- *Corresponding Author:
- X. F. Long
Department of Internal Medicine Intensive Care Unit,
Affiliated Zhongshan Hospital of Dalian Universtity,
Dalian,
Liaoning 116001,
China
E-mail: longxiaofeng88@sina.com
| This article was originally published in a special issue, “Trending Topics in Biomedical Research and Pharmaceutical Sciences” |
| Indian J Pharm Sci 2022:84(1) Spl Issue “136-139” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
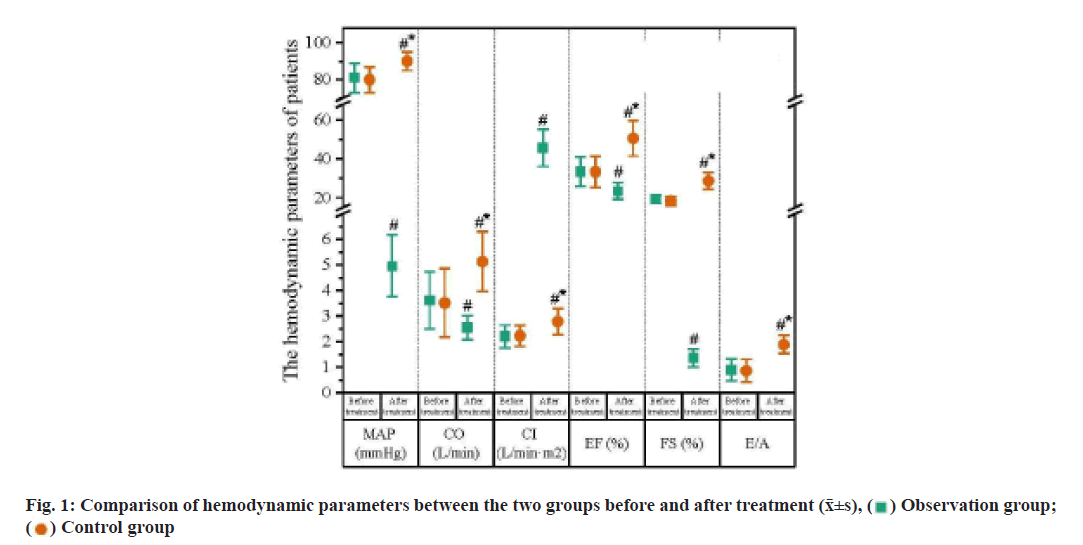
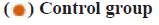
To investigate the efficacy of amiodarone on the heart failure patients with arrhythmia is the objective of the study. Between April 2018 and April 2020, 86 heart failure patients with arrhythmia who were admitted to the hospital for treatment were enrolled into the study and numbered, and according to the sequence of admission, they were randomized into the control group and observation group, with 43 patients in each group. Patients in two groups received the regular medication, while those in the observation group additionally took amiodarone. We measured the hemodynamic parameters of patients in two groups before and after treatment, including the mean arterial pressure, cardiac output, cardiac index, ejection fraction, fractional shortening and maximal flow velocity in early diastolic stage/maximal flow velocity in advanced diastolic stage, evaluated the efficacy and recorded the incidence rate of adverse reactions. Following the treatment, the effectiveness rate of patients in the observation group was significantly higher than that in the control group (c2=3.927, p<0.05), while the difference in the incidence rates of adverse reactions showed no statistical significance (p>0.05). Amiodarone in treatment of heart failure patients with arrhythmia can improve the heart function and efficacy, and thus it is safe and efficient in clinical practice.
Keywords
Amiodarone, arrhythmia, hemodynamic parameters, isosorbide mononitrate sustained release tablets, aspirin enteric-coated tablets, digoxin tablets
Chronic heart failure, as a persistent, progressive disease is mainly manifested by the inadequate cardiac compensation, frequently complicated with arrhythmia. Heart failure with arrhythmia represents the end stage in progression of heart diseases, plus the various factors, results in a high risk of cardiac sudden death that is 5 to 10 times compared to that of the healthy objects, thus being regarded as the major cause for death of patients [1,2]. Clinical evidence has shown the positive correlation between the age and incidence rate of heart failure with arrhythmia, especially the accelerated aging process in China that contributes to an obvious increase in the incidence rate and affects the health and life of people [3]. Clinically, the treatment mainly aims to improve the heart function and correct the arrhythmia. At present, medication is preferred in the treatment of heart failure complicated with arrhythmia that can mitigate the clinical symptoms effectively and be tolerated well for patients; moreover, it can be served as the auxiliary strategy for other methods [4]. Due to the negative inotropic effect, most of the anti-arrhythmia drugs are limited in clinical practice, while amiodarone, with mild negative inotropic effect, shows magnificent anti-arrhythmic effect [5]. Thus, in this study, we enrolled 86 heart failure patients with arrhythmia who were admitted to this hospital between April 2017 and April 2019 to analyze the effect of amiodarone on the heart failure patients with arrhythmia. Detailed information is reported as follows. Between April 2018 and April 2020, 86 heart failure patients with arrhythmia who were admitted to this hospital for treatment were enrolled into the study and numbered and according to the sequence of admission, they were randomized into the control group and observation group, with 43 patients in each group. There was no significant difference in sex distribution, age, disease duration and family history between the two groups (p>0.05), as shown in Table 1. All enrolled patients and their family agreed to participate in this study after they were informed of the protocol. Following the diagnosis, blood pressure and cardiac rhythm were monitored by use of an Echocardiogram (ECG) monitor. Patients in the two groups received the regular medication by oral administration of 40 mg isosorbide mononitrate sustained release tablets, once per day; aspirin entericcoated tablets 100 mg, once per day; digoxin tablets 0.125 mg, oral administration, once per day and furosemide tablets 40 mg, oral administration, once per day. Those in the observation group would additionally take the amiodarone hydrochloride injection (150 mg) and 5 % glucose (20 ml) via intravenous infusion. 30 min later after the vital signs and disease condition were under control, the dose of amiodarone was added by 150 mg; for patients with a decrease in heart rate, they were advised to take the amiodarone tablet (300 mg) via oral administration, once per day; for patients with heart rate below 55 beats/min, or blood pressure between 90/60 mmHg, amiodarone should be immediately withdrawn. Observation indexes used in this study was as follow. Heart function of patients in two groups was evaluated by the changes in the hemodynamic parameters before and after treatment. Before and after treatment, the Mean Arterial Pressure (MAP) was measured, and through the ECG, we determined the Cardiac Output (CO), Cardiac Index (CI), Ejection Fraction (EF), Fraction Shortening (FS) and the maximal flow rate in early diastolic phase/the maximal flow rate in advanced diastolic phase (E/A) of patients. We evaluated the clinical efficacy of patients in two groups and divided the results into three degrees [6]. Excellence-Patients had no or little clinical symptoms, with stable cardiac rhythm and improvement in heart function to Grade II or above. Improvement- After treatment, patients gained significant improvement in the clinical symptoms and more stable cardiac rhythm as compared to the level before treatment, with improvement in the heart function to Grade I or above. Failure-After treatment, patients gain no improvement, or even deterioration in clinical symptoms. Effective rate=(Excellence+Improvement)/43×100 %. Following treatment, we observed the anomaly in liver function, gastrointestinal discomfort or bradycardia of patients in two groups and calculated the incidence rate of adverse reactions as per the following formula. Incidence rate of adverse reaction=Cases of adverse reaction/43×100 %. Statistical Package for the Social Sciences (SPSS) 19.0 software was used to analyze the data of this study. Measurement data were presented as mean±standard deviation and compared by t test. Enumeration data were presented as n (%) and compared by use of chisquare test, p<0.05 suggested the relevant difference had statistical significance. Hemodynamic parameters of patients in two groups before and after treatment were compared. Following treatment, patients in two groups had significant improvement in the hemodynamic parameters and those in the observation group were more evident than the control group (p<0.05; fig. 1). The effectiveness rate of the treatment between two groups was compared. After treatment, the effectiveness rate in the control group was 72.09 %, significantly lower than 93.02 % in the observation group (χ2=3.927, p<0.05; Table 2). The incidence rate of the adverse reactions between two groups was compared. In two groups, adverse reactions were all observed after treatment and the incidence rate of the adverse reaction in the observation group was 6.98 %, approximating 9.30 % of the control group (p>0.05; fig. 2). Heart failure is the clinical syndrome caused by the heart functional disease or organic disease that compromises the ejection function, usually representing the end-stage of the heart disease. During the attack of heart failure, most of the patients suffer from the arrhythmia caused by the myocardial fibrosis, abnormal hypertrophy of myocardial cells, lesions in cardiac structure and congestion in systemic circulation, with clinical manifestations including shortness of breath, chest distress or palpitation, or the coldness in hand or foot, dizziness, headache, irregular palpitation or even precardiac convulsion, seizure or death [7,8]. Conventionally, clinical treatment is mainly carried out by the anti-heart failure treatment, while the positive treatment for anti-arrhythmia, improving the condition of patients and promoting the recovery of cardio version should be considered as well. Traditionally, clinical treatment for the heart failure patients complicated with arrhythmia mainly focuses on the baseline diseases and improvement of heart function. Previously, lidocaine is mostly used for treatment of arrhythmia as it can promote the efflux of potassium and inhibit the influx of sodium into the ventricular muscle, thereby decreasing the autorhythmicity. According to the clinical evidence, continuous intravenous administration of lidocaine usually triggers the mild negative ionotropic effect that may induce the instant or potential arrhythmia, so lidocaine is not the best choice for treatment of chronic heart failure complicated with arrhythmia [9,10]. Besides, heart failure usually interacts with the arrhythmia, which aggravates the myocardial ischemia, with the manifestation of anomaly in hemodynamics. Thus, in clinical treatment, ventricular arrhythmia should be corrected as soon as possible. Amiodarone is a kind of multi-channel blocker that can antagonize the arrhythmia and myocardial ischemia. Benzofuran, the major constituent of amiodarone, can be rapidly delivered to the target organs to decrease the autorhythmicity in the atrionector and atrioventricular junction, thereby rescuing the patients from the death caused by the heart failure complicated with arrhythmia [11,12]. Amiodarone, after medication, can hardly affect the myocardial contraction, let alone the negative ionotropic effect. Furthermore, amiodarone can promote the dilation of peripheral vessels, decrease the peripheral vascular resistance and cardiac afterload and eliminate the harmful free radicals, thereby protecting the myocardium and improving the heart function [13]. The findings of this study showed that after treatment, patients gained more evident improvement in the hemodynamic indicators than their counterparts in the control group, with a higher total effectiveness rate, suggesting that amiodarone performs well in improving the hemodynamics of heart failure patients with arrhythmia. This may attribute to the promising inhibitory effect of amiodarone on the rectifier potassium current, with mild negative ionotropic effect that can dilate the peripheral vessels and decrease the cardiac afterload, without any alteration in pump function of heart. After treatment, patients in two groups reported the adverse reactions, while the incidence rate of adverse reactions in the control group was 9.30 % and that in the observation group was 6.98 % (p>0.05). Thus, amiodarone is safe and reliable. To be concluded, amiodarone, in treatment of heart failure patients with arrhythmia, can improve the heart function and efficacy in patients with fewer adverse reactions including anomaly in liver function, gastrointestinal discomfort and bradycardia, and reliable efficacy and safety. Thus, it is worthy of being promoted in clinical practice.
| Group | Sex (Male/Female) | Age (year) | Disease duration (month) | Family history [n (%)] |
|---|---|---|---|---|
| Observation group (n=43) | 23/20 | 55.6±5.4 | 87.38±28.71 | 5(5.81) |
| Control group (n=43) | 26/17 | 56.4±5.6 | 84.24±31.15 | 4(4.65) |
Table 1: Comparison of General Materials between the two Groups (x¯±s, n=86)
| Group | N | Excellence | Improvement | Failure | Total effectiveness rate (%) |
|---|---|---|---|---|---|
| Observation group | 43 | 23 | 17 | 3 | 93.02 (40/43) |
| Control group | 43 | 10 | 21 | 12 | 72.09 (21/43) |
| χ2 | 3.927 | ||||
| p | 0.047 |
Table 2: Comparison of the Effectiveness Rate of Patients Between two Groups (n)
Conflict of interests:
The authors declared no conflict of interest.
References
- Luo YZ, Chen Y, He H. The effect of amiodarone on congestive heart failure with ventricular arrhythmia. China Med J 2015;12(8):57-60.
- Huang DJ, Zhang Z. Optimal medical therapy of chronic heart failure and prevention of sudden cardiac death. Chin J Card Arrhythm 2018;22(1):4-7.
- McAlister FA, Ezekowitz J, Hooton N, Vandermeer B, Spooner C, Dryden DM, et al. Cardiac resynchronization therapy for patients with left ventricular systolic dysfunction: A systematic review. JAMA 2007;297(22):2502-14.
[Crossref] [Google Scholar] [PubMed]
- Gao D, Sapp JL. Electrical storm: Definitions, clinical importance and treatment. Curr Opin Cardiol 2013;28(1):72-9.
[Crossref] [Google Scholar] [PubMed]
- Gasparini M, Lunati M, Landolina M, Santini M, Padeletti L, Perego G, et al. Electrical storm in patients with biventricular implantable cardioverter defibrillator: Incidence, predictors, and prognostic implications. Am Heart J 2008;156(5):847-54.
[Crossref] [Google Scholar] [PubMed]
- Tian HY, Zhang XS, Huangfu WZ. Echocardiography diagnostic value of clinical cardiac function classification in chronic heart failure (CHF). J Inner Mong Med Univ 2015;37(2):152-4.
- Nayak HM, Verdino RJ, Russo AM, Gerstenfeld EP, Hsia HH, Lin D, et al. Ventricular tachycardia storm after initiation of biventricular pacing: Incidence, clinical characteristics, management and outcome. J Cardiovasc Electrophysiol 2008;19(7):708-15.
[Crossref] [Google Scholar] [PubMed]
- Chen XG, Cao YK, Zhu YN. Study on the efficacy and safety of amiodarone in the treatment of critical patients with tachyarrhythmia. China Med J 2017;19(10):48-51.
- Yao YT. Clinical nursing observation of amiodarone in the treatment of heart failure with arrhythmia. Chin Med Clin 2016;16(3):445-7.
- Suzuki A, Shiga T, Nakai K, Futagawa K, Matsuyama Y, Shoda M, et al. Interlead difference between T-peak to T-end intervals in resynchronization patients with an implantable cardioverter-defibrillator. J Electrocardiol 2010;43(6):706-12.
- Nakai K, Miyake F, Kasanuki H, Shoda M, Futagawa K, Takahashi A, et al. Newly developed signal-averaged vector-projected 187-channel electrocardiogram can evaluate the spatial distribution of repolarization heterogeneity. Int Heart J 2008;49(2):153-64.
- Shiga T, Tanaka T, Irie S, Hagiwara N, Kasanuki H. Pharmacokinetics of intravenous amiodarone and its electrocardiographic effects on healthy Japanese subjects. Heart Vessels 2011;26(3):274-81.
[Crossref] [Google Scholar] [PubMed]
- Xiang ST, Li YL, Long PW. Drug treatment progress of heart failure with arrhythmia. Chin J Clin Health Care 2016;19(6):660-2.