- *Corresponding Author:
- Hongqiang Zhang
Department of Neurosurgery, The Second Hospital of Dalian Medical University, Liaoning 116023, China
E-mail: zhq20240122@126.com
| This article was originally published in a special issue, “Emerging Therapeutic Interventions of Biopharmaceutical Sciences” |
| Indian J Pharm Sci 2024:86(3) Spl Issue “274-279” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
To evaluate the clinical efficacy of Beifuxin in the management of surgical difficult-to-heal wounds. Our hospital enrolled 122 patients challenging with wound healing between June 2022 and June 2023, categorizing them randomly into a trial group and a control group. Treatment with Beifuxin was provided to the observation group, while the control group was managed with traditional wound dressing approaches. Comparative analysis was conducted between the two groups regarding clinical effectiveness, recovery duration, granulation tissue appearance, skin quality restoration, recurrence frequency and infection rate. The observation group displayed a notably higher total clinical effectiveness rate of 93.33 % in contrast to the 73.33 % rate in the control group, coupled with quicker wound healing and earlier onset of granulation tissue. Compared with the control group, the observation group displayed healed wounds with color, tension and hardness approaching that of normal skin, alongside lower rates of recurrence and wound infection. In managing difficult-to-heal wounds, Beifuxin has exhibited substantial clinical efficacy, fostering advanced wound healing, encouraging granulation tissue formation and enhancing the overall wound healing quality. Beifuxin exhibits potential for promising clinical applications and merits further comprehensive research and implementation.
Keywords
Beifuxin, recombinant bovine basic fibroblast growth factor, difficult-to-heal wounds, efficacy
Prolonged wounds that are difficult to heal are defined by their inability to heal as expected due to factors related to the injury site and the host[1,2]. Such wounds are often observed in scenarios involving traumatic ulcers, radiation ulcers, infected wounds, necrotic wounds and in individuals with chronic malnutrition and diabetes[3,4]. These wounds frequently lead to enduring pain, infection, limited functionality and reduced quality of life for patients[5]. Managing difficultto- heal wounds presents a significant challenge for both patients and healthcare providers[6,7].
Presently, addressing difficult-to-heal wounds encompasses a range of methods including wound debridement, antibiotic application, physical therapy, stem cell therapy and tissue-engineered materials[5,8-10]. Nevertheless, existing treatment approaches frequently do not adequately address the specific requirements of individual patients due to varied causes and clinical profiles. Consequently, the medical field has placed a strong emphasis on identifying an efficient treatment strategy to expedite the healing of difficult wounds.
Beifuxin (recombinant bovine basic fibroblast growth factor gel) is a holistic remedy employed in the management of challenging wound healing. Its chief constituent is recombinant bovine basic fibroblast growth factor, recognized for its potential to foster wound repair and healing[11]. Notwithstanding the extensive utilization of Beifuxin in clinical settings, there is ongoing controversy surrounding its effectiveness and operating mechanisms in treating challenging wounds. Hence, the purpose of this study is to appraise the clinical efficacy of Beifuxin in addressing difficultto- heal wound healing through clinical observation and to explore its potential mechanism of action.
Materials and Methods
General information:
A total of 122 patients with difficult-to-heal wounds admitted to our hospital from June 2022 to June 2023 were included in the study, of which 37 cases underwent perianal abscess drainage, 23 cases underwent excision of coccygeal nodules, 18 cases underwent mastectomy, 14 cases underwent sacrococcygeal cyst excision, 12 cases underwent rectal cancer resection, 10 cases underwent internal fixation for tibial fractures and 8 cases underwent hysterectomy. The range of skin defect area was 2-9 cm2. This study was approved by the hospital’s Ethics Committee and patients and their families voluntarily participated in this study, signing informed consent forms.
Inclusion criteria includes patients in the study were postoperative with difficult-to-heal wounds, where the postoperative wounds had exceeded the normal healing time and required external force to promote healing; patients and their families were willing to cooperate and signed informed consent forms. Exclusion criteria includes patients with chronic conditions such as diabetes and nerve damage; coagulation function disorders; long-term use of steroids or other factors affecting skin healing; patients with significant abnormalities in blood tests.
Methods:
Wound management: Difficult-to-heal wounds, due to their long duration and frequent infections, often involve non-fresh tissue, cessation of granulation tissue growth, and severe tissue contamination. Therefore, early mechanical debridement of necrotic tissues is necessary for such wounds, and debridement can be performed multiple times when necessary to avoid excessive bleeding. For wounds with severe infection, samples should be cultured first and appropriate antibiotic treatment given based on the culture and sensitivity results to control the infection. Utilization of polyvinylpyrrolidone iodine solution from Guangdong Hengjian Pharmaceutical Co., Ltd., (national drug approval number H44023924) was adopted for disinfecting the skin surrounding the wound and in cases featuring severe contamination, hydrogen peroxide from Guangdong Hengjian Pharmaceutical Co., Ltd., (H44023919) was employed to remove the contamination, with subsequent wound cleansing using normal saline. Various treatment protocols were applied tailored to the specific characteristics of each wound group once the wounds had dried.
Medication methods:
Control group medication: Dry iodophor gauze was applied to pack or cover the wound after cleaning ensuring an appropriate tightness without any gaps, followed by the administration of sterile dressings. Waterproof dressings were used for patients with significant exudation to prevent external exudate contamination. Dressings were changed every 4-6 h, based on the actual condition of the wound.
Observation group medication: Varying medication techniques were utilized based on the depth of the wound. For deeper wounds, Beifuxin (Zhuhai Yisheng Biopharma Co., Ltd., national drug approval number S20040001) gauze was directly packed into the wound without any gaps following wound cleaning, and sterile dressings were applied. Waterproof dressings were also used for patients with substantial exudation to prevent contamination. In instances of deep sinuses in wounds, Beifuxin was administered via injection using a scalp needle extension tube. For superficial wounds, the application of Beifuxin at a dosage of 300 IU/cm2 or the use of Beifuxin gauze for covering was followed by external wrapping with sterile dressing. The dressings were replaced every 4-6 h to correspond with the specific condition of the wound, and patients were monitored for 6 mo to assess the progress of wound healing.
Efficacy evaluation:
Clinical efficacy criteria: Complete formation of new granulation tissue on the wound, complete wound healing and the wound skin color is similar to normal skin; new granulation tissue growth on the wound with a healing rate of no less than 80 % noted as marked improvement; clean wound with minimal exudate, new granulation tissue in the wound, reduction in wound size, but with a healing rate of less than 80 % noted as improvement; after dressing, no new granulation tissue is observed, the wound still secretes, or the wound worsens noted as ineffectiveness.
Total effective rate=(sured+marked improvement+improvement)/Total cases×100 %.
Skin healing quality: Individuals were treated until the wound attained cleanliness, dryness and absence of exudate. Afterward, the color, hardness and tension of the wound skin were scrutinized and compared to normal skin, yielding a total score of 5. The wound skin exhibited qualities comparable to normal skin, with a moderate hardness and tension similar to normal skin, warranting a score of 5. In most areas, the wound skin closely resembled normal skin, with slight dark red pigmentation, slightly greater hardness than normal skin, and marginally reduced tension compared to normal skin, resulting in a score of 4. About half of the wound skin had a dark red appearance, relatively elevated hardness in the new skin, reduced tension compared to normal skin and nearly half of the wound demonstrating scarring, resulting in a score of 3. Most of the wound skin displayed a dark red color, relatively high new skin hardness and relatively low tension, with a likelihood of rupture, securing a score of 2. The wound skin demonstrated a dark red hue, scar-like characteristics, hardness, lack of tension in the new skin, and susceptibility to rupture, achieving a score of 1.
Observation indicators:
Following the treatment, the clinical effectiveness, duration of wound healing, appearance time of granulation tissue, quality of wound skin (color, hardness and tension), recurrence rate and infection rate within both groups were monitored.
Statistical methods:
Utilizing the Statistical Package for Social Sciences 25.0, the analysis was performed, comparing the measurement data, presented as mean±standard deviation, between the two groups via an independent sample t-test. Utilizing the chi-square test, the count data were analyzed. The criteria for establishing statistical significance were defined at a level of p<0.05.
Results and Discussion
Divided into the observation group (n=62) and the control group (n=60), the patients in the observation group comprised 36 males and 26 females, aged 18- 65, with an average age of (37.35±6.41) y, and a skin injury area of (4.53±0.75) cm2. The control group consisted of 37 males and 23 females, aged between 17 and 65, with an average age of (37.62±6.32) y, and a skin injury area of (4.32±0.72) cm2. No statistically significant discrepancies in general data, such as gender, age, and skin injury, were detected between the two groups (p>0.05), indicating their comparability (Table 1).
| Group (n) | Observation (62) | Control (60) | t/χ2 | p |
|---|---|---|---|---|
| Age | 37.35±6.41 | 36.12±6.94 | -1.025 | 0.308 |
| Sex | ||||
| Male | 36 | 37 | 0.165 | 0.685 |
| Female | 26 | 23 | ||
| Area of skin injury | 4.53±0.75 | 4.31±0.79 | -1.577 | 0.117 |
Table 1: General Information
The total clinical effective rates for the two groups were 93.33 % and 73.33 % correspondingly, with the observation group exhibiting a substantially higher total effective rate than the control group (p<0.05) (Table 2).
| Group (n) | Cured | Marked improvement | Improvement | Ineffectiveness | Total effective rate |
|---|---|---|---|---|---|
| Observation (62) | 34(54.84) | 14(22.58) | 9(14.52) | 5(8.06) | 57(91.94) |
| Control (60) | 16(26.67) | 12(20.00) | 15(25.00) | 17(28.33) | 43(71.67) |
| χ2 | 8.475 | ||||
| p | 0.004 |
Table 2: Curative Effect
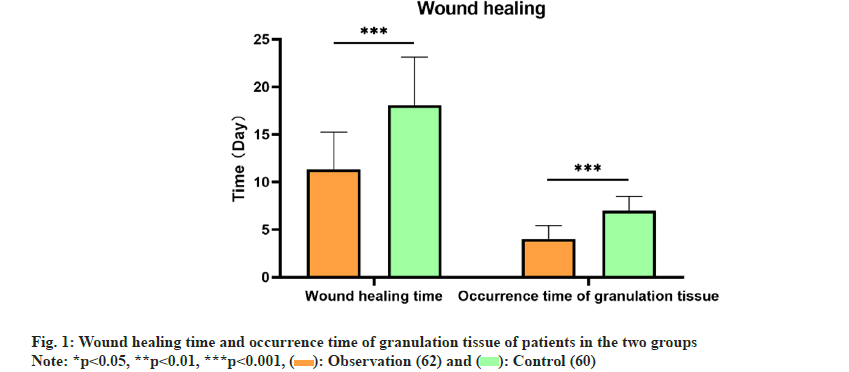
Post-treatment, the observation group exhibited a swifter wound healing period and earlier appearance of granulation tissue in comparison to the control group, with substantial disparities (p<0.05) (fig. 1).
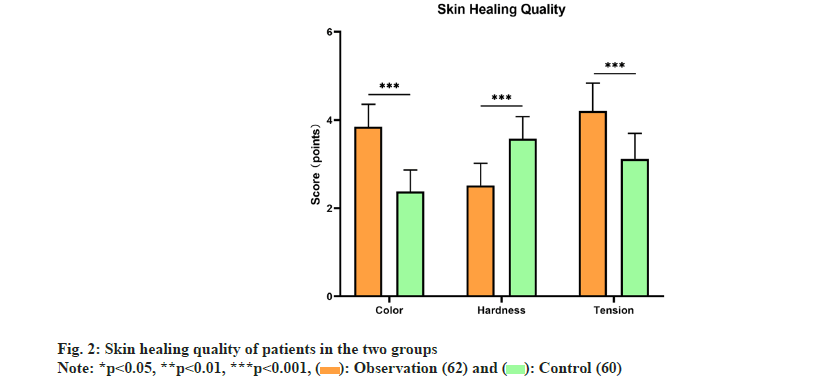
Following treatment, the color of the healed wounds in the observation group closely resembled normal skin color in contrast to the control group, and the tension and hardness of the healed skin were superior to those in the control group, with remarkable distinctions (p<0.05) (fig. 2).
Following treatment, the observation group exhibited a reduced recurrence rate and wound infection rate in comparison to the control group, with notable variations (p<0.05) (Table 3).
| Group (n) | Recurrence | Wound infection |
|---|---|---|
| Observation (62) | 6(9.68) | 4(6.45) |
| Control (60) | 17(28.33) | 15(25.00) |
| χ2 | 6.937 | 7.979 |
| p | 0.008 | 0.005 |
Table 3: Recurrence and Wound Infection Rate
Wound recovery constitutes a complex biological process, presenting a notable challenge in the treatment of difficult-to-heal wounds[12].
Recently, conventional wound dressing and surgical repair techniques have emerged as widespread therapies for challenging wound recoveries[13,14]. Nonetheless, traditional wound dressing techniques offer limited support in the process of wound recovery, primarily encompassing the packing or covering of wounds to prevent infection. At the same time, surgical repair methods pose certain risks, restricting their clinical utility. The literature has indicated that wound healing encompasses a set of complex biological processes, which include cell proliferation, migration, deposition of the extracellular matrix, angiogenesis, tissue remodeling and all of which are regulated and facilitated by molecular mechanisms[15-17]. The ideal treatment for difficult-to-heal wounds is a goal currently pursued by researchers.
Beifuxin, a gel containing recombinant bovine basic fibroblast growth factor, is typically applied at a dosage of approximately 300 IU/cm2, directly onto the wound and then covered with a suitablysized sterilized dressing. Research has indicated that recombinant bovine basic Fibroblast Growth Factor (rb-bFGF) promotes the repair and regeneration of cells originating from the mesoderm layer, such as epithelial cells, dermal cells, fibroblasts and vascular endothelial cells[18,19]. Research in pharmacology indicates that bFGF has the capacity to boost cell proliferation, differentiation and enhance local blood circulation, leading to the acceleration of wound healing. Consequently, it can be utilized for fresh wounds (such as trauma, skin graft donor site wounds, surgical wounds), burn wounds (generally shallow and deep second-degree burns, granulation wounds) and chronic wounds (like diabetic ulcers, different skin ulcers)[11,20].
The objective of this study was to assess the clinical effectiveness of Beifuxin in addressing challenging wound recoveries. Due to the frequent occurrence of issues such as infection and tissue necrosis in difficult-to-heal wounds, mechanical debridement of necrotic tissue is a vital component of treatment and should be performed incrementally as required to mitigate excessive bleeding. In instances of severe infection, it is imperative to perform initial culturing and initiate suitable antimicrobial treatment to effectively manage the infection.
As documented in this study, the observation group exhibited a total clinical effective rate of 93.33 %, significantly outperforming the 73.33 % in the control group. In addition, subsequent to treatment, the observation group exhibited accelerated wound healing time and earlier appearance of granulation tissue in comparison to the control group. Additionally, the wound color, tension and hardness in the observation group were more skin to normal skin compared to the control group. The observation group also exhibited a reduced recurrence rate and incidence of wound infection.
In summary, Beifuxin has displayed remarkable clinical efficacy in managing difficult-to-heal wounds. Additionally, the observation group revealed better outcomes across total clinical efficacy, wound healing duration, granulation tissue appearance, skin healing quality, recurrence rate and wound infection rate compared to the control group. It is indicative that Beifuxin may hasten wound recovery, stimulate granulation tissue formation, and enhance the quality of wound healing. However, it is important to note that this study has limitations, such as a relatively brief observation period and a small sample size, underscoring the necessity for additional research to verify these findings. On the whole, Beifuxin presents potential for clinical utilization in treating difficult-to-heal wounds, and justifies the need for additional in-depth research.
Conflict of interests:
The authors declared no conflict of interests.
References
- Wang P, Yin B, Su YJ, Jia CY. Research advances in healing mechanism of chronic refractory wounds mediated by long non-coding RNA. Zhonghua Shao Shang Za Zhi 2020;36(8):758-61.
[Crossref] [Google Scholar] [PubMed]
- Wang J, Wu H, Peng Y, Zhao Y, Qin Y, Zhang Y, et al. Hypoxia adipose stem cell-derived exosomes promote high-quality healing of diabetic wound involves activation of PI3K/Akt pathways. J Nanobiotechnology 2021;19(1):202.
[Crossref] [Google Scholar] [PubMed]
- Wang F, Zhang C, Dai L, Zhang Y, Wang Y, Hao Y, et al. Bafilomycin A1 accelerates chronic refractory wound healing in db/db mice. Biomed Res Int 2020;2020:6265701.
[Crossref] [Google Scholar] [PubMed]
- Li J, Li N, Fu W, Feng JK, Zhang QF. Influence of silver ion dressing on central venous catheter-related infection in severe burn patients. Zhonghua Shao Shang Za Zhi 2020;36(8):698-703.
[Crossref] [Google Scholar] [PubMed]
- Wang R, Guo Y, Li B, Zheng J, Tang Z, Shu M. Application effect of silver-containing dressings in the repair of chronic refractory wounds. Evid Based Complement Alternat Med 2022;2022:3616923.
[Crossref] [Google Scholar] [PubMed]
- Ren H, Zhao F, Zhang Q, Huang X, Wang Z. Autophagy and skin wound healing. Burns Trauma 2022;10:tkac003.
[Crossref] [Google Scholar] [PubMed]
- Yamane H, Araki R, Doi A, Sato F, Tanaka K, Miyazaki N, et al. Successful wound healing of refractory digital ulcer in patient with systemic sclerosis by Waon therapy. J Cardiol Cases 2021;24(4):190-2.
[Crossref] [Google Scholar] [PubMed]
- Peng Y, Meng H, Li PX, Jiang YF, Fu XB. Research advances of stem cell-based tissue engineering repair materials in promoting the healing of chronic refractory wounds on the body surface. Zhonghua Shao Shang Za Zhi 2023;39(3):290-5.
[Crossref] [Google Scholar] [PubMed]
- Yang J, Chen Z, Pan D, Li H, Shen J. Umbilical cord-derived mesenchymal stem cell-derived exosomes combined pluronic F127 hydrogel promote chronic diabetic wound healing and complete skin regeneration. Int J Nanomedicine 2020;15:5911-26.
[Crossref] [Google Scholar] [PubMed]
- Changala M, Laberge J, Kerlan R, Taylor A, Arain M, Kirkwood K. Managing refractory postoperative fistulas as chronic wounds using Video-Assisted Hydrodebridement (VAHD). J Gastrointest Surg 2019;23(3):608-12.
[Crossref] [Google Scholar] [PubMed]
- Fu HD, Wang S, Ge B, Li LQ, Zeng HM, Shu QF, et al. Nerve growth factor and substance P may be involved in moist exposed burn ointment-mediated chronic refractory wound healing. Exp Ther Med 2018;16(3):1987-93.
[Crossref] [Google Scholar] [PubMed]
- Dong XM, Pei LL, Lu PS, Ni P, Yu BF, Fan ZQ. Bacteriological investigation and drug resistance analysis of chronic refractory wound secretions. J Craniofac Surg 2022;33(7):2028-30.
[Crossref] [Google Scholar] [PubMed]
- Tang J, Guan H, Dong W, Liu Y, Dong J, Huang L, et al. Application of compound polymyxin B ointment in the treatment of chronic refractory wounds. Int J Low Extrem Wounds 2022;21(3):320-4.
[Crossref] [Google Scholar] [PubMed]
- Dong W, Xiao YR, Wu MJ, Jiang DY, Nie LJ, Liu YK, et al. Thoughts and principles of diagnosis and treatment of chronic refractory wounds in China. Zhonghua Shao Shang Za Zhi 2018;34(12):868-73.
[Crossref] [Google Scholar] [PubMed]
- Martin P, Nunan R. Cellular and molecular mechanisms of repair in acute and chronic wound healing. Br J Dermatol 2015;173(2):370-8.
[Crossref] [Google Scholar] [PubMed]
- Rodrigues M, Kosaric N, Bonham CA, Gurtner GC. Wound healing: A cellular perspective. Physiol Rev 2019;99(1):665-706.
[Crossref] [Google Scholar] [PubMed]
- Talbott HE, Mascharak S, Griffin M, Wan DC, Longaker MT. Wound healing, fibroblast heterogeneity, and fibrosis. Cell Stem Cell 2022;29(8):1161-80.
[Crossref] [Google Scholar] [PubMed]
- Arunkumar P, Dougherty JA, Weist J, Kumar N, Angelos MG, Powell HM, et al. Sustained release of basic Fibroblast Growth Factor (bFGF) encapsulated Polycaprolactone (PCL) microspheres promote angiogenesis in vivo. Nanomaterials (Basel) 2019;9(7):1037.
[Crossref] [Google Scholar] [PubMed]
- Schmal H, Zwingmann J, Fehrenbach M, Finkenzeller G, Stark GB, Südkamp NP, et al. bFGF influences human articular chondrocyte differentiation. Cytotherapy 2007;9(2):184-93.
[Crossref] [Google Scholar] [PubMed]
- Chakrabarti S, Mazumder B, Rajkonwar J, Pathak MP, Patowary P, Chattopadhyay P. bFGF and collagen matrix hydrogel attenuates burn wound inflammation through activation of ERK and TRK pathway. Sci Rep 2021;11(1):3357.
[Crossref] [Google Scholar] [PubMed]