- *Corresponding Author:
- Xinglong Zhang
WuXi XiShan District Hospital of Traditional Chinese Medicine, Wuxi , Jiangsu Province 214196, China
E-mail: 15962724726@126.com
| This article was originally published in a special issue,“Emerging Therapeutic Interventions of Biopharmaceutical Sciences” |
| Indian J Pharm Sci 2024:86(3) Spl Issue “268-273” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
This study assessed the efficacy and safety of edaravone dexborneol in conjunction with aspirin in managing acute ischemic stroke. A retrospective study was conducted with 128 individuals who were treated for ischemic stroke from February 2019 to June 2023. Based on varying treatment methods, the individuals were categorized into control (n=62) and observation groups (n=66). In the observation group, a combination therapy of edaravone dexborneol and aspirin was administered, while the control group was provided with enteric-coated aspirin. Comparative analysis of the two groups included clinical efficacy, neurological function using National Institutes of Health Stroke Scale, daily living activities, hemorheology parameters (whole blood high shear viscosity, whole blood low shear viscosity and plasma viscosity), serum oxidative stress levels (superoxide dismutase and malondialdehyde), and levels of neuroinjury biomarkers (neuron-specific enolase, specific calcium-binding protein 100-beta. The study also evaluated adverse reactions between the two groups. Significantly higher effectiveness of treatment was observed in the observation group (92.42 %) and control group (72.58 %) (p<0.05). While following the treatment, observation group exhibited a more notable declined in National Institutes of Health Stroke Scale scores and an elevation in activities of daily living scores when compared with the control group (p<0.05). Similarly, the observation group exhibited a notable decline in hemorheology parameters (including whole blood high shear viscosity, whole blood low shear viscosity, and plasma viscosity) when compared to the control group (p<0.05). The observation group displayed a notable decline in serum oxidative stress levels (malondialdehyde) and a considerable elevation in superoxide dismutase levels, compared to the control group (p<0.05). Furthermore, the observation group exhibited a remarkable decline in the levels of neuroinjury biomarkers compared to the control group (p<0.05). Adverse reaction incidence rates of 10.61 % and 9.68 % were observed in the observation group and control group, respectively (p>0.05). In the treatment of acute ischemic stroke, the utilization of edaravone dexborneol in combination with aspirin exhibits positive clinical efficacy and safety.
Keywords
Edaravone dexborneol, aspirin, acute ischemic stroke, efficacy, safety evaluation, neuroprotective effect
The symptoms of Acute Ischemic Stroke (AIS) often include limb numbness, speech impairment, limb dysfunction and in severe cases, may progress to hemiplegia. AIS necessitates immediate hospitalization for treatment due to its abrupt onset. Any delay in treatment could lead to brain tissue damage and compromised neurological function, considerably affecting patients' general well-being and daily functioning[1-3].
In the field of clinical practice, intravenous thrombolysis and endovascular intervention currently serve as the main treatment methods for AIS, both striving to re-establish cerebral blood flow and mitigate neurological harm. Nevertheless, some patients still face a poor prognosis[4,5]. Research in recent years has revealed that employing neuroprotective drugs can diminish brain tissue damage and suppress neuronal apoptosis, leading to improved patient results. In July 2020, the Chinese National Medical Products Administration (China NMPA) approved the use of edaravone in conjunction with dexborneol, an injectable concentrated solution, as a class 1 drug. In a proportion of 4:1, edaravone and dexborneol together create a synergistic effect by scavenging free radicals and reducing inflammation. Its key function in clinical usage is to alleviate neurological symptoms associated with AIS[6-9]. However, aspirin is a widely utilized antiplatelet drug that proficiently hinders platelet aggregation and release, consequently facilitating vasodilation and fostering improved blood circulation in the body[10,11]. The different mechanisms of anti-thrombotic action exhibited by Edaravone Dexborneol (Eda.B) and aspirin may result in a synergistic effect, potentially enhancing the therapeutic efficacy for AIS.
As a result, this study seeks to figure out the efficacy and safety of Eda.B in conjunction with aspirin in managing AIS patients, providing crucial scientific validation for further advancements in clinical practice in this area.
Materials and Methods
Molecular docking:
The study population consisted of 128 individuals who received treatment for ischemic stroke at our hospital from February 2019 to June 2023 and were subsequently categorized into two groups based on different treatment approaches. The control group (n=62) was provided with enteric-coated aspirin, while the observation group (n=66) was given a combination of Eda.B and aspirin, with both groups receiving standard treatment. Observation group comprised 30 male and 32 female individuals, aged (44-79) y with a mean age of (57.73±3.88) y. Similarly, the control group consisted of 34 female and 32 male individuals, aged (45-79) y with a mean age of (58.04±4.24) y. Baseline characteristics did not exhibit any remarkable differences between the two groups (p>0.05). This research received approval from the Ethics Committee of our institution.
Inclusion criteria:
Patients meeting the relevant diagnostic criteria and confirmed diagnosis of AIS[12]; disease onset within 72 h; patients with signed informed consent forms were included in this study.
Exclusion criteria:
Patients with concomitant systemic infection and other central nervous system diseases; patients who were allergic to the drugs used in this study; having a history of drug allergies; psychological disorders and severe organ diseases such as heart, liver, and kidney were excluded from the study.
Treatment methods:
Standard treatment, such as risk factor management, lipid-lowering and neuro-nutritional intervention, and circulatory enhancement, was administered to both groups. The patients' vital signs and blood pressure were monitored, and medications for treating arterial circulation issues were not administered during this time. Alongside standard care, the control group was prescribed enteric-coated aspirin (Bayer HealthCare Co., Ltd., National Drug Approval Number: HJ20160685) at a daily dose of 100 mg for a continuous treatment period of 14 d. The observation group received both aspirin and Eda.B (an injectable concentrated solution produced by Xian Voice Pharmaceutical Co., Ltd., National Drug Approval Number: H20200007), with aspirin dosage the same as that of the control group and Eda.B being mixed uniformly with 0.9 % sodium chloride solution at a volume of 100 ml and administered intravenously twice a day continuously for 2 w.
Observational parameters:
Clinical efficacy: It was evaluated using the following parameters, markedly effective, effective and ineffective. National Institutes of Health Stroke Scale (NIHSS) score reduction of 46 %-90 % with restored ability for self-care was considered to be markedly effective; NIHSS score reduction of 18 %-45 % with partial symptom disappearance was considered as effective and failure to achieve symptom improvement or worsening was considered to be ineffective. The sum of the marked effective rate and the effective rate determines the overall effective rate. NIHSS was utilized to assess neurological function, where a higher score represents more profound neurological impairment. Scores prior to and following treatment were compared using a scale to evaluate Activities of Daily Living (ADL), with a higher score signifying improved daily life functioning.
Hemorheological parameters: A hemorheological analyzer (Beijing Zhongchi Co., Ltd.,) was utilized to measure hemorheological parameters, including Whole Blood High Shear Viscosity (WBHSV) by collecting 3 ml of fasting venous blood prior to and following treatment. Levels of Malondialdehyde (MDA) and Superoxide Dismutase (SOD) were evaluated by examining the serum from fasting venous blood prior to and following treatment, using light scatter immunoturbidimetry for comparison.
Using Enzyme-Linked Immunosorbent Assay (ELISA), the levels of Neuron-Specific Enolase (NSE) and Specific protein 100-Beta (S-100 β), neuroinjury biomarkers, were measured both before and after treatment to compare the levels between the two groups. Adverse reactions were recorded during the treatment period.
Statistical analysis:
The analysis compared the measurement data between the two groups utilizing the Statistical Package for the Social Sciences (SPSS) 25.0 software, presented as mean±standard deviation, and employed the Chisquare (χ2) test for analyzing the count data, with statistical significance defined at p<0.05.
Results and Discussion
Significant importance was noted due to the total effective rate in the observation group being considerably higher, at 92.42 %, compared to the control group at 72.58 % (Table 1).
| Group | n | Markedly effective | Effective | Ineffective | Total effective rate |
|---|---|---|---|---|---|
| Observation | 66 | 27 (40.91) | 34 (51.52) | 5 (7.58) | 61 (92.42) |
| Control | 62 | 20 (32.26) | 25 (40.32) | 17 (27.42) | 45 (72.58) |
| χ2 | 8.844 | ||||
| p | 0.003 |
Table 1: Curative Effect
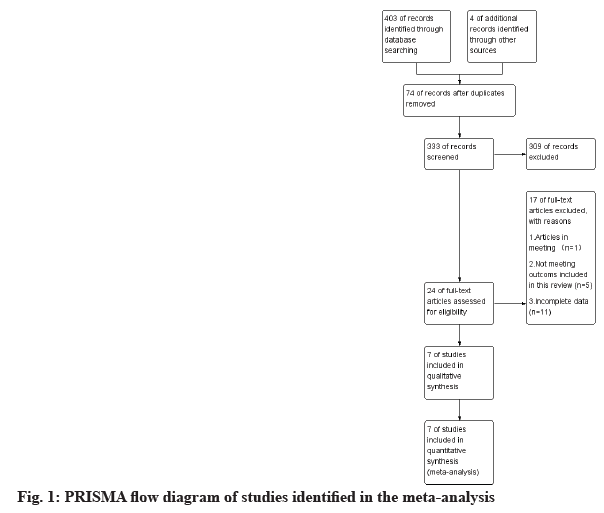
Prior to treatment, no remarkable difference was identified between the two groups in the comparison of NIHSS and ADL scores (p>0.05). Subsequent to treatment, there was a substantial decrease in NIHSS scores and an increase in ADL scores, particularly in the observation group, showing substantial significance as opposed to the control group (p<0.05) (fig. 1).
Prior to treatment, the comparison of Whole Blood High Shear Viscosity (WBHSV), Whole Blood Low Shear Viscosity (WBLSV), and Plasma Viscosity (PV) levels between groups did not reveal any remarkable significance (p>0.05). Following treatment, the levels of WBHSV, WBLSV, and PV all declined, with the observation group exhibiting lower levels, and the variances were notably significant (p<0.05) (Table 2).
| Group | n | WBHSV | WBLSV | PV | |||
|---|---|---|---|---|---|---|---|
| Before | After | Before | After | Before | After | ||
| Observation | 66 | 17.78±3.75 | 6.53±2.04* | 30.12±4.65 | 13.69±3.77* | 1.85±0.37 | 1.68±0.23* |
| Control | 62 | 17.95±3.72 | 8.86±2.64* | 29.78±4.74 | 16.66±3.84* | 1.92±0.35 | 1.45±0.22* |
| t | -0.823 | 4.82 | 0.882 | 5.124 | 0.151 | -5.049 | |
| p | 0.412 | 0 | 0.38 | 0 | 0.88 | 0 | |
Note: (*) indicates noteworthy difference following treatment compared with prior to treatment
Table 2: Hemorheological Level (Mpas-1)
There were no noteworthy differences in the levels of MDA and SOD between the two groups (p>0.05). Subsequently the average levels of MDA decreased, with the observation group showing remarkably lower levels, and the average levels of SOD increased, with the observation group showing higher levels (p<0.05) (Table 3).
| Group | n | MDA (mmol/l) | SOD (U/ml) | ||
|---|---|---|---|---|---|
| Before | After | Before | After | ||
| Observation | 66 | 5.76±1.47 | 3.23±0.87* | 58.46±7.78 | 97.46±10.74* |
| Control | 62 | 5.83±1.45 | 4.47±1.25* | 57.87±7.86 | 85.24±9.45* |
| t | -0.817 | 6.498 | -1.548 | -7.367 | |
| p | 0.415 | 0 | 0.124 | 0 | |
Note: (*) indicates noteworthy difference following treatment compared with prior to treatment
Table 3: Oxidative Stress Reaction
Neurological function markers were studied. There were no notable differences in the levels of NSE and Specific calcium-binding protein 100 Beta (S-100 β) between the two groups (p>0.05). The observation group showed lower levels of the two markers following treatment (p<0.05) (Table 4).
| Group | n | NSE (ng/ml) | S-100 β (ng/l) | ||
|---|---|---|---|---|---|
| Before | After | Before | After | ||
| Observation | 66 | 35.27±4.87 | 13.83±2.58* | 305.72±44.78 | 146.82±30.47* |
| Control | 62 | 34.93±4.94 | 16.32±2.81* | 307.41±46.82 | 203.75±34.93* |
| t | -0.783 | 4.598 | 0.229 | 9.392 | |
| p | 0.435 | 0 | 0.819 | 0 | |
Note: (*) indicates noteworthy difference following treatment compared with prior to treatment
Table 4: NSE and S-100 Β
No remarkable difference was identified between the two groups in the incidence rate of adverse reactions during treatment, with the observation group at 10.61 % and the control group at 9.68 % (p>0.05) (Table 5).
| Group | n | Hypotension | Rash | Palpitation | Nausea | Overall incidence |
|---|---|---|---|---|---|---|
| Observation | 66 | 1 (1.52) | 3 (4.55) | 1 (1.52) | 2 (3.03) | 7 (10.61) |
| Control | 62 | 2 (3.23) | 1 (1.61) | 2 (3.23) | 1 (1.61) | 6 (9.68) |
| χ2 | 0.03 | |||||
| p | 0.862 |
Table 5: Adverse Reactions (N%)
Patients suffering from ischemic stroke often encounter high disability and mortality rates due to its widespread impact as a cerebrovascular disease. Common chronic conditions such as hypertension and hyperlipidemia predispose individuals to the development of cerebral thrombosis, resulting in sustained cerebral ischemia and damage to local brain tissue or the overall brain function[13]. Promoting the restoration of blood supply to ischemic brain tissue, reopening obstructed blood vessels, and encouraging the recovery of neurological function are crucial in the clinical management of ischemic stroke[14].
As a frequently prescribed antiplatelet medication, aspirin significantly suppresses the activity of acetylated Cyclooxygenase 1 (COX-1), proficiently preventing platelet aggregation and release. Dilating blood vessels and releasing hydrogen ions, it can damage cell membrane proteins, thus preventing plaque detachment within blood vessels and reducing platelet aggregation. Nevertheless, aspirin's lack of effectiveness in inhibiting activated platelets means it is insufficient for promptly controlling the patient’s condition during treatment, requiring combination with other medications for effective management[15]; Eda.B is a multi-target neuroprotective agent. Edaravone scavenges free radicals, while dexborneol holds a notable anti-inflammatory effect[16]. The scientific proportion of edaravone and dexborneol in Eda.B was screened and determined, rendering its effectiveness in providing neuroprotection when used in clinical practice[17,18].
The observation group, employing a combination of Eda.B and aspirin for AIS patients, demonstrated a notably higher effective rate compared to the control group, treated with aspirin alone. This indicates that the combination of Eda.B and aspirin demonstrates good efficacy in treating AIS. Significantly, after treatment the observation group exhibited notable improvement in the NIHSS and ADL scores compared to the control group, implying the capacity of the combination therapy to enhance the recovery of neurological function and daily living capacity in patients. Furthermore, the observation group exhibited decreased levels of WBHSV, WBLSV and PV after treatment, all of which were remarkably lower than the control group. This implies that the combination therapy has the potential to enhance blood rheological properties, thereby promoting the restoration of cerebral blood flow. Observation group's post-treatment showed a marked reduction in MDA levels and a notable elevation in SOD levels when compared with the control group, suggesting the potential of the combination therapy in reducing oxidative stress levels and minimizing neural cell damage. Similarly, the observation group experienced a significant decrease in NSE and S-100 β levels, signifying a reduction in the levels of these markers that play a crucial role in assessing neural cell damage[19]. These results further confirm that the combination therapy can reduce neural cell damage. Regarding adverse reactions, no remarkable difference was identified between the two groups in the incidence rate during treatment, with the observation group at 10.61 % and the control group at 9.68 % (p>0.05).
The study's retrospective design is one of its limitations, which may introduce some information bias. Additionally, because of the relatively small sample size, larger randomized controlled studies are required for further validation of these results. Moreover, the analysis did not include the treatment time window, which can have an impact on future clinical decisions.
In summary, the combination of Eda.B and aspirin exhibits substantial clinical efficacy for AIS. It improves patients' neurological function, daily living capacity, hemorheological parameters, reduces oxidative stress and minimizes neural cell damage which suggests that the combination therapy can provide an effective and safe treatment strategy. The results offer a new therapeutic option for patients with AIS.
Conflict of interests:
The authors declared no conflict of interests.
References
- Feske SK. Ischemic stroke. Am J Med 2021;134(12):1457-64.
[Crossref] [Google Scholar] [PubMed]
- Jolugbo P, Ariens RA. Thrombus composition and efficacy of thrombolysis and thrombectomy in acute ischemic stroke. Stroke 2021;52(3):1131-42.
[Crossref] [Google Scholar] [PubMed]
- Walter K. What is acute ischemic stroke? JAMA 2022;327(9):885.
[Crossref] [Google Scholar] [PubMed]
- Mendelson SJ, Prabhakaran S. Diagnosis and management of transient ischemic attack and acute ischemic stroke: A review. JAMA 2021;325(11):1088-98.
[Crossref] [Google Scholar] [PubMed]
- Rabinstein AA. Update on treatment of acute ischemic stroke. Continuum 2020;26 (2):268-86.
[Crossref] [Google Scholar] [PubMed]
- Huang Y, Zhang X, Zhang C, Xu W, Li W, Feng Z, et al. Edaravone dexborneol downregulates neutrophil extracellular trap expression and ameliorates blood-brain barrier permeability in acute ischemic stroke. Mediators Inflamm 2022:1-11.
[Crossref] [Google Scholar] [PubMed]
- Xu J, Wang A, Meng X, Yalkun G, Xu A, Gao Z, et al. Edaravone dexborneol vs. edaravone alone for the treatment of acute ischemic stroke: A phase III, randomized, double-blind, comparative trial. Stroke 2021;52(3):772-80.
[Crossref] [Google Scholar] [PubMed]
- Zhang H, Wang L, Zhu B, Yang Y, Cai C, Wang X, et al. A comparative study of the neuroprotective effects of dl-3-n-butylphthalide and edaravone dexborneol on cerebral ischemic stroke rats. Eur J Pharmacol 2023;951:175801.
[Crossref] [Google Scholar] [PubMed]
- Xi Y, Ma J, Lu S. Favorable neuroprotective effect of intra-arterial application of edaravone dexborneol in ischemic stroke rats. J Stroke Cerebrovasc Dis 2023;32(11):107356.
[Crossref] [Google Scholar] [PubMed]
- Lin SF, Hu HH, Ho BL, Chen CH, Chan L, Lin HJ, et al. Pre-treatment of single and double antiplatelet and anticoagulant with intravenous thrombolysis for older adults with acute ischemic stroke: The TTT-AIS experience. Front Neurol 2021;12:1-8.
[Crossref] [Google Scholar] [PubMed]
- McDonald MM, Almaghrabi TS, Saenz DM, Cai C, Rahbar MH, Choi HA, et al. Dual antiplatelet therapy is associated with coagulopathy detectable by thrombelastography in acute stroke. J Intensive Care Med 2020;35(1):68-73.
[Crossref] [Google Scholar] [PubMed]
- Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. 2018 guidelines for the early management of patients with acute ischemic stroke: A guideline for healthcare professionals from the American heart association/American stroke association. Stroke 2018;49(3):e46-110.
[Crossref] [Google Scholar] [PubMed]
- Zhao J, Chen F, Lu L, Tang H, Yang R, Wang Y, et al. Effect of 106PEAR1 and 168PTGS1 genetic polymorphisms on recurrent ischemic stroke in Chinese patient. Medicine 2019;98(29):e16457.
[Crossref] [Google Scholar] [PubMed]
- Hurford R, Sekhar A, Hughes TA, Muir KW. Diagnosis and management of acute ischaemic stroke. Pract Neurol 2020;20(4):304-16.
[Crossref] [Google Scholar] [PubMed]
- Kamarova M, Baig S, Patel H, Monks K, Wasay M, Ali A, et al. Antiplatelet use in ischemic stroke. Ann Pharmacother 2022;56(10):1159-73.
[Crossref] [Google Scholar] [PubMed]
- Kikuchi K, Tancharoen S, Takeshige N, Yoshitomi M, Morioka M, Murai Y, et al. The efficacy of edaravone (radicut), a free radical scavenger, for cardiovascular disease. Int J Mol Sci 2013;14(7):13909-30.
[Crossref] [Google Scholar] [PubMed]
- Cao Y, Yue X, Jia M, Wang J. Neuroinflammation and anti-inflammatory therapy for ischemic stroke. Heliyon 2023;9(7):e17986.
[Crossref] [Google Scholar] [PubMed]
- Xu J, Wang Y, Wang A, Gao Z, Gao X, Chen H, et al. Safety and efficacy of edaravone dexborneol vs. edaravone for patients with acute ischaemic stroke: A phase II, multicentre, randomised, double-blind, multiple-dose, active-controlled clinical trial. Stroke Vasc Neurol 2019;4(3):109-14.
[Crossref] [Google Scholar] [PubMed]
- Onatsu J, Vanninen R, Jakala P, Mustonen P, Pulkki K, Korhonen M, et al. Tau, S100B and NSE as blood biomarkers in acute cerebrovascular events. In Vivo 2020;34(5):2577-86.
[Crossref] [Google Scholar] [PubMed]