- *Corresponding Author:
- Zhong Xu
Department of Traumatology, Zibo Hospital of Traditional Chinese Medicine, Affiliated Hospital of Shandong University of Traditional Chinese Medicine, Zibo, Shandong Province 255090, China
E-mail: zhongqiansi2694@163.com
| This article was originally published in a special issue, “Transformative Discoveries in Biomedical and Pharmaceutical Research” |
| Indian J Pharm Sci 2023:85(4) Spl Issue “239-245” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
To compare the effectiveness and safety of traditional open reduction and internal fixation with intramedullary nailing in the treatment of humeral shaft fractures. Seventy-four patients with humeral shaft fractures admitted to our hospital between June 2017 and June 2022 were recruited and assigned (1:1) into a control group and a study group according to the surgical method they received. The patients in the control group were treated with the open reduction and internal fixation procedure and the patients in the study group were treated with the intramedullary nailing procedure. Patients in both groups received 10 w of post-operative medication and functional exercise as adjunctive therapy and were followed up for 1 y after discharge from hospital. The surgical efficacy, perioperative indexes, inflammatory factor indexes, pain stress indexes, functional recovery of the shoulder and elbow joint, and complications of the two groups were compared. The excellent surgical rate of the study group was significantly better than that of the control group (p<0.05); the operative time, intraoperative bleeding, incision length and fracture healing time of the study group were significantly lower than those of the control group (all p<0.05); the levels of tumor necrosis factor-alpha, interleukin-1 beta and interleukin-8 at 1 w after surgery of the study group were significantly lower than those of the control group (all p<0.05); the levels of substance P and neuropeptide Y levels were significantly lower in the study group than in the control group (all p<0.05); Neer scores and histopathology scoring system at 3 mo, 6 mo, 9 mo and 1 y after surgery were significantly higher in the study group than in the control group (all p<0.05); the incidence of postoperative complications was significantly lower in the study group than in the control group (p<0.05). Compared with the traditional open reduction and internal fixation procedure, the intramedullary nailing procedure is more effective and safer in the treatment of humeral shaft fractures. This procedure can effectively improve the perioperative indicators of patients, reduce the inflammation and pain stress response of patients, and thus promote the further recovery of the function of the shoulder and elbow joint.
Keywords
Incisional plate fixation, intramedullary nail fixation, humeral shaft fracture, effectiveness, safety
Humeral shaft fractures are a common traumatic fracture and they account for approximately 3 % of all fractures in the body[1]. Due to the special anatomical location of the radial nerve, these fractures are often associated with abnormal sensory function, which affects patients' health and daily life. Most humeral stem fractures can be cured by conservative treatment, but because of the long immobilization time and the severe functional limitations of the shoulder and elbow joints, they are prone to deformities in healing, and surgery is currently preferred[2].
There are many clinical procedures for the treatment of humeral shaft fractures, the relatively mainstream procedures include traditional Open Reduction and Internal Fixation (ORIF) and Intramedullary Nailing (IMN). The ORIF technique has been used in clinical practice for many years and has been shown in numerous studies to provide good fracture alignment and fixation[3,4], but some studies have shown that the incision and repositioning of the patient can disrupt the original environment of bone growth, thereby prolonging the healing time and increasing the risk of non-union[5]. In recent years, the IMN technique has been gradually applied in the treatment of humeral stem fractures. It uses closed reduction central fixation, which can effectively restore the upper limb force line and avoid damage to the soft tissue and biological environment of the fractured end of the patient[6]. This not only facilitates the healing of the fracture and reduces medically induced nerve damage, but it is also associated with postoperative complications of the shoulder and elbow joint[7]. The best surgical option for humeral shaft fractures is still controversial in clinical practice. The aim of this study was to compare the effectiveness and safety of the ORIF procedure with the IMN procedure in the treatment of humeral stem fractures.
Materials and Methods
Study design and participants:
Seventy-four patients with humeral shaft fractures admitted to our hospital between June 2017 and June 2022 were enrolled, and baseline data such as gender, age, fracture affected side, fracture cause and fracture Neer's typing were collected. The patients were assigned into a control group and a study group according to the surgical procedure they underwent, with 37 cases in each group.
Inclusion and exclusion criteria:
Inclusion criteria: All patients were diagnosed with humeral stem fractures by clinically relevant tests; all patients' fractures were new; all patients' fractures were closed; all patients had no significant vascular or nerve injuries; all patients and their families were informed and signed the relevant informed consent forms for this study.
Exclusion criteria: Patients with open fractures; patients with a previous history of related medical conditions or shoulder and elbow dysfunction; patients with fractures that have occurred for more than 14 d; patients with psychiatric or cognitive impairment; patients with combined systemic or immune diseases were excluded; patients with relevant allergic reactions or contraindications to the procedures and drugs used in this study were excluded; patients and family members who were unable to cooperate completely with this study for various reasons.
Methods:
Internal fixation: Patients in the control group were treated with internal fixation using an incisional repositioning plate, and the specific measures were as follows; after brachial plexus anesthesia, the patient was guided to a supine position and the anterolateral part of the patient's fracture line was used as the incision, entered through the biceps interval, exposed and separated the patient's radial nerve, appropriately stripped the periosteum and fracture end, followed by traction repositioning, and after the repositioning check was confirmed, an 8-10 hole locking joint plate was placed in the anterolateral part of the patient's humerus. After repositioning, an 8-10 hole locking plate is placed in the anterolateral humerus, followed by 4 locking screws on each side of the humeral fracture end and the incision is closed.
Interlocking IMN: Patients in the study group were treated with closed interlocking intramedullary nailing with the following measures; after brachial plexus anesthesia, the patient was guided to a seated beach chair position, a 5 cm long incision was made at the acromion, the rotator cuff was incised, a positioning pin was placed next to the patient's intertrochanteric sulcus, the posterior opening of the medullary cavity was determined by C-arm fluoroscopy, and the guide pin was placed according to the anatomical pattern after traction repositioning. After confirming that the guide pin is located in the medullary cavity, a suitable intramedullary nail is selected for entry, the intramedullary nail is removed, longitudinal pressure is applied and proximal locking of the nail is performed, and the incision is closed.
Postoperative medication: Patients in both groups received 10 w of postoperative medication and functional exercise as adjunctive therapy specifically. Patients in both groups received 10 w of albumin and alpha osteopontin after surgery. Procalcitonin 5 units/w; alfacalcidol 1 μg/d. After surgery, the patient was suspended in a triangular scarf and asked to bend the elbow at 90°. 3 d after surgery, the patient was instructed to perform basic functional exercises of the shoulder joint, mainly including passive abduction, posterior extension and forward flexion, etc. After 3 w, the patient was instructed to perform active activities of the shoulder joint, etc. After the fracture had healed, the patient was instructed to perform functional exercises against resistance.
Patients are discharged from the hospital for a 1 y follow-up observation period, which includes telephone follow-up and recall follow-up. The frequency of telephone follow-up was 1 mo/time, and the frequency of recall follow-up was 3 mo/time. During the follow-up period, the patients' recovery of shoulder and elbow function, and the occurrence of complications were recorded.
Outcomes:
Surgical efficacy: Post-operative review showed complete healing of the fracture end and anatomical alignment which was excellent; post-operative review showed that the angle of the fracture end was less than 10° and that the fracture end was misaligned but not more than 5 mm which was good; post-operative review showed that the angle of the fracture end was less than 15° and that the fracture end was misaligned but not more than 1 cm which was poor.
Perioperative indices: The patients' perioperative indicators (operating time, intraoperative bleeding, incision length and fracture healing time) were counted by the relevant medical and nursing staff of our hospital.
Inflammatory factors indices: 3 ml of fasting venous blood was drawn from patients before and 1 w after surgery, the fluid was routinely centrifuged and sent for examination. The levels of Tumor Necrosis Factor-Alpha (TNF-α), Interleukin-1 Beta (IL-1β) and IL-8 were measured by Enzyme-Linked Immunosorbent Assay (ELISA).
Pain stress indices: 3 ml of fasting venous blood was taken from the patients before and 1 w after surgery, and the fluid was routinely centrifuged and sent for examination. The levels of Substance P (SP) and Neuropeptide Y (NPY) were measured by automatic biochemical analyzer.
Functional recovery of the shoulder and elbow joint: The Neer score and Histopathology Scoring System (HSS) score were used to assess the functional recovery of the patient's shoulder and elbow joint before at 3 mo, 6 mo, 9 mo and 1 y postoperatively. The Neer score is used to assess shoulder function and the HSS score is used to assess elbow function. Both the Neer score and the HSS score have a full score of 100, with higher scores indicating better recovery of the corresponding joint function.
Complications: The complications included in this study and development includes; shoulder stiffness, incisional infection, non-healing fracture and radial nerve injury.
Statistical analysis:
Statistical Package for the Social Sciences (SPSS) 25.0 was used to analyze the data. The measurement data are expressed using (x±s) and compared using t-test; the count data are expressed using n (%) and compared using Chi-square (χ²) test. p<0.05 indicates that the comparison is statistically significant. GraphPad Prism 8 was used as the graphing software.
Results and Discussion
In the control group, there were 22 males and 15 females, aged 23-60 y, with an average age of (39.28±7.31) y; fracture side has 25 on the left side and 12 on the right side; fracture causes has 12 smash injuries, 10 fall injuries and 15 traffic accident injuries; fracture Neer type has 7 in two parts, 22 in three parts and 8 in four parts. In the study group, there were 24 males and 13 females; age 22-58 y, mean age (39.62±7.27) y; fracture side has 28 on the left side, 9 on the right side; fracture causes has 14 cases of smash, 9 cases of fall, 14 cases of traffic accident; fracture Neer type has 8 cases of two parts, 20 cases of three parts and 9 cases of four parts. The general data of the two groups of patients were comparable and their comparisons were not significantly different (p>0.05) as shown in Table 1.
| Control group (n=37) | Study group (n=37) | t/χ² | p | |
|---|---|---|---|---|
| Gender | 0.23 | 0.632 | ||
| Male | 22 | 24 | ||
| Female | 15 | 13 | ||
| Age (year) | 39.28±7.31 | 39.62±7.27 | -0.201 | 0.841 |
| Fracture side | 0.598 | 0.439 | ||
| Left | 25 | 28 | ||
| Right | 12 | 9 | ||
| Causes of fractures | ||||
| Smash injury | 12 | 14 | 0.237 | 0.626 |
| Falling injury | 10 | 9 | 0.071 | 0.79 |
| Traffic accident injury | 15 | 14 | 0.057 | 0.812 |
| Neer type | ||||
| Two parts | 7 | 8 | 0.084 | 0.772 |
| Three parts | 22 | 20 | 0.22 | 0.639 |
| Four parts | 8 | 9 | 0.076 | 0.782 |
Table 1: Baseline Characteristics.
The excellent surgical rate in the control group was 78.38 % (29/37), of which 7 cases were excellent, 22 cases were good and 8 cases were poor; the excellent surgical rate in the study group was 94.59 % (35/37), of which 12 cases were excellent, 23 cases were good and 2 cases were poor. The excellent surgical rate of the study group was significantly better than that of the control group (p<0.05) as shown in Table 2.
| Group | n | Excellent | Good | Poor | Excellent and good rate |
|---|---|---|---|---|---|
| Control | 37 | 7 | 22 | 8 | 78.38 % (29/37) |
| Study | 37 | 12 | 23 | 2 | 94.59 % (35/37) |
| χ² | 4.162 | ||||
| p | 0.041 |
Table 2: Comparison of surgical outcomes [n (%)].
The operative time, intraoperative bleeding, incision length and fracture healing time in the study group were significantly lower than those in the control group (all p<0.05) as shown in Table 3.
| Control group (n=37) | Study group (n=37) | t | p | |
|---|---|---|---|---|
| Surgery time (min) | 91.32±10.17 | 84.15±7.69 | 3.421 | 0.001 |
| Intraoperative bleeding (ml) | 115.77±15.29 | 89.54±7.26 | 9.426 | <0.001 |
| Incision length (cm) | 12.32±2.39 | 5.21±1.17 | 5.21±1.17 | <0.001 |
| Fracture healing time (weeks) | 12.14±1.89 | 8.76±2.11 | 7.258 | <0.001 |
Table 3: Comparison of perioperative indicators (x̄±s).
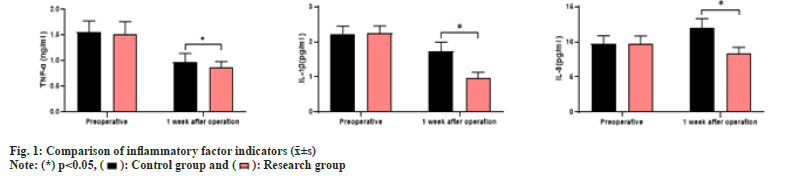
As shown in fig. 1, the preoperative and 1 w postoperative TNF-α in the control group were (1.56±0.21, 0.97±0.17), IL-1β were (2.23±0.22, 1.74±0.25) and IL-8 were (9.77±1.12, 12.07±1.25) respectively; the preoperative and 1-week postoperative TNF-α in the study group were (1.52±0.24, 0.86±0.12), IL-1β (2.25±0.21, 0.95±0.18) and IL-8 (9.75±1.10, 8.28±0.98) respectively in the study group. The preoperative levels of TNF-α, IL-1β and IL-8 in the two groups were compared (all p>0.05); the levels of TNF-α, IL-1β and IL-8 in the study group were significantly lower than those in the control group 1 w after surgery (all p<0.05).
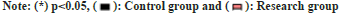
As shown in fig. 2, the SP before and 1 w after surgery in the control group were (3.04±0.28, 7.68±0.89) and NPY were (152.32±12.39, 195.31±3.16) respectively; the SP before and 1 w after surgery in the study group were (3.07±0.31, 5.17±0.38) and NPY were (151.87±12.65, 171.68±6.11). The preoperative SP and NPY levels of the two groups were compared (all, p>0.05); the SP and NPY levels of the study group at 1 w postoperatively were significantly lower than those of the control group (all p<0.05).
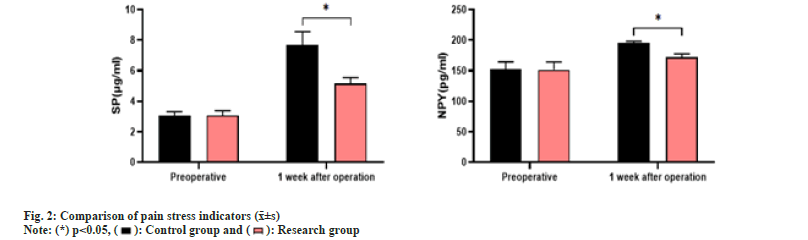
As shown in fig. 3, the Neer scores of the control group before surgery, at 3 mo, 6 mo and 9 mo and at 1 y were (62.36±5.23, 71.39±5.19, 77.85±5.26, 84.62±5.33 and 90.37±5.27) and the HSS scores were (68.75±5.16, 73.25±4.78, 78.26± 5.10, 83.89±4.94 and 88.39±5.17). The Neer scores of the study group at preoperative, 3 mo, 6 mo and 9 mo and at 1 y were (62.54±5.13, 75.46±5.87, 82.96±5.37, 90.48±5.29 and 94.15±4.11) and HSS scores (68.42±5.31, 78.36±4.85, 84.75±4.62, respectively) before and after surgery and at 88.68±4.46, 93.13±5.29). The preoperative Neer scores and HSS scores of the two groups were compared (all p>0.05); the Neer scores and HSS scores of the study group were significantly higher than those of the control group at 3 mo, 6 mo, 9 mo and at 1 y after surgery (all p<0.05).
In the control group, the complication rate was 24.32 % (9/37), including 1 case of shoulder stiffness, 2 cases of incision infection, 0 cases of non-healing fracture and 6 cases of radial nerve injury. In the study group, the complication rate was 5.41 % (2/37), including 1 case of shoulder stiffness, 1 case of incision infection, 0 cases of non-healing fracture and 0 cases of radial nerve injury. The incidence of postoperative complications in the study group was significantly lower than that in the control group (p<0.05) as shown in Table 4.
| Control group (n=37) | Study group (n=37) | χ² | p | |
|---|---|---|---|---|
| Stiffness of the shoulder joint | 1 | 1 | - | - |
| Infection of the Incision | 2 | 1 | - | - |
| Nonunion | 0 | 0 | - | - |
| Radial nerve injury | 6 | 0 | - | - |
| Total incidence (%) | 24.32 % (9/37) | 5.41 % (2/37) | 5.232 | 0.022 |
Table 4: Comparison of complications [n (%)].
Previous studies have concluded that conservative treatment modalities are the preferred choice for treating patients with humeral shaft fractures[8]. Conservative treatment effectively avoids the trauma caused to the patient by surgery and the relatively low cost of this modality is key to the high acceptance by the patient population. However, conservative treatment resulted in a non-healing rate of 21 % for humeral fractures, and that the greater degree of displacement and more complex muscle attachments in the humeral region than in other parts of the body, coupled with the fact that most patients with humeral stem fractures have vascular and nerve injuries, have been associated with lower satisfaction[9,10]. The traditional ORIF procedure is the most widely used procedure for the treatment of humeral stem fractures, and has been clinically accepted for its ideal biological properties[11]. However, some studies have shown that the ORIF procedure has a large field, which can lead to excessive exposure of the patient's tissues and can aggravate soft tissue injuries, etc.,[12]. Additionally, the ORIF procedure requires stripping the patient's periosteum, which can affect the blood supply to the fracture end and prolong the healing time[13].
The IMN technique is a minimally invasive technique that is now commonly used in clinical practice due to the shortcomings of the ORIF technique, which has better biological properties, does not cause stress masking and does not affect the blood supply to the fracture end during the repositioning and fixation process, which significantly reduces the healing time and facilitates the patient's ability to start functional exercise as soon as possible[14]. This significantly shortens the healing time of the fracture and allows the patient to start functional exercises as soon as possible[14]. A prior study stated that the treatment of humeral shaft fractures is comprehensive and postoperative pharmacological interventions and rehabilitation exercises should not be neglected[15]. Therefore, in this study, a 10 w adjuvant treatment of medication and functional exercise was administered to the patients. Calcitonin and alfacalcidol are both commonly used as adjuncts to fracture healing, and their use promotes bone synthesis and accelerates fracture healing[16]. Functional exercise is the key to the patient's subsequent rehabilitation and prevention of further fracture damage[17].
In this study, the surgical outcomes, perioperative parameters and complication rates of the patients in the study group were significantly better than those of the control group, which is consistent with the results of previous studies[18,19]. These results confirm that the IMN procedure is more effective and safer than the traditional ORIF procedure and that the use of the IMN procedure can effectively improve the perioperative parameters of patients. Studies showed that the inflammatory response and pain stress caused by postoperative trauma in fracture patients would have a certain impact on their own fracture healing[20]. In this study, the levels of TNF-α, IL-1β and IL-8 in the study group were significantly lower than those in the control group 1 w after surgery; the levels of SP and NPY in the study group were significantly lower than those in the control group 1 w after surgery. These suggest that the IMN procedure not only has a lower degree of activation of the postoperative inflammatory response, but also has less impact on the pain stress response of the patients. In this study, patients were followed up for 1 y after surgery, and the aim was to observe the differences in the recovery of shoulder and elbow joint function between the two groups. In this study, the Neer scores and HSS scores of the study group were significantly higher than those of the control group at 3 mo, 6 mo, 9 mo and 1 y after surgery, and this result was different from the results of Amer et al.[21], in which patients treated with the ORIF procedure, which yielded superior postoperative shoulder function recovery to those treated with the IMN procedure. The possible explanation may be related to the different observation indexes and assessment criteria, etc. Therefore, the advantages and disadvantages of the ORIF procedure and the IMN procedure for postoperative shoulder and elbow function recovery in patients with humeral stem fractures still need further clinical investigation.
In conclusion, the IMN procedure is more effective and safer than the traditional ORIF procedure in the treatment of humeral shaft fractures. This procedure can effectively improve the patient's perioperative indicators, reduce the patient's inflammation and pain stress response, and thus promote the further recovery of the patient's shoulder and elbow joint function.
Conflict of interests:
The authors declared no conflict of interests.
References
- Updegrove GF, Mourad W, Abboud JA. Humeral shaft fractures. J Shoulder Elbow Surg 2018;27(4):e87-97.
- Baertl S, Alt V, Rupp M. Surgical enhancement of fracture healing–operative vs. nonoperative treatment. Injury 2021;52(2):S12-7.
[Crossref] [Google Scholar] [PubMed]
- Beeres FJ, Diwersi N, Houwert MR, Link BC, Heng M, Knobe M, et al. ORIF vs. MIPO for humeral shaft fractures: A meta-analysis and systematic review of randomized clinical trials and observational studies. Injury 2021;52(4):653-63.
[Crossref] [Google Scholar] [PubMed]
- Hosseini Khameneh SM, Abbasian M, Abrishamkarzadeh H, Bagheri S, Abdollahimajd F, Safdari F, et al. Humeral shaft fracture: A randomized controlled trial of nonoperative vs. operative management (plate fixation). Orthopedic Res Rev 2019;11:141-7.
[Crossref] [Google Scholar] [PubMed]
- Stephens AR, Presson AP, Zhang C, Orleans B, Martin M, Tyser AR, et al. Comparison of direct surgical cost for humeral shaft fracture fixation: Open reduction internal fixation vs. intramedullary nailing. JSES Int 2021;5(4):734-8.
[Crossref] [Google Scholar] [PubMed]
- Wang Y, Kayastha Y, Cao Y, Guo Z, Yuan Y, Bi Y. Outcome of humeral shaft fracture treated with intramedullary nail and plate fixation. J Coll Physicians Surg Pak 2020;30(1):73-8.
[Google Scholar] [PubMed]
- Gottschalk MB, Carpenter W, Hiza E, Reisman W, Roberson J. Humeral shaft fracture fixation: Incidence rates and complications as reported by American board of orthopaedic surgery part II candidates. J Bone Joint Surg Am 2016;98(17):e71.
[Crossref] [Google Scholar] [PubMed]
- Ekegren CL, Edwards ER, de Steiger R, Gabbe BJ. Incidence, costs and predictors of non-union, delayed union and mal-union following long bone fracture. Int J Environ Res Public Health 2018;15(12):2845.
[Crossref] [Google Scholar] [PubMed]
- Dekker AP, Chuttha S, Tambe AA, Clark DI. Predicting the behavior of humeral shaft fractures: An independent validation study of the radiographic union score for humeral fractures and value of assessing fracture mobility. J Orthop Trauma 2021;35(10):555-9.
[Crossref] [Google Scholar] [PubMed]
- Pollock FH, Maurer JP, Sop A, Callegai J, Broce M, Kali M, et al. Humeral shaft fracture healing rates in older patients. Orthopedics 2020;43(3):168-72.
[Crossref] [Google Scholar] [PubMed]
- Yang J, Liu D, Zhang L, Lu Z, Liu T, Tao C. Treatment of humeral shaft fractures: A new minimally-invasive plate osteosynthesis vs. open reduction and internal fixation: A case control study. BMC Surg 2021;21(1):349.
[Crossref] [Google Scholar] [PubMed]
- Oliver WM, Carter TH, Graham C, White TO, Clement ND, Duckworth AD, et al. A prospective randomised controlled trial of operative vs. non-operative management of fractures of the humeral diaphysis: The humeral shaft fracture fixation (HU-FIX) study protocol. Trials 2019;20(1):475.
[Crossref] [Google Scholar] [PubMed]
- Esmailiejah AA, Abbasian MR, Safdari F, Ashoori K. Treatment of humeral shaft fractures: Minimally invasive plate osteosynthesis vs. open reduction and internal fixation. Trauma Monthly 2015;20(3):e26271.
[Google Scholar] [PubMed]
- Metsemakers WJ, Wijnen V, Sermon A, Vanderschot P, Nijs S. Intramedullary nailing of humeral shaft fractures: Failure analysis of a single centre series. Arch Orthop Trauma Surg 2015;135(10):1391-9.
[Crossref] [Google Scholar] [PubMed]
- Oliver WM, Searle HK, Ng ZH, Molyneux SG, White TO, Clement ND, et al. Factors associated with humeral shaft nonunion. J Shoulder Elbow Surg 2021;30(10):2283-95.
[Crossref] [Google Scholar] [PubMed]
- Paavolainen P, Taivainen T, Michelsson JE, Lalla M, Penttinen R. Calcitonin and fracture healing: An experimental study on rats. J Orthop Res 1989;7(1):100-6.
- Tang HC, Xiang M, Chen H, Hu XC, Yang GY. Manipulative reduction and small splint fixation combined with micromovement exercise for treatment of humeral shaft fractures. Zhongguo Gu Shang 2016;29(1):82-6.
[Google Scholar] [PubMed]
- Hu Y, Wu T, Li B, Huang Y, Huang C, Luo Y. Efficacy and safety evaluation of intramedullary nail and locking compression plate in the treatment of humeral shaft fractures: A systematic review and meta-analysis. Comput Math Methods Med 2022;2022.
[Crossref] [Google Scholar] [PubMed]
- Davies G, Yeo G, Meta M, Miller D, Hohmann E, Tetsworth K. Case-match controlled comparison of minimally invasive plate osteosynthesis and intramedullary nailing for the stabilization of humeral shaft fractures. J Orthop Trauma 2016;30(11):612-7.
[Crossref] [Google Scholar] [PubMed]
- Lode I, Nordviste V, Erichsen JL, Schmal H, Viberg B. Operative vs. nonoperative treatment of humeral shaft fractures: A systematic review and meta-analysis. J Shoulder Elbow Surg 2020;29(12):2495-504.
[Crossref] [Google Scholar] [PubMed]
- Amer KM, Kurland AM, Smith B, Abdo Z, Amer R, Vosbikian MM, et al. Intramedullary nailing vs. plate fixation for humeral shaft fractures: A systematic review and meta-analysis. Arch Bone Joint Surg 2022;10(8):661.
[Crossref] [Google Scholar] [PubMed]
 .
.
 .
.
 .
.



