- *Corresponding Author:
- Purnima Amin
Department of Pharmaceutical Sciences and Technology, Institute of Chemical Technology, Nathalal Pareikh Marg, Matunga, Mumbai - 400 019, India
E-mail: dramin@vsnl.net
| Date of Submission | 13 June 2009 |
| Date of Revision | 14 September 2010 |
| Date of Acceptance | 10 November 2010 |
| Indian J Pharm Sci 2010, 72 (6): 704-709 |
Abstract
Trimetazidine dihydrochloride, a cellular antiischemic agent indicated in the management and prophylaxis of angina pectoris is given as 20 mg thrice daily in the conventional dosage regimen. The purpose of the present study was to formulate and evaluate twice a day extended release tablets containing 30 mg trimetazidine dihydrochloride. The method developed to formulate these extended release tablets was melt congealing followed by wet granulation which exhibited uniform sustained release action and overcame the drawbacks of multidosing. The formulation was developed with Methocel® K100M and stearic acid as release retardant.
Keywords
Extended release tablets, melt congealing, Methocel® K100M, stearic acid, trimetazidine dihydrochloride
The term ‘controlled release’ refers to a system that delivers a drug continuously for a predetermined period with predictable and reproducible kinetics, and a known mechanism of release. Controlled release drug delivery systems are usually designed applying physical and polymer chemistry to produce a well characterised and reproducible dosage form that controls drug delivery to the body within the specifications of the required drug delivery profile [1]. Controlled drug delivery systems can be classified as, continuous release systems, e.g. dissolution [2], diffusion [3], ion exchange [3] and osmotically controlled systems [4]; delayed transit and continuous release systems, such as density based [5] and size based bioadhesive based systems [6]; delayed release systems that include intestinal and colonic release systems [7]. Melt congealing [8] is a process, which comprises of forming a molten mixture containing drug and pharmaceutically accepted carrier, delivering the molten mixture to an atomizing means to form droplets and congealing the droplets to form multiparticulates.
Trimetazidine dihydrochloride is cytoprotective antianginal drug that displays antiischemic activity.
It is believed to act through a triple cytoprotective action, restoration of energy production, reduction of energy utilization and opposing the overproduction of free radicals [9-11]. Treatment of angina pectoris involves long term therapy. Conventional dosage regimen is 20 mg thrice daily. Hence the objective of our work was to formulate twice daily tablets containing 30 mg of drug to maintain steady drug blood levels, prolong therapeutic action and improved patient compliance.
Materials and Methods
Trimetazidine dihydrochloride was gifted by Cipla Ltd., Mumbai, India. Methocel® K100M and Ethocel® was gifted by Colorcon Asia Pvt. Ltd., Mumbai, India. All the excipients and chemicals used were of Analytical Reagent (AR) grade.
Preparation of tablets
All the formulations as shown in Table 1 were developed using direct compression method. Extended release trimetazidine dihydrochloride tablets were formulated by direct compression method. All the ingredients were weighed and passed through 40#. The drug, diluents and polymer were blended in an octagonal blender for 10 min. Then the mixture was lubricated using talc and magnessium stearate in a blender for 5 min. Different polymers were used as release retardants such as Methocel® K100M, Eudragit® RSPO, Ethocel® and cellulose acetate. All the batches prepared are summerised in Table 1. The lubricated mixture was then compressed on a Cadmach tabletting machine (Cadmach Machinery Co. Pvt. Ltd. Ahmedabad, India) using 10 mm standard concave punches. Tablet weight was set at 250 mg with hardness of 5-6 kg/cm2. Release specifications were set at 90% release in 10h.
| Batch/Formula | T1 (mg) |
T2 (mg) |
T3 (mg) |
T4 (mg) |
T5 (mg) |
T6 (mg) |
T7 (mg) |
|---|---|---|---|---|---|---|---|
| Trimetazidine dihydrochloride | 30.00 | 30.00 | 30.00 | 30.00 | 30.00 | 30.00 | 30.00 |
| Methocel®K100M | 65.00 | 90.00 | 125.00 | ------ | ------ | ------ | ------ |
| Eudragit®RSPO | ------ | ------ | ------ | 15.00 | 75.00 | ------ | ------ |
| Ethocel® N -20 | ------ | ------ | ------ | ------ | ------ | 60.00 | ------ |
| Ethocel® N-100 | ------ | ------ | ------ | ------ | ------ | ------ | 60.00 |
| Avicel®PH102 | 147.00 | 122.50 | 87.50 | 197.00 | 137.00 | 152.00 | 152.00 |
| Dibasic calcium phosphate | ------ | ------ | ------ | ------ | ------ | ------ | ------ |
| Talc | 5.00 | 5.00 | 5.00 | 5.00 | 5.00 | 5.00 | 5.00 |
| Magnesium stearate | 2.50 | 2.50 | 2.50 | 2.50 | 2.50 | 2.50 | 2.50 |
| Total 249.50 | 250.00 | 250.00 | 249.50 | 249.50 | 249.50 | 249.50 |
Table 1: Formulation Development
Formulations T8 to T11 were developed using wet granulation method [Table 2]. All the ingredients were weighed and passed through 40#. The mixture of drug, diluent and polymer were blended in planetary mixer for 20 min. Solution of polyvinyl pyrrolidone was prepared in isopropyl alcohol. This solution was added to form a wet mass along with mixing. The wet mass was passed through multimill having 8 mm screen. The wet granules were dried in fluidised bed dryer at 40° for 30 min. Dried granules were then passed through multimill having 2 mm screen. The dried granules were finally passed through 20#. The dried granules were lubricated using talc and magnessium stearate in a blender for 5 min. The granules were then compressed using 11 mm round flat faced punches with beveled edges. Tablet weight was set at 250 mg with hardness of 5-6 kg/cm2.
| Batch/Formula | T8 | T9 | T10 | T11 | T12 | T13 |
|---|---|---|---|---|---|---|
| (mg) | (mg) | (mg) | (mg) | (mg) | (mg) | |
| Trimetazidine dihydrochloride | 30.00 | 30.00 | 30.00 | 30.00 | 30.00 | 30.00 |
| Methocel® K100M | 120.00 | ------ | ------ | ------ | 120.00 | 150.00 |
| Ethocel® N - 20 | ------ | ------ | 120.00 | 150.00 | ------ | ------ |
| Cellulose acetate | ------ | 120.00 | ------ | ------ | ------ | ------ |
| Stearic acid | ------ | ------ | ------ | ------ | 90.00 | 180.00 |
| Dibasic calcium phosphate | 93.00 | 93.00 | 93.00 | 93.00 | 2.50 | 3.75 |
| Talc | 5.00 | 5.00 | 5.00 | 5.00 | 7.50 | 7.50 |
| Magnesium stearate | 2.50 | 2.50 | 2.50 | 2.50 | 3.75 | 3.75 |
| Polyvinylpyrrolidone dissolved in Isopropyl alcohol | 12.50 | 12.50 | 12.50 | 14.00 | ------ | ------ |
| Total | 263.00 | 263.00 | 263.00 | 294.50 | 253.50 | 375.00 |
Table 2: Formulation Development
Formulations T12 and T13 were developed using melt congealing method. All the ingredients were weighed and passed through 40#. Drug was dispersed in molten stearic acid and congealed. The mass was then screened through 20#. This was blended in a blender with diluent and Methocel® K100M. Solution of polyvinyl pyrrolidone was prepared in isopropyl alcohol and was added to form a wet mass. The wet mass was passed through multimill having 8 mm screen. The wet mass was dried in fluidized bed dryer and dry granules were then passed through 20#. Dried granules were lubricated using talc and magnessium stearate and compressed on cadmach tabletting machine on 11 mm round flat faced punches with beveled edges. Tablet weight was fixed at 375 mg with hardness of 4-5 kg/cm2.
Evaluation of tablets
The granules were evaluated for flow properties like Carr’s index, Hausner’s ratio, density (bulk and tap density), angle of repose and loss on drying. The tablets were evaluated for physical appearance, diameter, thickness, hardness, friability, drug content and in vitro release studies. Drug content was determined using developed HPTLC method [12]. In vitro release studies were carried out using USP Type І dissolution apparatus containing 200 ml of pH 1.2 hydrochloric acid buffer for 2 h and Phosphate buffer pH 7.2 for remaining 8 h. The apparatus was operated at 100 rpm at a temperature of 37±0.5°. 5 ml aliquots were withdrawn at 0.5, 1, 1.5, 2, 3, 4, 5, 6, 8, 10 h intervals and absorbance was recorded using UV spectrophotometry at λmax of 269 nm.
In vitro drug release characteristics
The mechanism of drug release from the matrix tablet was analyzed using Korsmeyer-Peppas [13] equation where Mt/M∞ is the fractional solute release, t is the release time, k is a kinetic constant characterisic of the drug/polymer system, A is the area of the sample, cd is the tracer loading concentration and n is an exponent which characterises the mechanism of release of the tracers. Mt/M∞ = ktn (1), dMt/Adt = ncdktn-1 (2), when the diffusional release exponent (n) is equal to 1 then it characterizes zero order drug release behaviour.
Similarity factor (f2) analysis
In vitro drug release profile of the marketed trimetzidine dihydrochloride sustained release tablets was compared with the drug release profile of test product under similar experimental conditions. The data obtained from this drug release studies was used to determine the similarity factor between marketed and test product. Similarity factor was calculated using the formula shown in Eqn. 3, f2 = 50 log{ [ 1+(1/N)å(Ri – Ti)2]-0.5´100} (3), where N is number of time points, Ri and Ti are dissolution of reference and test products at time i. If f2 is greater than 50 then it is considered that 2 products have similar drug release behavior [14].
Stability study
Accelerated stability studies [15] ensures stability of the product under exaggerated conditions of temperature and humidity. The optimized formulation was strip packed and subjected to stability studies at 25°/60%RH, 30°/65%RH and 40°/75%RH at regular intervals for 6 months. The tablets were evaluated for dimension, hardness, friability, drug content and in vitro release. Degradation was monitored by using stability indicating HPTLC method.
Results and Discussion
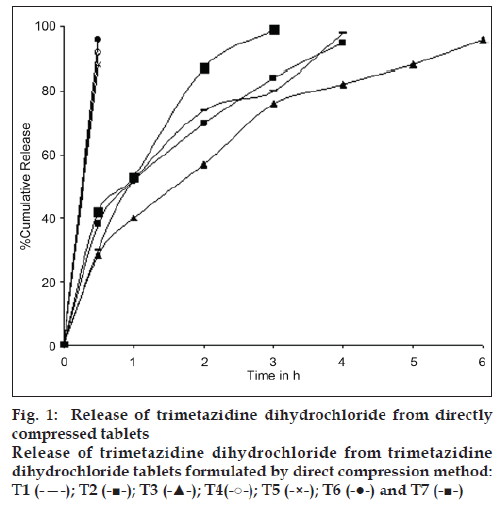
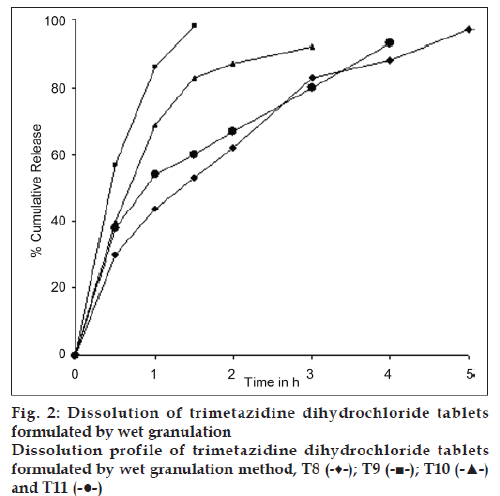
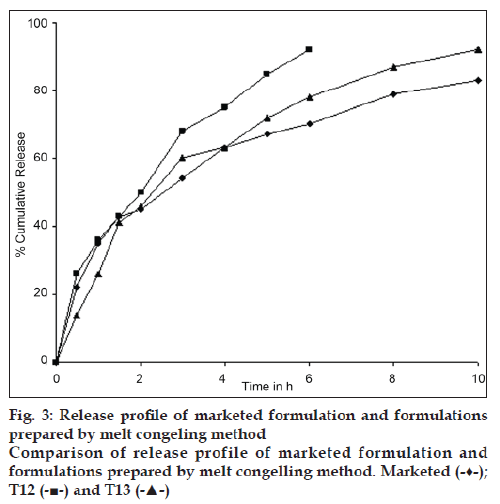
Formulations by direct compression, as shown in Table 1 and fig. 1, formulation T1 to T7 did not exhibit drug release as per desired specifications. So, wet granulation method, as shown in Table 2 and fig. 2, formulation T8 to T11 was tried in order to increase the cohesion and binding by formation of granules, using solution of polyvinyl alcohol in isopropyl alcohol as binder, DCP as diluent, and different polymers as release retardants. Wet granulation method did not give drug release as per set specifications. All the systems gave burst release. Therefore, the method used was melt congealing followed by wet granulation. In order to increase the hydrophobicity of the tablet various wax systems in combination with different polymers were used. Stearic acid and Methocel® K100M in different ratios were tried as release retardants (formulation T12 to T13). Batch T13 gave the desired release profile (fig. 3).
The results of the evaluation of tablets for appearance, tablet weight, diameter, thickness, hardness, friability is given in Table 3. The dissolution media used was 200 ml of pH 1.2 hydrochloric acid buffer for 2 h and phosphate buffer pH 7.2 for remaining 8 h. The basket type dissolution apparatus (Electrolab) was operated at 100 rpm; 37±0.5°. Formulations prepared using different combinations of polymers were tried and release was observed. Trimetazedine dihydrochloride tablets formulated by direct compression failed to give drug release as per desired specifications. The drug being highly water soluble and a hydrophilic material which allows quicker penetration of water in to the pores of the tablet system, resulted in faster drug release. Increase in cohesion and binding using PVA solution could not help in retardation of drug release. The probable reason of burst release could be insufficiency of hydrophobicity in the matrix. Hence, it was necessary to increase the hydrophobicity of the matrix.
| Parameter | Result |
|---|---|
| Appearance | Round, white, flat tablets with beveled edges |
| Tablet weight (mg) | 375±0.018 |
| Diameter (mm) | 11±0.044 |
| Thickness (mm) | 4.5±0.045 |
| Hardness (kg/cm2) | 4-5 |
| Friability(%) | 0.527 |
| Drug content (%) | 99.66±1.15 |
Table 3: Evaluation Of The Formulation
Melt congealling followed by wet granulation was thought to be a better process to increase the hydrophobicity of the matrix. Batch T12 although gave burst release it was quite close to the desired release profile. Further increase in the quantity of stearic acid and Methocel® K100M (batch T13) gave desired release profile. Increased quantity of stearic acid could coat the drug to a greater extent to give desired release profile.
Therefore, various wax systems in combination with different polymers were tried in order to increase the hydrophobicity of the system since the drug is highly water soluble. Thus tablets were formulated using Methocel® K100M, stearic acid, a wax system, dicalcium phosphate and other excipients by melt congealing method. Different ratios and combinations were tried to achieve a release of about 90% in 10 h.
Level of Methocel® K100M was varied from 120 mg to 180 mg and stearic acid from 90 mg to 150 mg. The amount of dihydrogen calcium phosphate was also varied from 2.5 mg to 3.75 mg. Formulation T13 having Methocel® K100M 180 mg and stearic acid 150 mg gave release according to set specifications and was compared with the marketed preparation. The tablet contains 48% of the polymer and 40% of stearic acid. The optimized formula concludes that not only high molecular weight polymer but also stearic acid wax system was required to obtain the tablet of our interest. The formulation, which gave release as per desired specifications, was subjected to stability studies.
The release exponent (n) indicates the release mechanism of the solute i.e. Fickian diffusion, anomalous non-Fickian diffusion, zero order time independent release and supercase II transport from the tablet. The diffusional release exponent (n) with their respective release mechanism and solute release rate is given in Table 4.
| Diffusional release exponent (n) |
Overall solute diffusion mechanism |
Time dependence of solute release rate (dMt/dt) |
|---|---|---|
| 0.5 | Fickian diffusion | t-0.5 |
| 0.5 < n < 1.0 | Anomalous (non-Fickian) diffusion | tn-1 |
| ######### | Case IItransport | Zero order time independent release |
| n > 1.0 | Super Case IItransport | tn-1 |
Table 4: Analysis of the diffusional release Mechanisms
The diffusional release exponent according to Korsmeyer Peppas Eqn. was found to be n = 0.6053, suggesting that the mechanism that leads to the diffusion of trimetazidine dihydrochloride from the sustained release tablets is anomalous (non-Fickian, drug diffusion in the hydrated matrix and polymer relaxation) diffusion [16-18].
The similarity factor f2 is the simple measure for the comparison of two dissolution profiles. It ensures the uniformity of product from batch to batch and help to predict bioavailability for formulation development. The similarity factor analysis between prepared tablets and marketed tablets showed the f2 factor (f2 = 66.81) greater than 50.
The f2 factor confirms that the formulated preparation T15 shows similar drug release as per marketed preparation. The results are summerized in Table 5. The developed product was found to be stable for 6 months under stability conditions.
| Time | % Cumulative release | f2 factor | |
|---|---|---|---|
| Reference | Test | ||
| 0.5 | 22 | 14 | 69.23 |
| 1 | 35 | 26 | 66.81 |
| 1.5 | 43 | 41 | 92.47 |
| 2 | 45 | 46 | 97.57 |
| 3 | 54 | 60 | 75.00 |
| 4 | 63 | 63 | 100.00 |
| 5 | 67 | 72 | 78.49 |
| 6 | 70 | 78 | 69.23 |
| 8 | 79 | 87 | 69.23 |
| 10 | 83 | 92 | 66.81 |
Table 5: F2 Factor Results
Twice daily ER tablets of trimetazidine dihydrochloride containing 30 mg of drug were successfully formulated by melt congealing followed by wet granulation method and have a uniform sustained action with increased patient compliance to overcome the drawbacks of multidosing. Tablets which were formulated using drug, stearic acid and Methocel® K100M in the ratio of 1:5:6 gave release as per set specifications. Optimized formulation was subjected to accelerated stability studies at room temperature 30°/65% RH at regular intervals for 6 months. The formulation was found stable with no change in all the parameters and in vitro release. HPTLC did not show presence of any degradation products.
Acknowledgements
Authors are grateful to the UGC for providing junior research fellowship.
References
- Steve IS, Bhaskara RJ, Xiaoling L, editors. Standard Handbook of Biomedical Engineering and Design. New York: McGraw-Hills; 2003.
- Gupta KV, Madhusudan H, Wheatley TA, Price JC. Controlled release tablets from carrageenans: Effect of formulation, storage and dissolution factors. Eur J Pharm Biopharm 2001;51:241-8.
- Tan HS, Wegman BM. Pharmaceutical Tablets. United States Patent No. 4711777;1987.
- Rama PY, Krishnaiah YS, Satyanarayana S. In vitro evaluation of guar gum as a carrier for colon specific drug delivery. J Control Release 1998;51:281-7.
- Streubel A, Siepmann J, Bodmeier R. Floating matrix tablets based on low density foam powder: Effects of formulation and processing parameters on drug release. Eur J Pharm Sci 2003;18:37-45.
- Peppas NA. Devices based on intelligent biopolymers for oral protein delivery. Int J Pharm 2004;277:11-7.
- Verma RK, Mishra B, Garg S. Osmotically controlled oral drug delivery. Drug Develop Ind Pharm 2000;26:695-708.
- Appel LE, Ray RJ, Newbold DD, Lyon DK. Azithromycin multiparticulate dosage forms by melt coneal processes. United States Patent Application No. 20050158391;2005.
- Nalbentgil S, Altintig A, Yilmaz H, Onder R. The effect of trimetazidine in the treatment of microvascular angina. Int J Angiol 2005;6:40-3.
- Hardman G, Limbird LE, Goodman AG, editors. Goodman and Gilman’s The Pharmacological Basis of Therapeutics. New York: McGraw-Hill; 2001.
- Naito SI, Osumi S, Hirose M. Trimetazidine in blood, bile, organs and urine. Chem Pharm Bull 1972;20:682-8.
- Thoppil SO, Cardoza RM, Amin PD. Stability indicating HPTLC determination of trimetazidine as bulk drug and in pharmaceutical formulations. J Pharm Biomed Anal 2001;25:15-20.
- Korsmeyer RW, Gurny R, Doelker EM, Buri P, Peppas NA. Mechanism of solute release from porous hydrophilic polymers. Int J Pharm 1983;15:25-35.
- Shah VP, Tsong Y, Sathe P, Liu JP. In vitro dissolution profile comparison-statistics and analysis of the similarity factor, f2. Pharm Res 1998;15:889-96.
- Cartensen JT, Rhodes CT, editors. Drug Stability- Principles and Practice. New York: Marcel Dekker Inc.; 2000.
- Ritger PL, Peppas NA. A simple equation for description of solute release I. Fickian and non-fickian release from non-swellable devices in the form of slabs, spheres, cylinder or discs. J Control Release 1987;5:23-36.
- Korsmeyer RW, Peppas NA. Effect of the morphology of hydrophilic polymeric matrices on the diffusion and release of water soluble drugs. J Membr Sci 1981;9:211-27.
- Peppas NA. Analysis of fickian and non-fickian drug release from polymer. Pharm Acta Helv 1985;60:110-1.