- *Corresponding Author:
- Li Xu
Department of Neurology, The Third Affiliated Hospital of Zhejiang Chinese Medical University, Hangzhou, Zhejiang 310009, China
E-mail: xuli725@163.com
| This article was originally published in a special issue, “Transformative Discoveries in Biomedical and Pharmaceutical Research” |
| Indian J Pharm Sci 2023:85(4) Spl Issue “142-148” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
To investigate the potential clinical utility of ultrasound elastography in the diagnosis and management of infants with congenital muscular torticollis. We conducted searches in PubMed, Embase, Web of Science and Cochrane library databases and limited the search time from the database was created in April 2023. Articles were screened according to inclusion and exclusion criteria. RevMan (version5.3) is used for meta-analysis. The study results were presented using either standard mean difference or mean difference as statistical measures to compare the difference between two groups and 95 % confidence intervals for consecutive outcomes. Chi-square test was used to calculate I2 to detect the heterogeneity between studies and then appropriate effect models were selected according to I2 or p values. Publication offset was evaluated using funnel plots. Of the 5 studies included. The years of publication ranged from 2013 to 2021, with sample sizes ranging from 20 to 120. Ultrasonic measurements of sternocleidomastoid muscle thickness (mean difference was 0.57, 95 % confidence intervals was -0.42-0.72, p<0.001). The A/U ratio of sternocleidomastoid muscle measured by ultrasound was (mean difference was -0.45, 95 % confidence interval was -1.56-0.66, p=0.42). Ultrasound imaging may be a useful adjunct to the evaluation of B ultrasound in sternocleidomastoid muscle infants. However, further high quality clinical trial studies are needed to obtain stronger clinical evidence.
Keywords
Sternocleidomastoid muscle, computed tomography, muscular torticollis, ultrasound
Congenital Muscular Torticollis (CMT) is a common cervical deformity in children, mainly caused by Sternocleidomastoid Muscle (SCM) contracture, which is typically characterized by a tilted head to the affected side and rotation of the mandible to the healthy side. Currently, the diagnosis of CMT mainly depends on history, physical examination, and imaging[1-3]. However, traditional imaging methods such as X-ray and Computed Tomography (CT) have problems such as high radiation dose, failure to assess soft tissue elasticity and failure to fully assess the extent of lesions in SCM[4-6]. Clinically, the lesion hardness of CMT is positively correlated with fibrosis, and the accurate evaluation of the lesion degree of CMT is very important for the judgment of treatment and prognosis. A non-invasive, low-risk, accurate and repeatable diagnostic method is of great significance for the diagnosis and treatment of pediatric muscular torticollis[7-10].
Traditional imaging methods, such as X-ray and CT, have problems such as high radiation dose, failure to evaluate soft tissue elasticity, and failure to comprehensively evaluate the degree of lesions in SCM[11]. Therefore, it is of great significance to develop a low-cost, noninvasive and repeatable diagnostic method for the diagnosis and treatment of pediatric muscular torticollis[12]. In recent years, ultrasound technology has attracted wide attention as a low-cost, non-invasive and reproducible imaging method[13-16]. It can provide more comprehensive and accurate diagnostic information. In recent years, some studies have shown that Virtual Touch Tissue Imaging Quantization (VTIQ) technique has high accuracy and reliability in the diagnosis of pediatric muscular torticollis, which has important clinical application value in guiding the treatment and monitoring the efficacy of pediatric muscular torticollis. The purpose of this meta-analysis was to evaluate the accuracy and reliability of ultrasound in the diagnosis of pediatric muscular torticollis, and to explore its clinical application value. In this context, this paper will systematically comb the existing relevant literature, and summarize and analyze the performance of ultrasonic technology in the diagnosis of pediatric muscular torticollis, in order to provide clinicians with more accurate and reliable diagnostic methods, and provide better guidance for the treatment of pediatric muscular torticollis.
Materials and Methods
Search strategy:
We searched the keywords related to "ultrasound", "muscular torticollis" and "children" in PubMed, Embase, Web of Science and Cochrane Library databases. The search time was limited from the establishment of the database to April 2023.
Qualification criteria:
Research types: Only observational studies and Randomized Controlled Trials (RCTs) on ultrasonic diagnosis of pediatric muscular torticollis were included. Non-RCTs, case reports and animal studies, and reviews were excluded.
This statement discusses the inclusion and exclusion criteria for a study on pediatric muscular torticollis in individuals aged 0-18 y old. The study includes children with this diagnosis but excludes those with torticollis caused by other medical conditions.
Intervention: This meta-analysis only focused on the diagnostic value of ultrasound technology without limiting intervention measures.
Comparison: In this meta-analysis, no control group interventions were involved and any therapeutic interventions were excluded.
Result measurement: The primary outcome was ultrasound diagnosis of pediatric muscular torticollis. The thickness and stress ratio of the mass in the SCM muscle was evaluated.
Research selection and data extraction:
Research options: When the authors searched the relevant literature in PubMed, Embase, Web of Science, Cochrane Library and other databases, the title and abstract were first screened and the full text was finally screened. Screening criteria included, RCTs or controlled clinical trials; the objective of the study was to evaluate the diagnostic value of ultrasound in pediatric muscular torticollis; data of control group and intervention group were included and provide adequate data. Evaluation of the thickness and stress ratio of the mass in the SCM muscle in the diagnosis of pediatric muscular torticollis by ultrasound. Two evaluators independently performed the screening process and cross-checked against the selection criteria. Differences between the two reviewers are resolved through negotiation, but if consensus is still lacking, a third reviewer is involved to reach an agreement.
Data extraction: Two evaluators independently extracted the publication year, first author name, publication date, study country and sample size of the included articles. Patient characteristics such as age, gender, intervention, methods of ultrasound examination (e.g., type of ultrasound probe, scanning mode, etc.) and results shown by ultrasound (e.g., thickness and stress ratio assessment of mass in SCM muscle, etc.) and ultrasound results. Thickness and stress ratio of mass in SCM muscle in case of differences in data extraction results, consensus is reached through discussion among all authors. All data will be summarized and analyzed to calculate the diagnostic value of ultrasound in pediatric muscular torticollis.
Risk assessment:
The risk assessment method of meta-analysis can be referred to the Cochrane bias risk tool. It mainly includes generating random sequence, including deviation factors, such as generating random sequence, hiding, defining blind method and incomplete result information and other biases. For migration risk assessment, it can be divided into the following aspects; migration type, data source selection, sample selection and processing, data analysis and result presentation. Each aspect can also be classified by risk level as low, unclear or high. The evaluation can be conducted independently by multiple authors and differences can be resolved through discussion. Finally, all evaluation results should be summarized to obtain the overall bias risk assessment results of meta-analysis, and possible bias factors should be discussed and explained in the results to improve the credibility and reliability of the study.
Statistical analysis:
ReviewManager (RevMan) version5.3 is used for meta-analysis. The data were summarized using Standardized Mean Difference (SMD) or Mean Difference (SMD) and 95 % Confidence Intervals (CI) for consecutive outcomes. Chi-square test was used to calculate I2 to detect the heterogeneity between studies, and then appropriate effect models were selected according to I2 or p values. When I2>50 % or p<0.05, indicating the possibility of significant heterogeneity, random effects model was used; otherwise, fixed effects model was used. We then assessed publication bias by observing the symmetry of the funnel plot. p>0.05 was considered to indicate the absence of publication bias and the results were presented in the form of pictures.
Results and Discussion
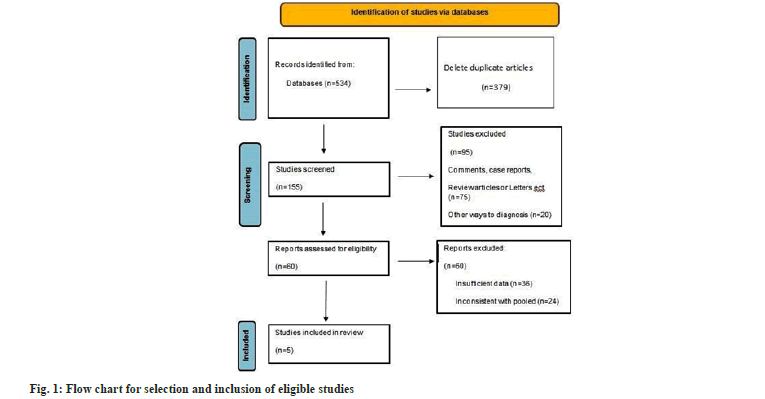
Using the prepared search strategy, a search was conducted in each database and a total of 534 articles were obtained after the selected study. By screening the titles or abstracts of all articles and the inclusion criteria, 84 studies that could not be included, such as repeated reports 379, conference abstracts, reviews and case reports were excluded,and 60 literatures that could not obtain the full text were excluded. Finally, it was determined that the included 5 studies met the inclusion criteria by browsing the full text. A total of 280 patients were included[11-19] (fig. 1). Of the 5 studies included[17-21], 3 were RCTs and 2 were retrospective studies, 4 were conducted in Korea and 1 was conducted in China. The years of publication ranged from 2013 to 2021, with sample sizes ranging from 20 to 120.The main features of these studies are summarized in Table 1.
| Study | Year | Country | Number of cases (experimental/control group) | Mean age | Male/female |
|---|---|---|---|---|---|
| Seong | 2016 | South Korea | 29/24 | 30.92±21.72 | 35,18 |
| Mi | 2020 | South Korea | 16041 | 23.65 | 50,5 |
| Hyeng | 2013 | South Korea | 67/66 | 24.21 | 81,52 |
| Zhang | 2021 | China | 9,10 | 13.1±77.8 | 11,8 |
| Gi | 2018 | South Korea | 11,9 | 69.0±26.2 | 12,8 |
Table 1: Baseline features included in the study.
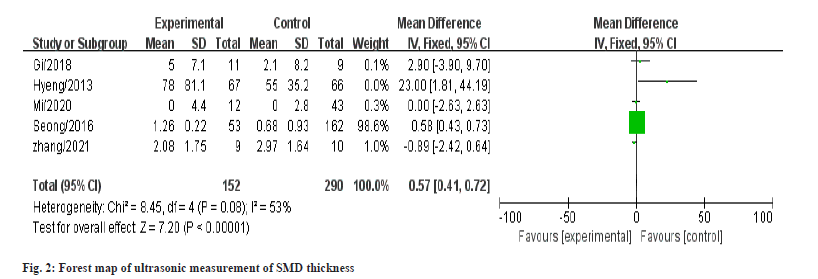
Five studies evaluated ultrasonography measures of SCM muscle thickness involving 442 patients. In five studies, the intergroup difference in favor of the experimental group was reported as p<1.2 in one study, p<0.1, and the final meta results showed that ultrasonic measurements of SCM muscle thickness were (MD: 0.57, 95 % CI: -0.42 to 0.72, p<0.001) with moderate heterogeneity (p=0.8, I2=53 %, fig. 2).
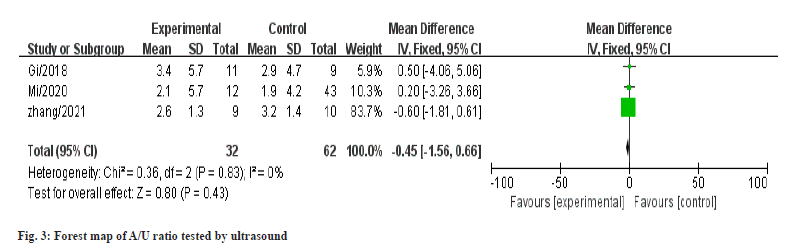
A total of three articles involved ultrasound testing of patients with neck A/U ratio including a total of 94 patients. Forest map results showed that A/U ratio of SCM muscle measured by ultrasonography was (MD: -0.45, 95 % CI: -1.56 to 0.66, p=0.42), which had no statistical significance and no heterogeneity (I2=0 %, p=0.83), as shown in fig. 3.
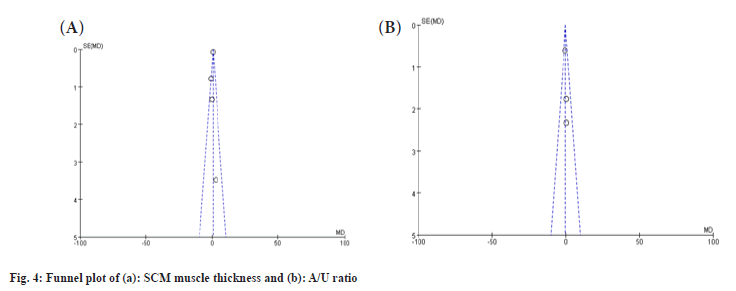
For SCM muscle thickness and A/U ratio, SMDS and their associated 95 % CI were combined and analyzed by funnel plot test to assess publication bias. The results are shown in fig. 4a and fig. 4b. Funnel plots of SCM muscle thickness and A/U ratio showed good symmetry.
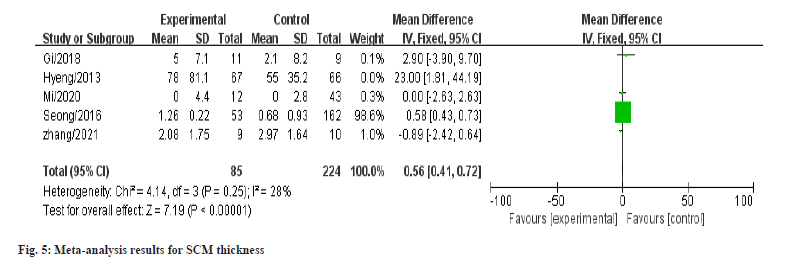
The meta-analysis was deemed dependable and strong as removing any literature did not considerably alter the results in the sensitivity analysis. Heterogeneity was detected in the meta-analysis results for SCM thickness, with an I2 of over 50 %, but after excluding the (MI/2020) study, the I2 decreased to 28 % as shown in fig. 5.
CMT is a common childhood neuromuscular disease. The main manifestations of the children are head tilt to the affected side after birth, hard tumor-like mass in the involved SCM[22-24], and crooked or twisted neck. If not treated in time, the patient may have head tilt, facial asymmetry and other symptoms, leading to other secondary deformities[25]. It may affect children's life and study. Therefore, early diagnosis and treatment are very important. Ultrasound is a non-invasive, non-radioactive imaging method that can detect changes in neck muscles and nerves[26-28]. It is the primary diagnostic tool for CMT, which can detect the thickness of SCM and muscle fiber thickening. In this paper, a meta-analysis was conducted on the diagnostic value of ultrasound in pediatric muscular torticollis, and its clinical significance[29]. Limitations and suggestions for further research discusses the use of VTIQ technology for diagnosing and monitoring children with CMT[30-33]. VTIQ is a real-time elastography technique that measures tissue elasticity in response to back pressure. The study found that the Square Wave Voltammetry (SWV) of the affected side in children with CMT was significantly greater than that of the healthy side, and the VTIQ technique can provide a more objective and accurate means of diagnosis. Furthermore, the mean SWV was positively correlated with head deviation and muscle hardness, suggesting that VTIQ can also evaluate the effectiveness of treatment for CMT[34-37].
The results of this study showed that ultrasonic measurements of SCM muscle thickness (MD: 0.57, 95 % CI: -0.42 to 0.72, p<0.001). A/U ratio of the SCM muscle measured by ultrasound was (MD: -0.45, 95 % CI: -1.56-0.66, p=0.42). The affected SCM mass grows in response to environmental changes after birth, undergoes differentiation and maturation, and then produces CMT. In this study, no evidence of neck or SCM injury was found in the physical examination screening of 442 newborns. In addition, ultrasound examination found no evidence of neck injury in infants with CMT. This raises questions about the quality of ultrasonic SCM. Overall, our results provide new insights into ultrasonic inspection SCM. These findings may help improve ultrasound diagnosis and treatment of SCM, thereby helping to reduce patient suffering and improve quality of life.
There are some limitations to this meta-analysis. First, due to resource and time constraints, ultrasound cannot be performed on every child with pediatric muscular torticollis and some patients may be missed. Secondly, because some patients or their parents do not comply with the study protocol or are difficult to follow, some data may be missing or follow-up may be lost. In addition, as this meta-analysis is a retrospective study, there may be some selection bias, reporting bias or other possible bias, which may affect the accuracy of the conclusions. In addition, the diagnostic criteria for muscular torticollis may vary, which may also influence the results. Therefore, these limitations need to be noted when interpreting the results.
In conclusion, ultrasound imaging may be a useful adjunct to the evaluation of B-type ultrasound in SCM infants, especially in predicting the recovery outcome of SCM infants.
Conflict of interests:
The authors declared no conflict of interests.
References
- Le Neindre A, Philippart F, Luperto M, Wormser J, Morel-Sapene J, Aho SL, et al. Diagnostic accuracy of diaphragm ultrasound to predict weaning outcome: A systematic review and meta-analysis. Int J Nurs Stud 2021;117:103890.
[Crossref] [Google Scholar] [PubMed]
- Mahmoodpoor A, Fouladi S, Ramouz A, Shadvar K, Ostadi Z, Soleimanpour H. Diaphragm ultrasound to predict weaning outcome: Systematic review and meta-analysis. Anaesthesiol Intensive Ther 2022;54(2):164-74.
[Crossref] [Google Scholar] [PubMed]
- Kim GH, Kim PH, Shin JH, Nam IC, Chu HH, Ko HK. Ultrasound-guided sclerotherapy for the treatment of ovarian endometrioma: An updated systematic review and meta-analysis. Eur Radiol 2022;32(3):1726-37.
[Crossref] [Google Scholar] [PubMed]
- Liu W, Zhang ZY, Yin SS, Yan K, Xing BC. Contrast-enhanced intraoperative ultrasound improved sensitivity and positive predictive value in colorectal liver metastasis: A systematic review and meta-analysis. Ann Surg Oncol 2021;28:3763-73.
[Crossref] [Google Scholar] [PubMed]
- Mhanna M, Beran A, Nazir S, Sajdeya O, Srour O, Ayesh H, et al. Lung ultrasound–guided management to reduce hospitalization in chronic heart failure: A systematic review and meta-analysis. Heart Fail Rev 2021;27(3):821-6.
[Crossref] [Google Scholar] [PubMed]
- Ucci MA, di Mascio D, Bellussi F, Berghella V. Ultrasound evaluation of the uterus in the uncomplicated postpartum period: A systematic review. Am J Obstet Gynecol 2021;3(3):100318.
[Crossref] [Google Scholar] [PubMed]
- Liu L, Wang T, Lei B. Ultrasound-guided microwave ablation in the management of symptomatic uterine myomas: A systematic review and meta-analysis. J Minim Invasive Gynecol 2021;28(12):1982-92.
[Crossref] [Google Scholar] [PubMed]
- Hirooka M, Koizumi Y, Sunago K, Nakamura Y, Hirooka K, Watanabe T, et al. Efficacy of B-mode ultrasound-based attenuation for the diagnosis of hepatic steatosis: A systematic review/meta-analysis. J Med Ultrason 2022;49(2):199-210.
[Crossref] [Google Scholar] [PubMed]
- Xydias EM, Kalantzi S, Tsakos E, Ntanika A, Mpeis N, Prior M, et al. Comparison of 3D ultrasound, 2D ultrasound and 3D Doppler in the diagnosis of endometrial carcinoma in patients with uterine bleeding: A systematic review and meta-analysis. Eur J Obstet Gynecol Reprod Biol 2022;277:42-52.
[Crossref] [Google Scholar] [PubMed]
- Rahman MI, Chan BP, Far PM, Mbuagbaw L, Thabane L, Yaghoobi M. Endoscopic ultrasound vs. computed tomography in determining the resectability of pancreatic cancer: A diagnostic test accuracy meta-analysis. Saudi J Gastroenterol 2020;26(3):113-9.
[Crossref] [Google Scholar] [PubMed]
- Kaplan SL, Coulter C, Sargent B. Physical therapy management of congenital muscular torticollis: A 2018 evidence-based clinical practice guideline from the American physical therapy association academy of pediatrics physical therapy. Pediat Phys Ther 2018;30(4):240-90.
[Crossref] [Google Scholar] [PubMed]
- Kaplan SL, Coulter C, Fetters L. Physical therapy management of congenital muscular torticollis: An evidence-based clinical practice guideline. Pediatr Phys Ther 2013;25(4):348-94.
[Crossref] [Google Scholar] [PubMed]
- Suhr MC, Oledzka M. Considerations and intervention in congenital muscular torticollis. Curr Opin Pediatr 2015;27(1):75-81.
[Crossref] [Google Scholar] [PubMed]
- Keklicek H, Uygur F. A randomized controlled study on the efficiency of soft tissue mobilization in babies with congenital muscular torticollis. J Back Musculoskelet Rehabil 2018;31(2):315-21.
[Crossref] [Google Scholar] [PubMed]
- Song S, Hwang W, Lee S. Effect of physical therapy intervention on thickness and ratio of the sternocleidomastoid muscle and head rotation angle in infants with congenital muscular torticollis: A randomized clinical trial (CONSORT). Medicine 2021;100(33):e26998.
[Crossref] [Google Scholar] [PubMed]
- Goel A, Shrivastava P, Goel A, Bhandari PS. Congenital muscular torticollis in ‘late-comers’: A proposal for grading of severity and outcome scales. J Plast Reconstr Aesthet Surg 2022;75(8):2831-70.
[Crossref] [Google Scholar] [PubMed]
- Hong SK, Song JW, Woo SB, Kim JM, Kim TE, Lee ZI. Clinical usefulness of sonoelastography in infants with congenital muscular torticollis. Ann Rehabil Med 2016;40(1):28-33.
[Crossref] [Google Scholar] [PubMed]
- Jeong MR, Lee IS, Shin YB, Song YS, Park S, Song JW, et al. Clinical efficacy of real-time Sonoelastography for the follow-up of congenital sternocleidomastoid muscle torticollis. Taehan Yongsang Uihakhoe Chi 2020;81(1):176-89.
[Crossref] [Google Scholar] [PubMed]
- Park HK, Kang EY, Lee SH, Kim KM, Jung AY, Nam DH. The utility of ultrasonography for the diagnosis of developmental dysplasia of hip joint in congenital muscular torticollis. Ann Rehabil Med 2013;37(1):26-32.
[Crossref] [Google Scholar] [PubMed]
- Zhang C, Ban W, Jiang J, Zhou Q, Li J, Li M. Two-dimensional ultrasound and shear wave elastography in infants with late-referral congenital muscular torticollis. J Ultrasound in Med 2019;38(9):2407-15.
[Crossref] [Google Scholar] [PubMed]
- Park GY, Kwon DR, Kwon DG. Shear wave Sonoelastography in infants with congenital muscular torticollis. Medicine 2018;97(6):e9818.
[Crossref] [Google Scholar] [PubMed]
- Chen SC, Ho YS, Suen LK, Yu J, Tang W, Jiang JF, et al. Traditional Chinese medicine (TCM) massage for the treatment of congenital muscular torticollis (CMT) in infants and children: A systematic review and meta-analysis. Complement Ther Clin Prac 2020;39:101112.
[Crossref] [Google Scholar] [PubMed]
- Amaral DM, Cadilha RP, Rocha JA, Silva AI, Parada F. Congenital muscular torticollis: Where are we today? A retrospective analysis at a tertiary hospital. Porto Biomed J 2019;4(3):e36.
[Crossref] [Google Scholar] [PubMed]
- Greve KR, Sweeney JK, Bailes AF, Van Sant AF. Infants with congenital muscular Torticollis: Demographic factors, clinical characteristics, and physical therapy episode of care. Pediatr Phys Ther 2022;34(3):343-51.
[Crossref] [Google Scholar] [PubMed]
- Seager A, Meldrum D, Conroy R, French HP. Congenital muscular torticollis: The reliability of visual estimation in the assessment of cervical spine active rotation and head tilt by physiotherapists and the impact of clinical experience. Eur J Pediatr 2020;179:1823-32.
[Crossref] [Google Scholar] [PubMed]
- Christensen C, Landsettle A, Antoszewski S, Ballard BB, Carey H, Pax Lowes L. Conservative management of congenital muscular torticollis: An evidence-based algorithm and preliminary treatment parameter recommendations. Phys Occup Ther Pediatr 2013;33(4):453-66.
[Crossref] [Google Scholar] [PubMed]
- Bashir A, Amjad F, Ahmad A, Arooj A, Gilani SA. Effect of physical therapy treatment in infants treated for congenital muscular torticollis-A narrative review. J Pak Med Assoc 2023;73(1):111-6.
[Crossref] [Google Scholar] [PubMed]
- Menon K, Schlapbach LJ, Akech S, Argent A, Biban P, Carrol ED, et al. Criteria for pediatric sepsis—A systematic review and meta-analysis by the pediatric sepsis definition taskforce. Crit Care Med 2022;50(1):21-36.
[Crossref] [Google Scholar] [PubMed]
- DeMarsh S, Huntzinger A, Gehred A, Stanek JR, Kemper KJ, Belsky JA. Pediatric osteopathic manipulative medicine: A scoping review. Pediatrics 2021;147(2).
[Crossref] [Google Scholar] [PubMed]
- Rahmati M, Keshvari M, Mirnasuri S, Yon DK, Lee SW, Il Shin J, et al. The global impact of COVID-19 pandemic on the incidence of pediatric new-onset type 1 diabetes and ketoacidosis: A systematic review and meta-analysis. J Med Virol 2022;94(11):5112-27.
[Crossref] [Google Scholar] [PubMed]
- Ricciuto A, Aardoom M, Orlanski-Meyer E, Navon D, Carman N, Aloi M, et al. Predicting outcomes in pediatric crohn’s disease for management optimization: Systematic review and consensus statements from the pediatric inflammatory bowel disease–ahead program. Gastroenterology 2021;160(1):403-36.
[Crossref] [Google Scholar] [PubMed]
- Tan Lim CS, Esteban Ipac NA, Recto MS, Castor MA, Casis Hao RJ, Nano AL. Comparative effectiveness of probiotic strains on the prevention of pediatric atopic dermatitis: A systematic review and network meta-analysis. Pediatr Allergy Immunol 2021;32(6):1255-70.
[Crossref] [Google Scholar] [PubMed]
- Patel P, Robinson PD, Wahib N, Cheung P, Wong T, Cabral S, et al. Interventions for the prevention of acute phase chemotherapy-induced nausea and vomiting in adult and pediatric patients: A systematic review and meta-analysis. Support Care Cancer 2022;30(11):8855-69.
[Crossref] [Google Scholar] [PubMed]
- Lee JJ, Philteos J, Levin M, Namavarian A, Propst EJ, Wolter NE. Clinical prediction models for suspected pediatric foreign body aspiration: A systematic review and meta-analysis. JAMA Otolaryngol Head Neck Surg 2021;147(9):787-96.
[Crossref] [Google Scholar] [PubMed]
- Patel RS, Veluri N, Patel J, Patel R, Machado T, Diler R. Second-generation antipsychotics in management of acute pediatric bipolar depression: A systematic review and meta-analysis. J Child Adolesc Psychopharmacol 2021;31(8):521-30.
[Crossref] [Google Scholar] [PubMed]
- Paller AS, Beck LA, Blauvelt A, Siegfried EC, Cork MJ, Wollenberg A, et al. Infections in children and adolescents treated with dupilumab in pediatric clinical trials for atopic dermatitis—A pooled analysis of trial data. Pediatr Dermatol 2022;39(2):187-96.
[Crossref] [Google Scholar] [PubMed]
- Sohouli MH, Farahmand F, Alimadadi H, Rahmani P, Motamed F, da Silva Magalhaes EI, et al. Vitamin D therapy in pediatric patients with inflammatory bowel disease: A systematic review and meta-analysis. World J Pediatr 2023;19(1):48-57.
[Crossref] [Google Scholar] [PubMed]