- *Corresponding Author:
- Z. L. Lin
Thoracic Surgery Department,
The First People’s Hospital of Wenling,
Wenling 317500,
China
E-mail: lxiaolingabc@163.com
| This article was originally published in a special issue, “Diagnostic and Therapeutic Advances in Biomedical Research and Pharmaceutical Sciences” |
| Indian J Pharm Sci 2021:83(5)Spl Issue “224-230” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
To study the effects of perioperative psychological reinforcement intervention on negative emotion and quality of life in lung cancer patients is the main objective. 120 lung cancer patients were selected and divided into two groups: experimental group and control group. The control group was given routine nursing and the experimental group was given psychological nursing. The difference in profile of mood states-short form scores, University of California, Los Angeles loneliness scale and distress tolerance scores, European organisation for research and treatment of cancer quality of life questionnaire C30 scores between the two groups before and after the intervention was comparatively analyzed to reveal the correlation between negative emotions and quality of life as well as the effects of psychological reinforcement interventions on negative emotions and quality of life. The difference in profile of mood states-short form scores, University of California, Los Angeles loneliness scale and distress tolerance scores between the two groups after the intervention were observed. Where, the total profile of mood states-short form score was (17.28±5.41) points in the experimental group and (37.62±11.50) points in the control group after the intervention. Correlation between negative emotions and quality of life was shown and psychological reinforcement intervention had significant impact on negative emotions and quality of life. Perioperative psychological reinforcement intervention can significantly improve negative emotions in lung cancer patients, improving patient satisfaction and prognosis.
Keywords
Lung cancer, perioperative period, psychological reinforcement intervention, negative emotion, quality of life.
Lung cancer is a malignant tumor of bronchial mucosa epithelium or gland. Due to the fast increase in morbidity and mortality of the disease, it has also become one of the most threatening malignant tumors to people’s health and life [1,2]. In recent years, statistics have revealed that poor self-immunity and bad habits of smoking, etc., of the elderly makes incidence of lung cancer stay high in the elderly. The patient’s main manifestations include cough, fever, chest pain and blood sputum. Other organs of the body, etc., will be involved in the severe cases [3]. At present, clinical treatment of lung cancer mainly includes surgery and chemotherapy to prolong patient’s survival time [4,5]. Lung cancer patients need to stay in bed on a long-term basis for treatment and recuperation. Therefore, if nursing is untimely, patients will be prone to pressure sores or even paralysis, which seriously affects patient’s quality of life. Routine nursing often taken clinically has certain effects in improving the patient’s condition but the patient’s negative emotions are not obviously relieved. Studies have found that psychological reinforcement intervention can relieve patient’s negative emotions to a certain extent, leading to significant prognosis. Therefore, in this study, 120 lung cancer patients were studied to investigate the impact of perioperative psychological reinforcement intervention on negative emotion and quality of life in lung cancer patients [6,7].
Materials and Methods
General information:
120 lung cancer patients who received chemotherapy at the Central Hospital from May 2018 to May 2020 were selected as subjects. The patients had average age of (35.34±8.58) y, including 65 male patients and 55 female patients.
Inclusion criteria: All patients meet the diagnostic criteria for lung cancer; the patient’s clinical data are complete and accurate, with no contraindications to chemotherapy and other physical diseases; all subjects have signed informed consent.
Exclusion criteria: Lung cancer patients not diagnosed by pathological biopsy and cytology; patients who have received chemotherapy; patients with severe heart, liver and kidney organ failure or pregnant and lactating female patients; patients who cannot cooperate with this experiment [8,9].
Method:
The above 120 patients were divided into 2 groups, experimental group and control group. The control group was given routine nursing. The experimental group was given psychological nursing. That is, after the doctor and nurse understand the patient’s condition in detail, they actively communicate with the patient to know about the patient’s true ideas and take targeted counseling and psychological nursing to ease the patient’s negative mood and promote the patient’s quick recovery [10]. Changes in negative emotions and prognosis of the two groups are observed and comparatively analyzed.
Observation indicators and methods:
Comparative analysis of Profile Of Mood States- Short Form (POMS-SF) scores in the two groups before and after intervention: POMS-SF is mainly used to evaluate emotional changes of cancer patients before and after psychological intervention. The questionnaire consists of 30 adjectives, including 6 subscales of Tension-Anxiety (TA), Depression- Dejection (Dd), Anger-Hostility (Ah), Fatigue-Inertia (Fi), Confusion-Disorder (Cb) and Vitality-Activity (Va). The score is 0-4. Where, 0 means “not at all”, 1 means “slightly”, 2 means “sometimes”, 3 means “quite a lot” and 4 means “greatly”. Note that the first 5 subscales are negative scales, which means the mood is worse under a higher score, while VA is a positive scale, which means the mood is better under a higher score.
Comparison of POMS-SF, University of California, Los Angeles loneliness scale (ULS-8) and Distress Tolerance (DT) score differences between the two groups before and after the intervention: POMS-SF score difference is calculated as in comparative analysis of POMS-SF scores in the two groups before and after intervention. ULS-8 is a loneliness scale which contains 8 items. Where, 1 point means “never”, 2 points means “rarely”, 3 points means “sometimes” and 4 points means “always”. A higher patient’s score indicates stronger loneliness. DT is used to reflect the average pain experienced by the patient in the last week, with 1-3 points for mild pain, 4-6 points for moderate pain, 7-9 points for severe pain and 10 points for extreme pain [11,12].
Comparative analysis of European organisation for research and treatment of cancer quality of life questionnaire C30 (QLQ-C30) score between the two groups before and after the intervention: European organisation for research and treatment of cancer quality of life questionnaire C30 (QLQ-C30) contains a total of 30 items, including 5 functions of physical function, cognitive function, role function, emotional function and social function plus 3 symptoms of fatigue, pain, nausea and vomiting. Where, 1 point means “no completely”, 2 points means “a little”, 3 points means “quite a lot” and 4 points means “very much” [13,14]. A higher score in function indicates patient’s better functional status and quality of life; a higher score in symptom indicates more symptoms or problems, that is, worse quality of life.
Comparative analysis of QLQ-C30 score difference between the two groups before and after the intervention: QLQ-C30 score difference is calculated as in comparative analysis of POMS-SF scores in the two groups before and after intervention.
Correlation analysis of negative emotions and quality of life: According to the research results of comparative analysis of POMS-SF scores in the two groups, comparison of POMS-SF, ULS-8 and DT score differences between the two groups, comparative analysis of QLQ-C30 score between the two groups and comparative analysis of QLQ-C30 score difference between the two groups before and after the intervention, the correlation between POMS-SF, DT and ULS-8 and QLQ-C30 is analyzed.
Effect of time and intervention factors on quality of life and mood state: Combining the research results of comparative analysis of POMS-SF scores in the two groups, comparison of POMS-SF, ULS-8 and DT score differences between the two groups, comparative analysis of QLQ-C30 score between the two groups and comparative analysis of QLQ-C30 score difference between the two groups before and after the intervention, the effect of time and intervention factors on quality of life and mood state are analyzed.
Statistical methods:
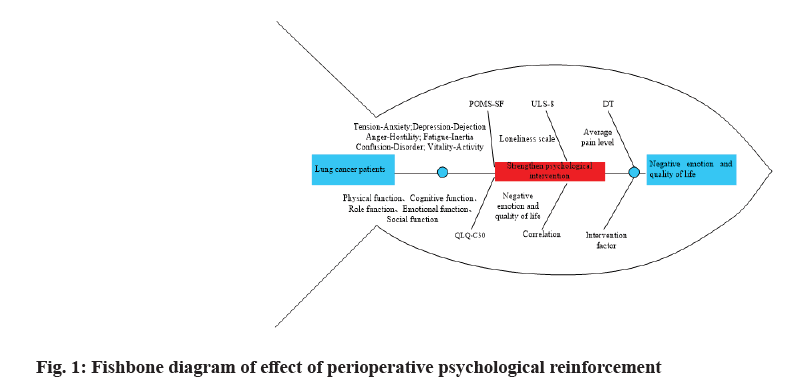
SPSS 20.0 software was used for statistical analysis of the experimental data. The experimental data are expressed as mean±standard deviation (x±s). One-way analysis of variance is used for significance analysis of data. p<0.05 indicates difference in data between the groups; p<0.01 indicates significant difference, as shown in fig. 1
Results and Discussion
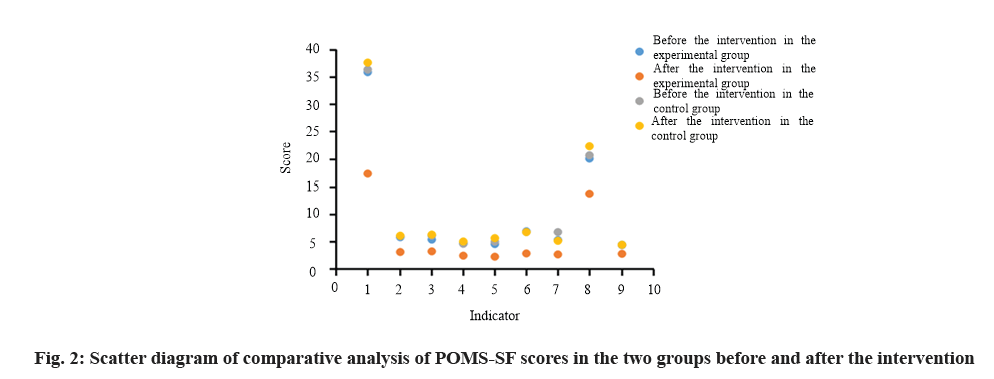
The total POMS-SF score is (35.86±12.39) points in the experimental group and (36.35±12.28) points in the control group before the intervention; the total POMS- SF score is (17.28±5.41) points in the experimental group and (37.62±11.50) points in the control group after the intervention. Comparative analysis shows that cancer patients have obvious negative emotions. The ULS-8 and DT scores are respectively (20.03±3.05) and (4.42±1.13) points in the experimental group before the intervention, which are respectively (13.74±2.12) and (2.74±0.73) points after the intervention. The ULS- 8 and DT scores are respectively (20.64±2.24) and (22.29±1.76) points in the control group before the intervention, which are respectively (4.31±0.73) and (4.40±0.83) points after the intervention. There is nostatistical difference in the total POMS-SF scores and the subscales between the experimental group and the control group before the intervention (p>0.05), showing comparability; statistical difference is shown after the intervention (p<0.05), shown in Table 1.
| Item | Experimental group (n1=60) | Control group (n2=60) | ||||||
|---|---|---|---|---|---|---|---|---|
| Before the intervention | After the intervention | t | p | Before the intervention | After the intervention | t | p | |
| Total POMS-SF score | 35.86±12.39 | 17.28±5.41 | 7.54 | 0.001 | 36.35±12.28 | 37.62±11.50 | -1.759 | 0.19 |
| TA | 5.78 ± 2.76 | 3.07±1.61 | 4.55 | 0.001 | 5.95±2.76 | 6.06±2.50 | -1.187 | 0.245 |
| DD | 5.34±2.22 | 3.19±1.61 | 4.76 | 0.001 | 6.07±2.73 | 6.26±2.32 | -0.394 | 0.684 |
| AH | 4.68±2.88 | 2.40±1.14 | 4.95 | 0.001 | 4.57±2.48 | 5.00±2.41 | -0.983 | 0.325 |
| FI | 4.52±3.07 | 2.21±1.86 | -4.97 | 0.001 | 4.97±2.79 | 5.62±1.61 | -3.164 | 0.002 |
| CB | 6.87±1.97 | 2.81±1.14 | 4.27 | 0.001 | 6.73±2.16 | 6.72±2.14 | 0.641 | 0.562 |
| VA | 5.28±7.62 | 2.63±2.54 | -5.70 | 0.001 | 6.73±2.16 | 5.12±1.83 | -0.113 | 0.905 |
| ULS-8 | 20.03±3.05 | 13.74±2.12 | 17.4 | 0.001 | 20.64±2.24 | 22.29±1.76 | -4.04 | 0.001 |
| DT | 4.42±1.13 | 2.74±0.73 | -5.77 | 0.001 | 4.31±0.73 | 4.40±0.83 | -0.75 | 0.451 |
Table 1: Comparison of the Success Rate of Weaning Between The Two Groups
As shown in fig. 2, Note: 1 means total POMS-SF score; 2 means TA; 3 means DD; 4 means AH; 5 means FI; 6 means CB; 7 means VA; 8 means ULS-8; 9 means DT [15].
There are statistically significant differences in POMS- SF, ULS-8 and DT scores between the two groups before and after the intervention (p<0.05) (Table 2).
| Item | Experimental group (n1=60) | Control group (n2=60) | t | p | ||||
|---|---|---|---|---|---|---|---|---|
| Before the intervention | After the intervention | Difference value | Before the intervention | After the intervention | Difference value | |||
| Total POMS-SF score | 35.86±12.39 | 17.28±5.41 | 18.58±5.69 | 36.35±12.28 | 37.62±11.50 | 1.27±11.75 | 7.25 | 0.001 |
| TA | 5.78±2.76 | 3.07±1.61 | 2.71±1.89 | 5.95±2.76 | 6.06±2.50 | 0.11±2.66 | 6.58 | 0.001 |
| DD | 5.34±2.22 | 3.19±1.61 | 2.15±1.98 | 6.07±2.73 | 6.26±2.32 | 0.19±2.68 | 5.85 | 0.001 |
| AH | 4.68±2.88 | 2.40±1.14 | 2.28±2.65 | 4.57±2.48 | 5.00±2.41 | 0.43±2.45 | 5.63 | 0.001 |
| FI | 4.52±3.07 | 2.21±1.86 | 2.31±2.85 | 4.97±2.79 | 5.62±1.61 | 0.65±2.54 | 5.32 | 0.001 |
| CB | 6.87±1.97 | 2.81±1.14 | 4.06±1.87 | 6.73±2.16 | 6.85±2.14 | 0.2±2.14 | 7.05 | 0.001 |
| VA | 5.28±7.62 | 2.63±2.54 | 2.65±5.60 | 6.73±2.16 | 7.12±1.83 | 0.39±1.89 | 6.74 | 0.001 |
| ULS-8 | 20.03±3.05 | 13.74±2.12 | 6.29±2.74 | 20.64±2.24 | 22.29±1.76 | 1.65±2.01 | 14.60 | 0.001 |
| DT | 4.42±1.13 | 2.74±0.73 | 1.68±0.85 | 4.31±0.73 | 4.40±0.83 | 0.09±0.75 | 7.50 | 0.001 |
Table 2: Comparative Analysis of Difference in POMS-SF, ULS-8 and DT Scores before and after the Intervention (X±S)
After the intervention, except for diarrhea, the scores of functional areas in the experimental group show a significant upward trend, while the scores of symptoms and single test items decrease, showing statistically significant difference (p<0.05); except for dyspnea and financial difficulty (p<0.05), the scores of other items in the control group show no statistically significant difference before and after the intervention (p>0.05), shown in Table 3.
| Item | Experimental group (n1=60) | Control group (n2=60) | ||||||
|---|---|---|---|---|---|---|---|---|
| Before the intervention | After the intervention | t | p | Before the intervention | After the intervention | t | p | |
| Functional area | ||||||||
| Physical function | 8.67±3.32 | 11.10±1.63 | 5.25 | 0.001 | 8.76±2.48 | 8.65±2.33 | 1.102 | 0.312 |
| Role function | 2.09±1.48 | 3.58±0.88 | 3.67 | 0.001 | 2.89±1.45 | 2.71±1.02 | 0.755 | 0.452 |
| Cognitive function | 3.67±1.48 | 4.21±0.61 | 2.70 | 0.001 | 3.83±1.07 | 3.33±0.90 | 1.875 | 0.065 |
| Emotional function | 7.53±2.40 | 7.95±0.71 | 4.91 | 0.001 | 7.78±2.45 | 3.71±1.03 | 0.592 | 0.695 |
| Social function | 3.11±1.40 | 4.37±0.98 | 3.48 | 0.001 | 3.33±1.56 | 7.36±0.82 | 1.725 | 0.485 |
| Overall health condition | 7.74±1.54 | 8.17±0.94 | 4.07 | 0.001 | 7.88±1.22 | 2.60±1.21 | 1.942 | 0.170 |
| Symptom/single item | ||||||||
| Fatigue | 2.81±1.62 | 2.26±0.76 | 4.84 | 0.001 | 2.58±1.95 | 2.60±1.21 | 0.043 | 0.956 |
| Pain | 2.74±1.64 | 1.84±0.81 | 7.36 | 0.001 | 2.49±1.46 | 2.21±1.05 | 4.254 | 0.382 |
| Nausea and vomiting | 2.28±1.75 | 1.19±0.45 | 5.19 | 0.001 | 2.09±1.68 | 2.31±1.35 | 1.050 | 0.285 |
| dyspnea | 1.88±0.83 | 1.16±0.49 | 4.26 | 0.001 | 2.18±1.10 | 1.74±0.80 | 2.262 | 0.025 |
| Insomnia | 2.18±0.84 | 1.63±0.49 | 4.75 | 0.001 | 2.06±0.75 | 2.36±0.75 | 1.679 | 0.095 |
| Loss of appetite | 2.80±0.73 | 1.95±0.62 | 4.50 | 0.001 | 2.54±0.95 | 2.60±0.83 | 0.470 | 0.638 |
| Constipation | 1.96±1.05 | 1.33±0.61 | 2.87 | 0.001 | 1.82±0.83 | 1.98±0.90 | 0.965 | 0.336 |
| Diarrhea | 1.18±0.46 | 1.02±0.15 | 4.67 | 0.001 | 1.25±0.44 | 1.12±0.33 | 0.441 | 0.285 |
| Financial difficulty | 2.56±0.82 | 3.23±0.57 | 4.274 | 0.001 | 2.86±0.78 | 3.40±0.59 | 3.290 | 0.001 |
Table 3: Comparative Analysis of QLQ-C30 Scores between the Experimental Group and the Control Group Before the Intervention (x±s)
In terms of difference in quality of life (QLQ-C30) scores between the two groups before and after the intervention, except for social function, dyspnea, diarrhea and financial difficulty which show no statistically significant difference (p>0.05), scores of other indicators show statistically significant difference before and after the intervention (p<0.05) shown in Table 4.
| Item | Experimental group (n1=60) | Control group (n2=60) | t | p | ||||
|---|---|---|---|---|---|---|---|---|
| Before the intervention | After the intervention | Difference value | Before the intervention | After the intervention | Difference value | |||
| Functional area | ||||||||
| Physical function | 8.67±3.32 | 11.10±1.63 | 2.47±2.03 | 8.76±2.48 | 8.65±2.33 | -0.09±2.38 | 4.029 | 0.001 |
| Role function | 2.09±1.48 | 3.58±0.88 | 1.49±0.94 | 2.89±1.45 | 2.71±1.02 | -0.17±1.35 | 3.686 | 0.001 |
| Cognitive function | 3.67±1.48 | 4.21±0.61 | 0.54±0.69 | 3.83±1.07 | 3.33±0.90 | -0.48±1.06 | 6.158 | 0.001 |
| Emotional function | 7.53±2.40 | 7.95±0.71 | 0.42±1.31 | 7.78±2.45 | 3.71±1.03 | 0.08±2.45 | 7.685 | 0.001 |
| Social function | 3.11±1.40 | 4.37±0.98 | 1.26±1.18 | 3.33±1.56 | 7.36±0.82 | 0.40±1.46 | 1.823 | 0.085 |
| Overall health condition | 7.74±1.54 | 8.17±0.94 | 0.43±0.72 | 7.88±1.22 | 2.60±1.21 | -0.50±0.92 | 6.852 | 0.001 |
| Symptom/single item | ||||||||
| Fatigue | 2.81±1.62 | 2.26±0.76 | -0.55±1.23 | 2.58±1.95 | 2.60±1.21 | 0.03±1.16 | 3.653 | 0.001 |
| Pain | 2.74±1.64 | 1.84±0.81 | -0.88±0.67 | 2.49±1.46 | 2.21±1.05 | -0.27±0.98 | 4.152 | 0.001 |
| Nausea and vomiting | 2.28±1.75 | 1.19±0.45 | -1.07±0.85 | 2.09±1.68 | 2.31±1.35 | 0.24±1.10 | 3.895 | 0.001 |
| dyspnea | 1.88±0.83 | 1.16±0.49 | -0.70±0.44 | 2.18±1.10 | 1.74±0.80 | -0.45±0.79 | 1.260 | 0.306 |
| Insomnia | 2.18±0.84 | 1.63±0.49 | -0.53±0.60 | 2.06±0.75 | 2.36±0.75 | 0.33±1.04 | 5.682 | 0.001 |
| Loss of appetite | 2.80±0.73 | 1.95±0.62 | -0.84±1.05 | 2.54±0.95 | 2.60±0.83 | 0.10±0.86 | 3.561 | 0.001 |
| Constipation | 1.96±1.05 | 1.33±0.61 | -0.60±1.13 | 1.82±0.83 | 1.98±0.90 | 0.17±0.89 | 2.652 | 0.015 |
| Diarrhea | 1.18±0.46 | 1.02±0.15 | -0.12±0.37 | 1.25±0.44 | 1.12±0.33 | -0.09±0.71 | 0.185 | 0.865 |
| Financial difficulty | 2.56±0.82 | 3.23±0.57 | 0.65±0.64 | 2.86±0.78 | 3.40±0.59 | 0.57±0.43 | 0.052 | 0.856 |
Table 4: Comparative Analysis of QLQ-C30 Score Difference between the two Groups before and after the Intervention (x±s)
Correlation analysis between QLQ-C30 item scores and total POMS-SF scores, subscale scores, loneliness scores and psychological pain scores shows that the general trend in that the functional areas of quality of life are significantly correlated with negative emotions (p<0.05), the symptom areas and single items are significantly correlated with negative emotions (p<0.05) shown in Table 5.
| QLQ-C30 | TA | FI | DD | AH | CD | VA | Total POMS-SF score | ULS-8 | DT |
|---|---|---|---|---|---|---|---|---|---|
| Physical function | 0.025 | 0.263 | 0.052 | 0.052 | 0.052 | 0.063 | 0.065 | 0.141 | 0.279 |
| Role function | 0.012 | 0.285 | 0.063 | 0.084 | 0.065 | 0.008 | 0.152 | 0.185 | 0.120 |
| Emotional function | 0.456 | 0.201 | 0.582 | 0.465 | 0.043 | 0.052 | 0.625 | 0.263 | 0.123 |
| Cognitive function | 0.165 | 0.305 | 0.26 | 0.083 | 0.038 | 0.165 | 0.263 | 0.254 | 0.196 |
| Social function | 0.085 | 0.185 | 0.284 | 0.082 | 0.082 | 0.075 | 0.152 | 0.056 | 0.155 |
| Overall health condition | 0.089 | 0.186 | 0.167 | 0.186 | 0.125 | 0.103 | 0.012 | 0.082 | 0.241 |
| Nausea and vomiting | 0.065 | 0.011 | 0.34 | 0.26 | 0.070 | 0.036 | 0.011 | 0.028 | 0.001 |
| Fatigue | 0.024 | 0.23 | 0.165 | 0.256 | 0.096 | 0.080 | 0.263 | 0.264 | 0.023 |
| Pain | 0.238 | 0.184 | 0.238 | 0.233 | 0.154 | 0.029 | 0.305 | 0.380 | 0.168 |
| Dyspnea | 0.147 | 0.162 | 0.154 | 0.118 | 0.056 | 0.050 | 0.262 | 0.054 | 0.012 |
| Insomnia | 0.084 | 0.325 | 0.207 | 0.205 | 0.286 | 0.016 | 0.238 | 0.058 | 0.025 |
| Loss of appetite | 0.063 | 0.275 | 0.085 | 0.241 | 0.019 | 0.105 | 0.294 | 0.063 | 0.227 |
| Constipation | 0.176 | 0.023 | 0.267 | 0.261 | 0.145 | 0.056 | 0.164 | 0.025 | 0.052 |
| Diarrhea | 0.096 | 0.042 | 0.203 | 0.045 | 0.087 | 0.063 | 0.245 | 0.362 | 0.053 |
| Financial difficulty | 0.123 | 0.182 | 0.308 | 0.108 | 0.056 | 0.196 | 0.063 | 0.215 | 0.065 |
Table 5: Correlation Analysis of Negative Emotions and Quality of Life
The impact of perioperative psychological reinforcement intervention on negative emotions and quality of life in lung cancer patients is analyzed. Perioperative psychological reinforcement is an intervention factor that exerts insignificant effect on loss of appetite, diarrhea and financial difficulty in QLQ-C30 with statistical difference (p>0.05), but significant effect is exerted on other areas of quality of life and mood state, showing statistical differences (p<0.05). At the same time, except for social function, dyspnea, diarrhea and financial difficulty in QLQ-C30, there is interaction between intervention factors and time factors in other areas and mood state (p<0.05).
Lung cancer is a common malignant tumor in China, which shows gradually increasing incidence under gradually increasing pressure and influence of external factors such as irregular life, seriously threatening patient’s health and quality of life. Moreover, most patients are in advanced stage in clinical examination [16]. Recent years witness high incidence of lung cancer in the elderly, mainly due to reduced immunity in the elderly [17]. Clinical investigation found that most patients currently take rest after surgery, which brings certain negative emotions [18]. The conventional nursing methods adopted in clinical practice display some drawbacks, such as emotional instability which leads to a decline in rehabilitation ability. Comparatively speaking, psychological reinforcement intervention can significantly relieve negative emotions and improve quality of life in lung cancer patients [19]. The results of this experiment indicate that perioperative psychological reinforcement intervention can significantly improve negative emotions of lung cancer patients, thereby improving patient satisfaction and prognosis.
Psychological reinforcement intervention can relieve negative emotions of lung cancer patients to a certain extent and help patients positively face occurrence and treatment of the disease. Firstly, it creates a harmonious relationship between medical staff and patients, which will relieve the patient’s anxiety so that patients receive treatment more easily, thereby improving psychological state. Secondly, it provides psychological counseling to effectively help patients solve their physical and psychological problems based on patient’s treatment plan. Thirdly, it provides a good and comfortable environment for rapid postoperative recovery as well as corresponding dietary supplement to promote the improvement of the patient’s lung tissue function, thereby improving quality of life.
To conclude, the impact of perioperative psychological reinforcement intervention on negative emotions and quality of life in lung cancer patients is scientifically studied. By giving comprehensive consideration to various factors such as medical, social and economic factors, etc., standardized psychological nursing can provide patients with comprehensive treatment plan to effectively improve the nursing quality and patient’s acceptability. To enable more scientific grasp of the condition of the disease, rehabilitation treatment and research on its pathogenesis and rules should be carried out to lay a theoretical foundation and provide corresponding technical support to help patient’s rehabilitation and future research.
Conflicts of interest:
The authors declared no conflict of interest.
References
- Wang TT, He LY, Zhang M, Wang SM, Zhao AG, Chu L, et al. Development of improved version of quality of life assessment instrument for lung cancer patients based on traditional Chinese medicine (QLASTCM-Lu). Chin J Integr Med 2019;25(11):831-6.
- Van Der Weijst L, Lievens Y, Schrauwen W, Surmont V. Health-related quality of life in advanced non-small cell lung cancer: a methodological appraisal based on a systematic literature review. Front Oncol 2019;9:715.
- Saranya K, Sreejith K, Ajaykumar. Comparison of quality of life of patients on treatment with cisplatin and gemcitabine, carboplatin and gemcitabine, carboplatin and paclitaxel, carboplatin and pemetrexed for non-small cell lung cancer. J Oncol Pharm Pract 2019;25(8):1853-9.
- Marinho AP, Fin G, Baptistella AR, Nodari Júnior RJ, Benetti M. Translation and cultural adaptation of the European Organisation for research and treatment of cancer quality of life questionnaire-lung cancer module for quality of life assessment in patients with lung cancer in Brazil. J Bras Pneumol 2019;45(4).
- Oh S, Ryu E. Does holding back cancer-related concern affect couples marital relationship and quality of life of patients with lung cancer? An actor–partner interdependence mediation modeling approach. Asian Nurs Res 2019;13(4):277-85.
- Lenderking WR, Lin H, Speck RM, Zhu Y, Huang H, Huang J, et al. Patient-reported outcomes and quality of life in advanced ALK+non-small-cell lung cancer trial of brigatinib (ALTA). Future Oncol 2019;15(24):2841-55.
- Franciosi V, Maglietta G, Degli Esposti C, Caruso G, Cavanna L, Berte R, et al. Early palliative care and quality of life of advanced cancer patients-a multicenter randomized clinical trial. Ann Palliat Med 2019;8(4):381-9.
- Kaneko Y, Mouri T, Seto Y, Nishioka N, Yoshimura A, Yamamoto C, et al. The quality of life of patients with suspected lung cancer before and after bronchoscopy and the effect of mirtazapine on the depressive status. Intern Med 2020;59(13):1605-10.
- Kawaguchi Y, Hanaoka J, Ohshio Y, Okamoto K, Kaku R, Hayashi K, et al. Sarcopenia predicts poor postoperative outcome in elderly patients with lung cancer. Gen Thorac Cardiovasc Surg 2019;67(11):949-54.
- Kedia SK, Collins A, Dillon PJ, Akkus C, Ward KD, Jackson BM. Psychosocial interventions for informal caregivers of lung cancer patients: A systematic review. Psychooncology 2020;29(2):251-62.
- Jankowska-Polanska B, Polanski J, Chabowski M, Rosinczuk J, Mazur G. Influence of coping strategy on perception of anxiety and depression in patients with non-small cell lung cancer. Trends Biomed Res 2019:57-70.
- Su T, He C, Li X, Xiao L, He J, Bai Y, et al. Association between early informed diagnosis and survival time in patients with lung cancer. Psychooncology 2020;29(5):878-85.
- Arbour KC, Riely GJ. Systemic therapy for locally advanced and metastatic non–small cell lung cancer: a review. JAMA 2019;322(8):764-74.
- Pongthavornkamol K, Lekdamrongkul P, Pinsuntorn P, Molassiotis A. Physical symptoms, unmet needs and quality of life in thai cancer survivors after the completion of primary treatment. Asia Pac J Oncol Nurs 2019;6(4):363-71.
- de Mol M, Visser S, Aerts J, Lodder P, van Walree N, Belderbos H, et al. The association of depressive symptoms, personality traits and sociodemographic factors with health-related quality of life and quality of life in patients with advanced-stage lung cancer: an observational multi-center cohort study. BMC Cancer 2020;20:1-4.
- Van Dams R, Grogan T, Lee P, Punglia R, Raldow A. Impact of health-related quality of life and prediagnosis risk of major depressive disorder on treatment choice for stage I lung cancer. JCO Clin Cancer Inform 2019;1:1-8.
- de Mol M, Visser S, den Oudsten BL, Lodder P, van Walree N, Belderbos H, et al. Frequency of low-grade adverse events and quality of life during chemotherapy determine patients’ judgement about treatment in advanced-stage thoracic cancer. Support Care Cancer 2019;27(9):3563-72.
- Casebeer AW, Antol DD, Hopson S, Khoury R, Renda A, Parikh A, et al. Using the healthy days measure to assess factors associated with poor health-related quality of life for patients with metastatic breast, lung, or colorectal cancer enrolled in a Medicare advantage health plan. Popul Health Manag 2019;22(5):440-8.
- Mazieres J, Kowalski D, Luft A, Vicente D, Tafreshi A, Gumus M, et al. Health-related quality of life with carboplatin-paclitaxel or nab-paclitaxel with or without pembrolizumab in patients with metastatic squamous non-small-cell lung cancer. J Clin Oncol 2020;38(3):271-80.