- *Corresponding Author:
- Li Ma
Department of Anesthesiology,People's Hospital of Guangxi Zhuang Autonomous Region, Nanning 530022, Guangxi Zhuang Autonomous Region, China
E-mail: nanningchestnut@163.com
| Date of Received | 27 July 2020 |
| Date of Revision | 28 February 2021 |
| Date of Acceptance | 22 June 2021 |
| Indian J Pharm Sci 2021;83(3):603-609 |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
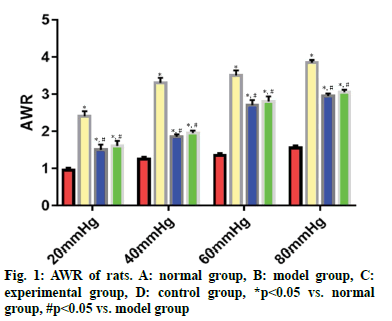
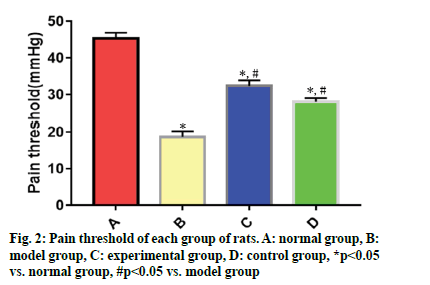
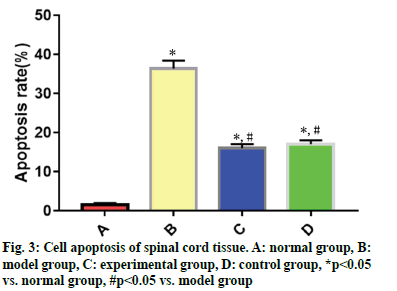
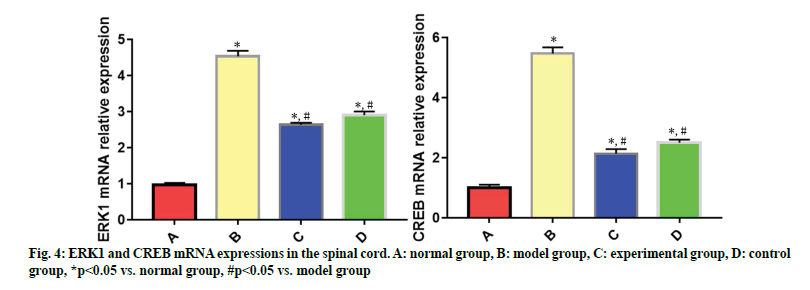
To evaluate the protective effects of dexmedetomidine on the colon and spinal cord of rats with functional chronic visceral pain and its regulatory mechanism on extracellular signal-regulated kinase 1-cyclic adenosine monophosphate response element-binding protein signaling pathway. A rat model of irritable bowel syndrome was established by colorectal distention stimulation. Animals were categorized into normal group, model group, experimental group and control group. No treatment was given in normal group, while colorectal distention stimulation was utilized in model group, experimental group and control group. After successful modeling, the animals in experimental group were injected intraperitoneally with 5 μg/kg of dexmedetomidine hydrochloride injection daily, those in control group were injected intraperitoneally with 5 μg/kg pinaverium bromide daily and those in normal group and model group were injected intraperitoneally daily with the same volume of normal saline, for 14 consecutive days. Abdominal withdrawal reflex score and pain threshold of rats were measured. Cell apoptosis in the spinal cord of rats was determined by terminal deoxynucleotidyl transferase-mediated dUTP nick end labeling staining. The messenger ribonucleic acid expressions of extracellular signal-regulated kinase 1 and cyclic adenosine monophosphate response element-binding protein in the spinal cord were detected by realtime quantitative polymerase chain reaction and phosphorylated-extracellular signal-regulated kinase 1 and phosphorylated-cyclic adenosine monophosphate response element-binding protein expressions in the spinal cord of rats were tested by Western blotting. Compared with normal group, abdominal withdrawal reflex score, cell apoptosis rate, messenger ribonucleic acid expressions of extracellular signal-regulated kinase 1 and cyclic adenosine monophosphate response element-binding protein, phosphorylatedextracellular signal-regulated kinase 1 and phosphorylated-cyclic adenosine monophosphate response element-binding protein expressions were significantly higher (p<0.05) and pain threshold value was significantly lower (p<0.05) in model group, experimental group and control group at 20 mmHg, 40 mmHg, 60 mmHg and 80 mmHg pressures. Abdominal withdrawal reflex score, cell apoptosis rate, messenger ribonucleic acid expressions of extracellular signal-regulated kinase 1 and cyclic adenosine monophosphate response element-binding protein, phosphorylated-extracellular signal-regulated kinase 1 and phosphorylated-cyclic adenosine monophosphate response element-binding protein expressions were significantly lower (p<0.05) and pain threshold value was significantly higher (p<0.05) in experimental group and control group than those in model group at 20 mmHg, 40 mmHg, 60 mmHg and 80 mmHg pressures. Dexmedetomidine can prominently ameliorate the clinical symptoms of rats with functional chronic visceral pain and may protect the colon and spinal cord by inhibiting the extracellular signalregulated kinase 1/cyclic adenosine monophosphate response element-binding protein signaling pathway.
Keywords
Dexmedetomidine, functional chronic visceral pain, irritable bowel syndrome, extracellular signal-regulated kinase 1, cyclic adenosine monophosphate response element-binding protein
Functional chronic visceral pain caused by irritable bowel syndrome (IBS) is a persistent and recurrent disease that seriously affects the physical and mental health and normal life of patients. Functional chronic visceral pain is a chronic gastrointestinal disorder involving the digestive system, mainly manifested by abdominal pain and bloating, as well as changes in bowel habits and stool trxaits[1]. At present, the molecular mechanism of the disease is still under investigation and previous basic research and clinical data have indicated that genetics, environment, abnormal gastrointestinal motility, endocrine disorders, reduced immune function and high visceral sensitivity are all the factors affecting the progression of the disease[2]. Zhuo et al.[3] reported that ameliorating the disorders of brain-gut axis in patients with IBS could significantly alleviate clinical symptoms such as abdominal pain and abdominal discomfort, but the authors did not elucidate the mechanism of action. Giummarra et al.[4] reported that the spinal cord, serving as an important central nervous system connecting the brain-gut axis, was of crucial importance in the abdominal or thoracic organ pain. Extracellular signal-regulated kinase 1 (ERK1)-cyclic adenosine monophosphate response element-binding protein (CREB) signaling pathway plays an important role in the occurrence, progression, persistence or repair and disappearance of the pain[5]. Sun et al.[6] reported that inhibiting the phosphorylation of the ERK1/CREB signaling pathway in a rat model of inflammatory visceral pain could significantly reduce the pain behavior of experimental animals. Clinically, dexmedetomidine is a α2-adrenergic receptor agonist with good sedative, analgesic and organ protection effects. A previous study demonstrated that dexmedetomidine can down regulate the release of inflammatory factors and polarization of interneurons in central tissues by reducing the release of glutamate, thus inhibiting the transmission of pain[7]. However, there is little research about dexmedetomidine in IBS. In this study, a rat model of IBS was established, aiming to explore the mechanism of dexmedetomidine on IBS pain transmission from the perspective of the ERK1/CREB signaling pathway in the spinal cord, so as to provide new reference for the clinical medication of IBS.
Materials and Methods
Experimental animals, main reagents and apparatus:
Full term newborn specific pathogen free (SPF) grade male Sprague-Dawley (SD) rats, weighing 6-8 g, were purchased from Beijing Jinmuyang Experimental Animal Breeding Co., Ltd., animal license number: SYXK (Beijing): 2020-0007. In the SPF grade animal room of the Animal Experiment Center of our hospital, 5 newborn rats and 1 SD lactating rat were kept in the same cage and the lactating rats were fed at 20-25°, given free access to food and water, with day and night natural light. The research purpose and operation of this study were reviewed and approved by the Animal Care and Use Committee of our hospital.
Dexmedetomidine Hydrochloride Injection [2 ml:0.2 mg, Yangtze River Pharmaceutical (Group) Co., Ltd., NMPN: H20183219], Pinaverium Bromide Tablets [50 mg×15 s, Mylan Laboratories SAS (France), approval number: 20160396], hematoxylin-eosin (HE) staining kits (Roche, USA), Western blotting kits (Roche, USA), phenobarbital sodium (Beijing Solarbio Science & Technology Co., Ltd.), paraformaldehyde solution [Beyotime Biotechnology Co., Ltd. (Shanghai, China)] and phosphorylated-ERK1 (p-ERK1) and phosphorylated-CREB (p-CREB) (Cell Signaling Technology, Inc., USA) were prepared.
The instruments included a biological fluorescence microscope (Nikon, Japan), an electron microscope (JEOL, Japan), an animal-related surgical equipment package (Zhangjiagang Dadu Medical Instruments Co., Ltd.), an ultra-thin microtome (Thermo, USA), a gel electrophoresis system (Bio-Rad, USA) and a tissue grinding machine (Keller Instruments Co., Ltd.).
Establishment of model of functional chronic visceral pain and grouping:
The newborn rats were adaptively fed for later experiments. First, they were categorized into normal group (n=10), model group (n=10), experimental group (n=10) and control group (n=10) using a random number table. No treatment was given in normal group, while according to the methods proposed by Grabauskas et al.[8], newborn rats in model group, experimental group and control group were treated with colorectal distention (CRD) stimulation for 2 min, once a day, in the awake state within 8-21 d after birth to establish a rat model of functional chronic visceral pain. The specific operations involved: First, a lubricated self-made balloon occluder was inserted into the anus to a depth of about 2 cm. Next, a volume of 0.25 ml gas was inflated into the balloon occluder with a medical tiny syringe. After lasting for 1 min, the balloon occluder was deflated and taken out. About 2 h later, the above operation was repeated once. After stimulation, the newborn rats were fed routinely. When animals grew to 8 w of age, abdominal withdrawal reflex (AWR) score and pain threshold of rats were measured. The significant difference in AWR score and pain threshold from experimental animals meant the successful modeling.
After 8 w of successful modeling, the animals in experimental group were injected intraperitoneally with 5 μg/kg of dexmedetomidine hydrochloride injection daily, those in control group were injected intraperitoneally with 5 μg/kg pinaverium bromide daily[9] and those in normal group and model group were injected intraperitoneally daily with the same volume of normal saline, for 14 consecutive days.
Measurement of rat AWR:
After fasting for 12 h, the rats were anesthetized by ether inhalation. The balloon occluder was inserted into the anus to a depth of about 2 cm. Subsequently, the rats were placed in a transparent container (20 cm×10 cm×10 cm). After the rats were awake, the self-made distention balloon was connected to a sphygmomanometer to adjust the pressure using a three-way tube and CRD stimulation (20 mmHg, 40 mmHg, 60 mmHg and 80 mmHg pressure levels) was given, each for 20 s at an interval of 5 min, 3 times for each pressure level. The scoring standards were as follows[10]: 0 points: animals without obvious behavior changes, 1 point: animals with their heads upward but no abdominal muscle contraction, 2 points: animals with slight abdominal muscle contraction but no abdominal muscle lifting, 3 points: animals with strong abdominal muscle contraction and abdominal muscle lifting, but no pelvic lifting and 4 points: animals with body lifting, pelvis lifting off the table and arched abdomen.
Measurement of pain threshold:
Preliminary preparations were the same as above. CRD stimulation started from 15 mmHg, with a pressure increase gradient of 5 mmHg, each for 20 s at an interval of 5 min. When the animal’s AWR score reached 3 points, the pressure value was the pain threshold of the rat[11].
Cell apoptosis in the spinal cord:
The spinal cord was extracted from each group of rats and pretreated in accordance with the instructions of terminal deoxynucleotidyl transferase-mediated dUTP nick end labeling (TUNEL) staining kits, followed by antigen retrieval, sealing, labeling, dark staining, dehydration, neutral gum mounting and microscopic examination. The cells with green fluorescence in the field of view were considered as apoptotic cells[12]. The ratio of the number of TUNEL positive cells to the total cells indicated the cell apoptosis rate.
ERK1 and CREB messenger ribonucleic acid (mRNA) expressions in the spinal cord:
The spinal cord tissue was taken from each group of rats to extract the total ribonucleic acid (RNA) in the sample with TRIzol reagent. Next, the RNA was reversely transcribed into complementary deoxyribonucleic acid (cDNA) according to instructions of the reverse transcription kit, followed by real-time quantitative polymerase chain reaction (RT-qPCR) for amplification. 2−ΔΔCt was used to express the relative expression level of gene mRNA[13], with glyceraldehyde-3-phosphate dehydrogenase (GAPDH) as a reference. The sequences of the reaction primer were as follows:
GAPDH mRNA sense strand: 5'-CCCGGGTTTCAGAGACAACTTC-3', antisense strand: 5'-TCCACATGCTTTATTCCAGCAATC-3', ERK1 mRNA sense strand: 5'-CATGAGAGCCCTCACACTCCT-3', antisense strand: 5'-CACCTTTGCTGGACTCTGCAC-3' and CREB mRNA sense strand: 5'-TCACAGGTACAGGGATGAGGACAC-3', antisense strand: 5'-CAAAGCACAGCAATGTCCTGAAG-3'.
Expressions of p-ERK1 and p-CREB in the spinal cord:
The spinal cord tissue was taken from each group of rats and placed in the lysis buffer at 4° for 30 min. After centrifugation, the supernatant was diluted. The total protein was routinely extracted from the sample and loaded (50 μg). After electrophoresis, the sample was transferred and sealed. Subsequently, the sample was diluted with primary antibody (1:1000) and secondary antibody (1:5000), incubated at room temperature and treated with color development for 30 min. The gray value of the target protein was analyzed with GAPDH as a reference[14].
Statistical analysis:
SPSS 16.0 software was adopted for statistical analysis of experimental data and GraphPad Prism 8.0 was used for graphing. Data with normal distribution, such as interleukin-1β (IL-1β) and tumor necrosis factor alpha (TNFα) gene expression levels were expressed by mean±standard deviation (x?±s). Univariate analysis was used for comparison among multiple groups and t-test was employed for pairwise comparison, p<0.05 indicated that the difference was statistically significant.
Results and Discussion
During the experiment, the rats in normal group were in good mental state, reacted alertly, had smooth and shiny fur and had regular excretion. No obvious abnormality was observed in stool properties. The water and food intake increased steadily and the body mass increased rapidly. The rats in model group were in a poor mental state, slow to respond, preferred to gather together and lick the abdomen and had reduced activity. They were easily irritated and had dull fur, pale auricles, irregular excretion, loose stools around the anus and poor appetite. The increase in food intake and body weight was not obvious. The mental state of the rats in experimental group and control group was notably ameliorated, the flexibility of the fur of the rats was markedly improved, the frequency of licking the abdomen was obviously reduced and the loose stools around the anus was significantly alleviated.
The experimental results indicated that under 20 mmHg, 40 mmHg, 60 mmHg and 80 mmHg pressure levels, the AWR score was significantly higher in model group, experimental group and control group than that in normal group (p<0.05), while it was significantly lower in experimental group and control group than that in model group ??(p<0.05). There was no significant difference in the AWR score between experimental group and control group ??(p>0.05) (fig. 1).
The experimental results showed that the pain threshold value was significantly lower in model group, experimental group and control group than that in normal group (p<0.05), while it was significantly higher in experimental group and control group than that in model group (p<0.05). There was no significant difference in the pain threshold value between experimental group and control group (p>0.05) (fig. 2).
TUNEL results displayed that the cell apoptosis rate was significantly higher in model group, experimental group and control group than that in normal group (p<0.05), while it was significantly lower in experimental group and control group than that in model group (p<0.05). No significant difference was found in the cell apoptosis rate between experimental group and control group (p>0.05) (fig. 3).
The RT-qPCR results demonstrated that mRNA expressions of ERK1 and CREB were significantly higher in model group, experimental group and control group than those in normal group (p<0.05), while they were significantly lower in experimental group and control group than those in model group (p<0.05). There were no significant differences in the mRNA expressions of ERK1 and CREB between experimental group and control group (p>0.05) (fig. 4).
The Western blotting results revealed that p-ERK1 and p-CREB expressions were significantly higher in model group, experimental group and control group than those in normal group (p<0.05), while they were significantly lower in experimental group and control group than those in model group (p<0.05). P-ERK1 and p-CREB expressions had no significant differences between experimental group and control group (p>0.05) (fig. 5).
Epidemiological data have indicated that as people’s material and spiritual living standards improve, the incidence rate of IBS exhibits an increasing trend annually. The pathogenesis of such disease is complicated and its molecular mechanism has not yet been fully elucidated. Due to the lack of clinically effective drugs, the current treatment of this disease is mainly dominated by controlling the progression of clinical symptoms such as abdominal pain and diarrhea in patients[15]. With the development of minimally invasive surgery and digestive endoscopy diagnosis and treatment technology, laparoscopy and digestive endoscopy can be used to diagnose and treat many digestive tract diseases or even tumors, so the effective intervention for visceral noxious stimulation and visceral pain is also one of the issues that need more attention[16].
Dexmedetomidine, serving as a new analgesic and sedative drug, can protect central nervous system and effectively relieve pain[17]. Wu et al.[18] reported that dexmedetomidine could prominently reduce paw withdrawal mechanical threshold, regulate Ras-related C3 botulinumtoxin substrate 1 (Rac1) signal transduction in the spinal cord and block the progression of neuropathic pain in rats. Qin et al.[19] reported that in a rat model of spinal cord ischemia-reperfusion injury, dexmedetomidine could effectively reduce the oxidative stress response in the injured area and inhibit the apoptosis of rat central neurons, thus exerting central nervous protection effects. Xing et al.[20] reported that dexmedetomidine could notably alleviate postoperative pain in patients undergoing laparoscopic surgery. In this study, by establishing a rat IBS model and using clinical common drug pinaverium bromide as a control, it could be seen that the mental state of the rats in experimental group was notably ameliorated, the flexibility of the fur of the rats was markedly improved and the frequency of licking the abdomen was obviously reduced, indicating that dexmedetomidine can significantly ameliorate the clinical symptoms of IBS rats. Moreover, both AWR score and pain threshold value of rats were significantly ameliorated, suggesting that dexmedetomidine has a great analgesic effect.
In-depth explication of the therapeutic target of drugs is conducive to accurately controlling the therapeutic strategy of drugs and further revealing the molecular mechanism of the disease. The important regulatory role of the ERK1/CREB pathway in pain-related diseases has been well-documented[21]. ERK is phosphorylated into p-ERK1 under the action of physiological excitatory transmitters, which carries signals and undergoes nuclear translocation and converts downstream CREB into a pro-survival transcription factor (p-CREB), thus actively regulating the transcription, splicing and translation of related genes to intervene in neuronal cell apoptosis, proliferation, excitement and growth[22]. Torres-Perez et al.[23] reported that in a rat model of local scald on the paw, inhibiting the conduction of the ERK1/CREB pathway in the burn region could significantly ameliorate the pain of experimental animals. The results of RT-qPCR and Western blotting in the present study elucidated that mRNA expressions of ERK1 and CREB and p-ERK1 and p-CREB expressions in the spinal cord of experimental rats were significantly reduced, indicating that inhibiting the ERK1/CREB pathway may be a strategy for the drug to exert its effects.
In conclusion, dexmedetomidine can prominently ameliorate the clinical symptoms of rats with functional chronic visceral pain and may protect the colon and spinal cord by inhibiting the ERK1/CREB signaling pathway. However, patient’s physique and specificity of disease progression should be considered when dexmedetomidine is applied for the clinical treatment of IBS.
Conflicts of interest:
The authors declared no conflict of interest.
References
- Lacy BE, Pimentel M, Brenner DM, Chey WD, Keefer LA, Long MD, et al. ACG clinical guideline: management of irritable bowel syndrome. Am J Gastroenterol 2021;116(1):17-44.
- Aziz I, Simren M. The overlap between irritable bowel syndrome and organic gastrointestinal diseases. Lancet Gastroenterol Hepatol 2021;6(2):139-48.
- Zhuo BF, Zhang YQ, Ning XY. Effect of Tongxie Yao Fang combined with Sijunzi decoction on brain-gut peptide in irritable bowel syndrome patients with diarrhea type. J Nanjing Univ Tradit Chin Med 2019;35(1):25-8.
- Giummarra MJ, Simpson P, Gabbe BJ. Pain, anxiety and depression in the first two years following transport-related major trauma: a population-based, prospective registry cohort study. Pain Med 2020;21(2):291-307.
- Kim Y, Kwon SY, Jung HS, Park YJ, Kim YS, In JH, et al. Amitriptyline inhibits the MAPK/ERK and CREB pathways and proinflammatory cytokines through A3AR activation in rat neuropathic pain models. Korean J Anesthesiol 2019;72(1):60-7.
- Sun L, Zhou J, Sun C. MicroRNA-211-5p enhances analgesic effect of dexmedetomidine on inflammatory visceral pain in rats by suppressing ERK signaling. J Mol Neurosci 2019;68(1):19-28.
- Calhoun G, Wang L, Almeida LE, Kenyon N, Afsar N, Nouraie M, et al. Dexmedetomidine ameliorates nocifensive behavior in humanized sickle cell mice. Eur J Pharmacol 2015;754:125-33.
- Grabauskas G, Wu X, Gao J, Li JY, Turgeon DK, Owyang C. Prostaglandin E2, produced by mast cells in colon tissues from patients with irritable bowel syndrome, contributes to visceral hypersensitivity in mice. Gastroenterology 2020;158(8):2195-207.
- Yao JP, Zhao Y, Chen Y, Chen LP, Feng XM, Li Y, et al. Effect of electroacupuncture on intestinal epithelial mucosal barrier function in rats with diarrhea-predominant irritable bowel syndrome. Zhen Ci Yan Jiu 2020;45(5):357-62.
- Parisio C, Lucarini E, Micheli L, Toti A, Bellumori M, Cecchi L, et al. Extra virgin olive oil and related by-products (Olea europaea L.) as natural sources of phenolic compounds for abdominal pain relief in gastrointestinal disorders in rats. Food Funct 2020;11(12):10423-35.
- Lucarini E, Coppi E, Micheli L, Parisio C, Vona A, Cherchi F, et al. Acute visceral pain relief mediated by A3AR agonists in rats: Involvement of N-type voltage-gated calcium channels. Pain 2020;161(9):2179-90.
- Li W, Yao S, Li H, Meng Z, Sun X. Curcumin promotes functional recovery and inhibits neuronal apoptosis after spinal cord injury through the modulation of autophagy. J Spinal Cord Med 2021;44(1):37-45.
- Dong WT, Huang K, Song M, Zhou LT, Hou HY, Liu T, et al. Effect of Guben Zenggu Decoction on Expressions of Serum BALP and CaM, CaMK? mRNA in NEI Network of Ovariectomized Rats. Sichuan Da Xue Xue Bao Yi Xue Ban 2019;50(1):27-33.
- Song YF, Pei LX, Chen L, Geng H, Yuan MQ, Xu WL, et al. Electroacupuncture relieves irritable bowel syndrome by regulating IL-18 and gut microbial dysbiosis in a trinitrobenzene sulfonic acid-induced post-inflammatory animal model. Am J Chin Med 2020;48(1):77-90.
- Roberts A, Grafton G, Powell AD, Brock K, Chen C, Xie D, et al. CSTI-300 (SMP-100); a novel 5-HT3 receptor partial agonist with potential to treat patients with irritable bowel syndrome or carcinoid syndrome. J Pharmacol Exp Ther 2020;373(1):122-34.
- Chung HG, Min YW, Lee C, Hong SN, Won JY, Jang JA, et al. Effects of novel probiotics in a murine model of irritable bowel syndrome. Korean J Gastroenterol 2020;75(3):141-6.
- Liu Y, Liu W, Wang X, Wan Z, Liu Y, Leng Y. Dexmedetomidine relieves acute inflammatory visceral pain in rats through the ERK pathway, toll-like receptor signaling and TRPV1 channel. J Mol Neurosci 2018;66(2):279-90.
- Wu XX, Xing F, Lu XH. Role of spinal Rac1 signaling pathway in dexmedetomidine-induced reduction of neuropathic pain in rats. Chin J Anesthesiol 2020;40(9):1101-4.
- Qin Y, Yang G. Intrathecal injection of dexmedetomidine improves neuromotor function in rats with spinal cord ischemia-reperfusion injury based on the CXCR4-FAK signaling pathway. Chin J Comp Med 2020;30(4):77-85.
- Xing MY, Liang X, Guo QL, Zou WY. Intraperitoneal instillation of dexmedetomidine plus local anesthetic relieves the postoperative pain in laparoscopic surgery: a meta-analysis. J Clin Anesthesiol 2020;36(4):364-70.
- Shao S, Xia H, Hu M, Chen C, Fu J, Shi G, et al. Isotalatizidine, a C 19-diterpenoid alkaloid, attenuates chronic neuropathic pain through stimulating ERK/CREB signaling pathway-mediated microglial dynorphin A expression. J Neuroinflammation 2020;17(1):1-11.
- Jiang N, Wang H, Lv J, Wang Q, Lu C, Li Y, et al. Dammarane sapogenins attenuates stress-induced anxiety-like behaviors by upregulating ERK/CREB/BDNF pathways. Phytother Res 2020;34(10):2721-9.
- Nagy I, Torres-Perez JV, Adamek P, Palecek J, Vizcaychipi M, Varga A. The NAv1. 7 blocker protoxin II reduces burn injury-induced spinal nociceptive processing. J Mol Med 2018;96(1):75-84.