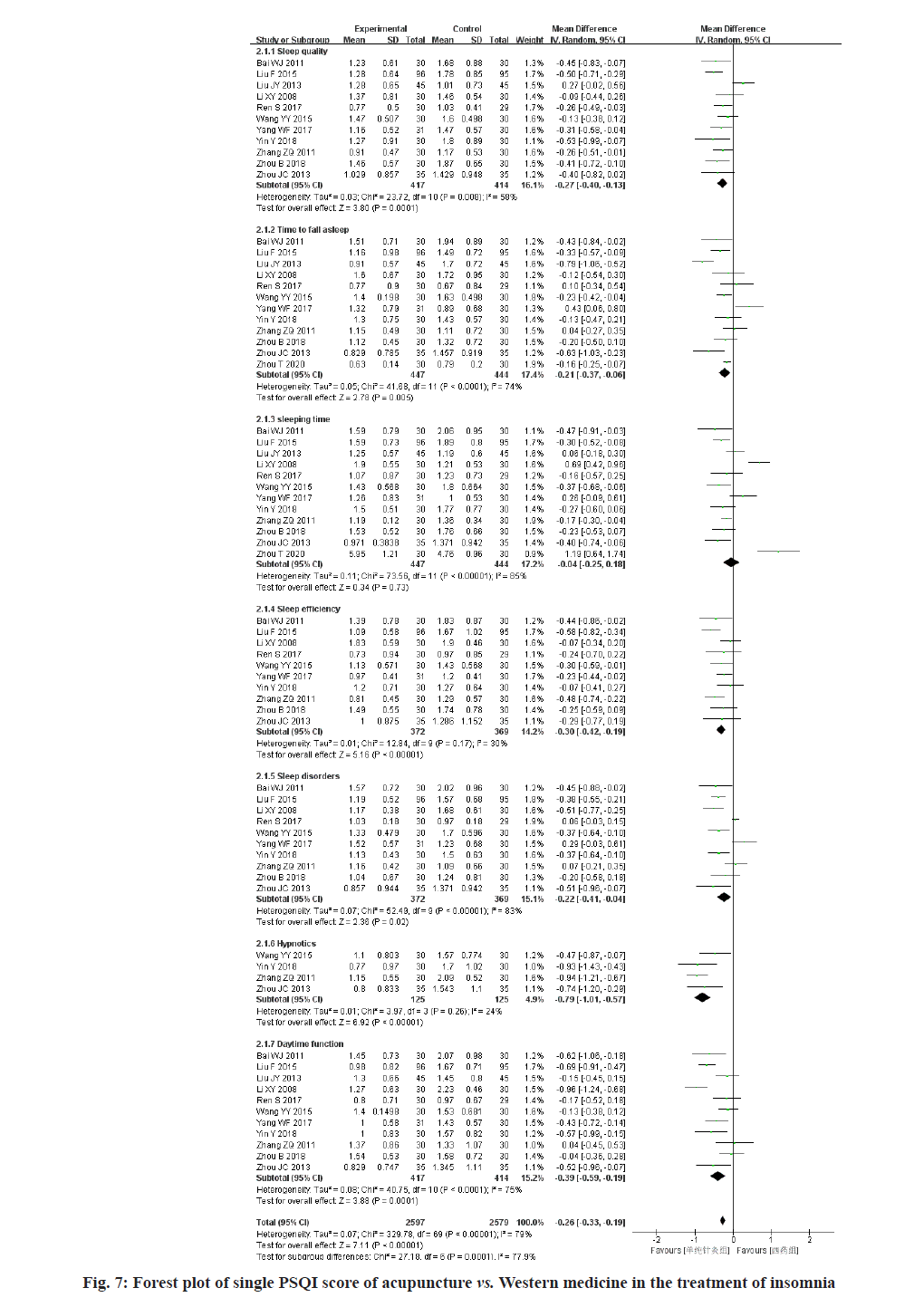
Sleep quality was recorded in 11 articles of literature [3-16,21,23] and the results showed that the sleep quality of acupuncture in the treatment of insomnia was better than that of Western medicine. Heterogeneity test showed that I2=58 %, suggesting that the heterogeneity was high; sensitivity analysis was conducted and the results showed that high heterogeneity did not affect the stability of conclusion. Begg’s and Egger’s tests were conducted and the results were p=0.102 and p=0.773, suggesting that there was no obvious publication bias. The pooled effect sizes were WMD=-0.27, 95 % CI [-0.40, -0.13] and p<0.01.
Time to fall asleep was recorded in 11 articles of literature [3-19,21,23] and the results showed that the time to fall asleep of acupuncture in the treatment of insomnia was better than that of Western medicine. Heterogeneity test showed that I2=74 %, suggesting that the heterogeneity was high; sensitivity analysis was conducted and the results showed that high heterogeneity did not affect the stability of conclusion. Begg’s and Egger’s tests were conducted and the results were p=1.000/p=0.740, suggesting that there was no obvious publication bias. The pooled effect sizes were WMD=-0.21, 95 % CI [-0.37, -0.06] and p<0.01.
Sleeping time was recorded in 12 articles of literature [3-19,21,23] and the forest plot showed that the sleeping time results of acupuncture vs. Western medicine in the treatment of insomnia were ineffective. Heterogeneity test showed that I2=85 %, suggesting that the heterogeneity was high; sensitivity analysis was conducted and the results showed that the sensitivity was high and the conclusion was instable. The confidence interval of the results obtained after removing Liu et al. passed through the invalid line, so the results obtained were instable. Begg’s and Egger’s tests were conducted and the results were p=0.493/p=0.447, suggesting that there was no obvious publication bias. The pooled effect sizes were WMD=-0.30, 95 % CI [-0.05, 0.18] and p=0.73.
Sleep efficiency was recorded in 10 articles of literature [3-16,21,23] and the results showed that the sleep efficiency of acupuncture in the treatment of insomnia was better than that of Western medicine. Heterogeneity test showed that I2=30 %, suggesting that there was no obvious heterogeneity among the studies. Begg’s and Egger’s tests were conducted and the results were p=0.788/p=0.683, suggesting that there was no obvious publication bias. The pooled effect sizes were WMD=- 0.30, 95 % CI [-0.42, -0.19] and p<0.01.
Sleeping disorders were recorded in 10 articles of literature [3-16,21,23] and the results showed that the sleeping disorders of acupuncture in the treatment of insomnia were lower than those of Western medicine. Heterogeneity test showed that I2=83 %, suggesting that the heterogeneity was high; sensitivity analysis was conducted and the results showed that high heterogeneity did not affect the stability of conclusion. Begg’s and Egger’s tests were conducted and the results were p=0.421/p=0.107, suggesting that there was no obvious publication bias. The pooled effect sizes were WMD=-0.22, 95 % CI [-0.41, -0.04] and p<0.01.
Hypnotics were recorded in 4 articles of literature [6,8,11,21] and the results showed that the hypnotics of acupuncture in the treatment of insomnia were better than those of Western medicine. Heterogeneity test showed that I2=24 %, suggesting that there was no obvious heterogeneity among the studies. Begg’s and Egger’s tests were conducted and the results were p=1.000/p=0.594, suggesting that there was no obvious publication bias. The pooled effect sizes were WMD=-0.79, 95 % CI [-1.01, -0.57] and p<0.01.
Daytime function was recorded in 11 articles of literature [3-16,21,23] and the results showed that the daytime function of acupuncture in the treatment of insomnia was better than that of Western medicine. Heterogeneity test showed that I2=79 %, suggesting that the heterogeneity was high; sensitivity analysis was conducted and the results showed that high heterogeneity did not affect the stability of conclusion. Begg’s and Egger’s tests were conducted and the results were p=0.815/p=0.484, suggesting that there was no obvious publication bias. The pooled effect sizes were WMD=-0.39, 95 % CI [-0.59, -0.19] and p<0.01. Details are shown in fig. 7.
Heterogeneity Analysis
After data processing, sensitivity analysis was conducted on those with high heterogeneity (I2>50 %) and it was speculated that the reasons might be that: The included patients had different courses of disease, ages and genders (for example, only female patients were included for perimenopausal insomnia), so there were individual differences in samples; the included patients had different types of insomnia. Some patients were included in insomnia according to TCM syndromes (such as syndrome of heart-kidney imbalance and syndrome of heart-spleen deficiency), some were included in the primary insomnia, perimenopausal insomnia, senile insomnia and some were included in insomnia regardless of types. Different types of insomnia had different prognosis and outcomes; the included patients were treated in different courses and with different methods. In the experimental groups, some patients were treated by routine acupuncture, some by dialectical acupoint selection and some by other acupuncture methods (such as Tongyuan therapy and Jin tri-points); in the control group, most patients were treated with Estazolam, and some with other Western medicines (such as Stilnox and Eszopiclone) and the dose was not uniform, which might cause different outcomes; The same score used for outcome indicators in the included studies may differ in the influence of subjective and objective factors, such as different understandings of use of the same scale or the interference by subjective evaluation of authors of the literature.
Discussion
In TCM, insomnia is a kind of disease characterized by frequent failure to get normal sleep. Insomnia is treated based on the principle of regulating yin and yang of Zang-fu organs, mainly by tonifying deficiency and reducing excess. Acupuncture, as a special treatment in TCM, is used to dredging the channel, regulating yin and yang, strengthening body resistance and eliminating evil through the conduction of meridians, collaterals and acupoints, so as to treat the systemic diseases. After years of clinical study, the author has found that acupuncture of Sishencong, Baihui, Houxi, Lieque, Anmian and Gongxue is effective in the clinical treatment of insomnia. Acupuncture of Sishencong [25] can nourish heart and tranquilize mind and soothe liver and relieve depression, thus improving the structure of sleep; acupuncture of Baihui [26] around which there are abundant blood vessels can treat insomnia. Modern studies have also confirmed that acupuncture can make patients in a state of qi-blood harmony, peaceful yin and compact yang in the treatment of insomnia [27,28], thus improving the sleep quality of patients. Purpose of this paper is to collect high-quality clinical randomized controlled trials and strictly evaluate and analyze them one by one and then statistically process the data by quantitative synthesis and objectively evaluate them, so as to draw the comprehensive conclusion. The conclusion is drawn from the effective rate and PSQI score of acupuncture vs. Western medicine in the treatment of insomnia, which provides clinical evidence-based evidence for acupuncture treatment of insomnia.
Based on the data of literature included in this paper, it can be concluded that the effective rate of acupuncture in the treatment of insomnia was 90.43 % and that of Western medicine was 73.72 %, suggesting that the effective rate of acupuncture was higher than that of Western medicine. In subjective sleep quality, sleep latency, habitual sleep efficiency, sleep disorders, use of hypnotics and daytime dysfunction, the heterogeneity of habitual sleep efficiency and use of hypnotics was low and the results were more stable. The results can provide certain clinical hints, where patients in an urgent need to improve insomnia (such as those affected by long-term insomnia, in poor emotions and of short temper) can be treated by acupuncture to improve their sleep quality and reduce their dependence on hypnotics, so that they can better return to the family and society, improve their compliance and obtain a better treatment outcome.
In addition, there are also some limitations in this study, such as different scoring criteria included and few articles of literature on long term followup. Therefore, international unified standard should be used in the evaluation of insomnia by RCTs and long term follow-up should be added as the outcome observation indicators; TCM scoring criteria should be improved and subjective human factors should be reduced in RCTs of acupuncture to avoid the impact on the authenticity of the results. In this paper, metaanalysis of acupuncture vs. Western medicine in the treatment of insomnia is described, which is instructive to the subsequent clinical treatment, despite the limited quality of literature included in the study. Based on clinical experience, the therapy of acupuncture combined with medicine has a better clinical effect in the treatment of insomnia, compared with a single therapy. At the same time, more large-sample and high quality randomized controlled trials are expected to provide evidence-based medical evidence and further verify the conclusion.
Conflict of interests:
The authors declared no conflicts of interest.
References
- Croke LM. Treatment of chronic insomnia in adults: ACP guideline. Am Fam Physician 2017;95(10):669-70.
- Dongyan W, Ruoyu W, Lei H, Jinglan F. Research progress of acupuncture in the treatment of obstructive sleep apnea hypopnea syndrome. Liaoning J Tradit Chin Med 2020;1-7.
- Li XY, Zhou ZL, Zhang B. Clinical observation on acupuncture for treating middle or elderly aged patients with insomnia. Tianjing J Tradit Chin Med 2010;27:386-8.
- Wanfang Y. A clinical study about the liver treatment of insomnia on the menopausal transition by acupuncture. Chengdu Univ Tradit Chin Med 2017.
- Su D, Zhao J, Jin H. The clinical efficacy of acupuncture at Yuan–primary point and Luo–connecting point of the heart meridian (HT) for the treatment of deficiency insomnia. J Clin Acupunct Moxibustion 2011;27:34-6.
- Jingchao Z. Randomized controlled clinical study on treatment of primary insomnia by the head acupoint working in with yuan-source points and collateral-points combination. Chengdu Univ Tradit Chin Med 2013.
- Yuan Y. The clinical observation on penetration needling of complementary acupoints for insomnia. Chengdu Med Univ 2018.
- Yayun W. Clinical study of insomnia with the treatment of Tongdutianshen-Yinqiguiyuan. Guangzhou Univ Chin Med 2015.
- Peifang L. Evaluation and analysis of clinical pathway effect of acupuncture in treating insomnia 2016.
- Wu CH. Clinical study on the treatment of insomnia by Jin tri-points. Guangzhou Univ Chin Med 2013.
- Zhiqiang Z. Clinical observation of acupuncture of five internal organs back shu for the treatment of insomnia. Guangming J Chin Med 2011;26(8).
- Zou J. Observation of clinical effect of acupuncture for the treatment of insomnia. Henan Med Res 2017;26(8).
- Xu H, Wang P, He W. Clinical Observation on Eye-Acupuncture in Treatment of Insomnia. J Liaoning Univ Tradit Chin Med 2014:08.
- Liu J, Wei X. Clinical observation of electro-acupuncture treating insomnia deficiency. Shenzhen J Integr Tradit Chin West Med 2013;23(3).
- Liu F, Wang L, Wei QP, Wang ZH. Clinical curative observation of applying acupuncture at shen-you time to regulate 196 cases of insomnia. Journal Sichuan Tradit Chin Med 2015;33(8):174-6.
- Zhou B, Yuan Z, Feng H. Curative effect observation of 30 cases insomnia with heart yang kidney yin in coordination by regulating spirit and tonifying kidney acupuncture method. Tianjin J Tradit Chin Med 2018;35(4).
- Li Y, Li H, Wang J. Clinical Study on acupuncture-moxibustion in treatment of chronic insomnia. Systems Med 2020;5(22).
- Xie X. Clinical effect of acupuncture in the treatment of sleep disorders after stroke and its effect on nerve function. Mod J Integr Tradit Chin West Med 2018;27(29).
- Zou T, Su L, Zhou A. Midnight-noon ebb-flow acupoint-opening method in the treatment of sleep disorder. Chin J Clin Res 2020;33(4).
- Wang J, Wang L, Zhang Y. Senile insomnia treated with integrated acupuncture and medication therapy: a randomized controlled trial. Zhongguo Zhen Jiu 2015;35(6):544-8.
- Bai WJ, Zhang ZQ. Clinical study of heel vessel acupuncture treating insomnia. Chin Arch Tradit Chin Med 2011;29:413-4.
- Hao J, Zhou H, Wang Y. Biao-Ben points association warm-acupuncture combined with head and back massage therapy on insomnia after cerebral infarction. Chin Arch Tradit Chin Med 2016;34(7).
- Shuang R, Jie Z, Xu H. Clinical observation of invigorating spleen and nourishing heart acupuncture treatment on insomnia. Chin J Tradit Chin Med Pharm 2017;32(9).
- Tang Y, Zhang S. Clinical observation of acupuncture of “Sanshen point” for the treatment of insomnia after stroke. Chin J Integr Med Cardiovasc Dis 2015;13(16).
- Song DJ, He L, Zhang R, Dong X. Research progress of EX-HN1. J Clin Acupuncture Moxibustion 2018;34(2):82-4.
- Xue-Fen WU, Zheng XN, Yan WA, Xiao-Li CH, Li LI, Xin-Ran WE, et al. Acupuncture at acupoints along the meridians for primary insomnia: a multi-center randomized controlled trial. Zhongguo Zhen Jiu 2020:465-71.
- Pi M, Chen PD, Yang ZX, Yu HB, Luo WS, Wu YG, et al. Effect of governor vessel electro-acupuncture plus hucb-mscs transplantation on neurological deficit scores and cellular apoptosis of cerebral ischemia-reperfusion rats. Lishizhen Med Materia Medica Res 2014;25:492-5.
- Yang Z, Chen P, Yu H, Luo W, Pi M, Wu Y, et al. Combinatorial effects of conception and governor vessel electroacupuncture and human umbilical cord blood-derived mesenchymal stem cells on pathomorphologic lesion and cellular apoptosis in rats with cerebral ischemia/reperfusion. J Tradit Chin Med 2013;33(6):779-86.