- *Corresponding Author:
- Y. Jin
Emergency Department, Tongde Hospital of Zhejiang Province, Hangzhou, Zhejiang 310012, China
E-mail: zhangjin_740@126.com
| This article was originally published in a special issue, “Modern Applications in Biomedical Research and Pharmaceutical Sciences” |
| Indian J Pharm Sci 2022:84(3) Spl Issue “207-212” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
To investigate the effect of post-ischemic adaptation on myocardial perfusion injury in patients with ST segment elevation myocardial infarction by percutaneous coronary intervention. 80 patients were selected and divided into observation group (receiving treatment, 46 cases) and control group (without treatment, a total of 34 cases) and then two groups of patients were compared with serum free oxygen radicals (lipid peroxide, nitric oxide, hydroxyl), detection of stress (superoxide dismutase, glutathione peroxidase, malondialdehyde products, advanced oxidation protein products, major adverse cardiac events) difference rate and follow-up period of myocardial reperfusion injury after operation. Compared with before treatment, the two groups of patients after 8 h, nitric oxide, hydroxyl, lipid peroxide at superoxide dismutase and advanced oxidation protein products decreased, glutathione peroxidase and malondialdehyde increased, were statistically significant (all p<0.05); 8 h after the operation time, the observation group lipid peroxide, nitric oxide, hydroxyl, superoxide dismutase, advanced oxidation protein products were lower than the control group, glutathione peroxidase malondialdehyde were higher than that of control group, were statistically significant (all p<0.05); the control group of patients after reperfusion injury incidence rate (17.65 %) was significantly higher than the observation group (6.52 %), comparison between groups was statistically significant (χ2=1.117, p<0.05); the incidence of major adverse cardiovascular events of control group during the follow-up period were 64.71 % which was significantly higher than that of observation group (36.96 %), the difference was statistically significant (p<0.05). Ischemic post conditioning can significantly improve the detection of oxygen free radicals and related stress products in patients with ST segment elevation myocardial infarction after percutaneous coronary intervention treatment, reduce the postoperative reperfusion injury and improve the prognosis of patients.
Keywords
Ischemic post conditioning, myocardial perfusion injury, percutaneous coronary intervention, ST segment elevation myocardial infarction
Acute ST-Segment Elevation Myocardial Infarction (STEMI) is one of the most common critical diseases of the cardiovascular system in clinical practice. It is a serious threat to human health with a high risk of disability and death[1]. STEMI is an ischaemic myocardial infarction due to persistent or complete occlusion of a coronary vessel, resulting in inadequate or interrupted blood supply to the coronary arteries. Therefore, national treatment guidelines recommend reperfusion therapy in the early stages of STEMI[2]. Thrombolytic therapy and Percutaneous Coronary In3tervention (PCI) can open the Infarct-Related Artery (IRA) to greatly improve the clinical prognosis of STEMI patients[3]. Although appropriate PCI therapy is important in improving myocardial cell injury and reducing myocardial cell necrosis, ischemia-reperfusion operations can also cause myocardial cell loss[4]. Therefore, how to reduce ischemia-reperfusion injury during PCI has become an important area of clinical research in the treatment of STEMI. Studies have shown that ischaemic clinical preadaptation can be effective in protecting cardiomyocytes and preventing ischaemic reperfusion injury in patients with STEMI[5], but clinical application criteria and implementation are difficult due to the fact that ischaemic clinical preadaptation management needs to be applied before myocardial infarction, which remains unpredictable[6]. Post-ischaemic adaptation management has received considerable attention in recent years and several studies have confirmed its feasibility for application in patients with myocardial infarction[7]. However, no clinical reports have been seen in the acute PCI treatment of patients with STEMI. Hence, this study investigated the effect of post-ischaemic adaptation management on myocardial perfusion injury in patients with acute PCI for STEMI by retrospectively analysing the STEMI cases admitted to our hospital.
Materials and Methods
Study subjects:
Patients with STEMI treated with acute PCI between January 2019 and December 2020 were used for retrospective analysis.
Inclusion criteria: Complete medical records and a signed informed consent for the study; meeting the diagnostic criteria of the “Chinese guidelines for the diagnosis and treatment of acute STEMI”[8]; onset <12 h and no angina attack within 48 h before infarction; preoperative coronary angiographic findings of occlusive lesions and Thrombolysis in Myocardial Infarction (TIMI) grade 0 coronary flow; no collateral circulation in the infarcted area.
Exclusion criteria: Patients with non-acute STEMI; patients who have undergone thrombolytic therapy before the procedure; patients with old myocardial infarction, history of PCI therapy, coronary artery bypass graft; patients with chronic cardiac insufficiency and cardiac dysfunction; patients with heavy thrombus load in the IRA, where thrombus aspiration is applied; IRAs with left main lesions or other coronary occlusions combined with severe left main stenosis; IRAs with TIMI flow of grade 2 or higher at first imaging or IRAs with grade 2 or higher collateral circulation; lesions with anatomical structures unsuitable for PCI (e.g. including severe left main lesions, severe 3-vessel lesions, severe calcifications, tortuous lesions, etc.); patients who require interventional treatment of other non-IRA vessels for secondary PCI. A total of 80 patients were included in the study according to the above criteria, including 43 male patients and 37 female patients. Clinical information such as age, gender, hypertension rate, diabetes rate and hyperlipidaemia rate of the patients were recorded. Patients were aged 46-83 y with a mean age of (63.23±9.52) y, who all had left main stem lesions with stent placement implantation at preoperative TIMI grade 0. The patients were divided into an observation group (treated, 46 cases) and a control group (untreated, 34 cases) based on whether or not they received post-ischaemic adaptation treatment in accordance with their medical records.
Treatment for post-ischaemic management:
Patients and families were informed of the risks of surgery before operation in both groups. Patients were given a loading dose of clopidogrel (300 mg), aspirin (300 mg) and atorvastatin calcium (80 mg) in sequence prior to surgery. Patients were routinely punctured by the right radial artery, but in the case of a positive Allen test, a radial artery malformation, or a subclavian artery variant, the femoral artery was performed. After that, the patient’s coronary lesion count and IRA were determined from the imaging results and Electrocardiogram (ECG). Then, PCI was performed with reference to the relevant procedures in the American College of Cardiology Foundation’s “Guidelines for Percutaneous Coronary Intervention”[9]. In the observation group, the blood flow was blocked with a 4-6 atm low-pressure filling balloon for 30 s before reperfusion for 1 min and then the air was released to open the blood flow for 1 min. The procedure was repeated 3 times. The control group was not treated with any post-ischaemic treatment (excluding conventional treatments such as medication, defibrillation and electrical resuscitation) within 6 min of reperfusion. After successful PCI (TIMI of grade 3 for distal IRA flow, residual stenosis of no more than 20 %, no serious postoperative complications), conventional subcutaneous treatment with low molecular heparin (5000 U/dose, 1 time/12 h for 5-7 d), aspirin orally (100 mg/d for 5-7 d) and clopidogrel (75 mg/d for 5-7 d) was given clinically. Also, angiotensin-converting enzyme inhibitors or statins were given according to the principles of coronary heart disease prophylaxis. The follow-up visits were conducted at 3 mo after the surgery.
10The criteria for determining ischaemic reperfusion injury[10] are the presence of acute bradycardia, hypotension, frequent ventricular prematurity or severe ventricular arrhythmias in the patient 8h postoperatively. Besides, Myocardial Ischemia Reperfusion Injury (MIRI) angiography shows thrombosis or embolism of tissues and organs (heart, kidney, brain, etc.).
Detection of oxygen free radicals and related stress products:
2 ml of venous blood was taken from the patients before and 8 h after the treatment, packed into test tubes and centrifuged at 3000 rpm for 5 min using a tabletop centrifuge. The upper layer of serum was pipetted and stored in test tubes at low temperature (-20°) then sent to the laboratory for serum oxygen radical related assays in strict accordance with Enzyme- Linked Immunosorbent Assay (ELISA). The activity of Lipid Peroxide (LPO), Nitric oxide free radicals (NO) and Hydroxyl radicals (OH) was measured by a free radical test kit (manufacturer: Shanghai Hengyuan Biotechnology; batch number: HZ20138E). The human Malondialdehyde (MDA) ELISA kit (manufacturer: Shanghai Hengyuan Biotechnology; batch number: HY20105E), human Superoxide Dismutase (SOD) ELISA kit (manufacturer: Shanghai Hengyuan Biotechnology; batch number: HY21060E), human Glutathione Peroxidase (GSH-Px) ELISA kit (manufacturer: Shanghai Hengyuan Biotechnology; batch number: HY20369E) and human Advanced Oxidation Protein Products (AOPP) ELISA kits (manufacturer: Shanghai Hengyuan Biotechnology; batch number: HY20133E) were used to detect serum MDA, SOD, GSH-Px, AOPP respectively.
Occurrence of Major Adverse Cardiac Events (MACE) during the follow-up period:
The occurrence of MACE such as cardiac death, unstable angina, non-fatal infarction and non-fatal heart rate was recorded for patients during the 3 mo follow- up treatment period.
Statistical analysis:
The data were counted using Statistical Package for the Social Sciences (SPSS) 20.0 software and the measures were expressed as meanStandard Deviation (SD). The differences within groups were analysed by paired t-test and the differences between groups were analysed by two independent t-tests. The categorical data were characterized by number of cases and percentages and the differences between groups were analyzed by the χ2 test. p<0.05 indicated that the differences were statistically significant.
Results and Discussion
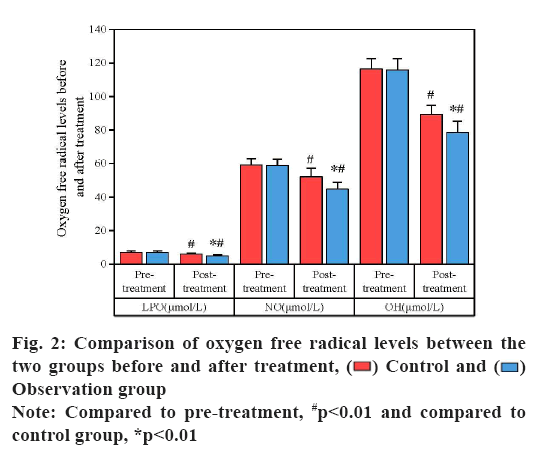
Comparison of clinical demographic and baseline information between the two groups of patients were as follows. There was no statistically significant difference (p>0.05) between the control and observation groups in terms of age, gender, hypertension rate, diabetes rate and hyperlipidaemia rate, etc. The data was shown in fig. 1.
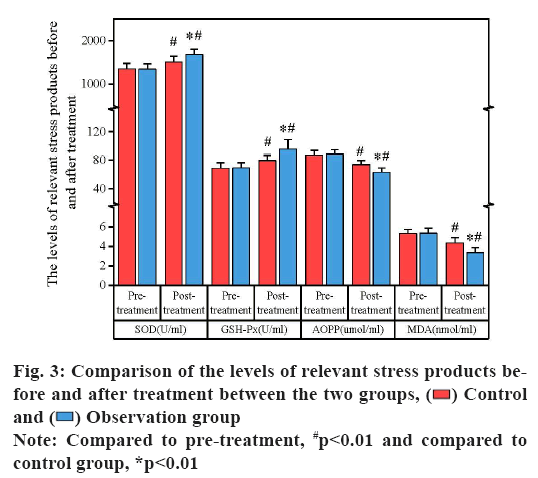
Comparison of oxygen free radical levels between the two groups before and after treatment was as follows. The expression of LPO, NO and OH in the serum of both groups were not statistically significant when compared before treatment (p>0.05). The expression of LPO and OH in serum was significantly lower while NO was significantly higher (p<0.01) in both groups at 8 h postoperatively compared to pre-treatment. The expression of LPO and OH in the observation group was significantly lower while NO was higher than that in the control group at 8 h postoperatively (p<0.01), as shown in fig. 2.
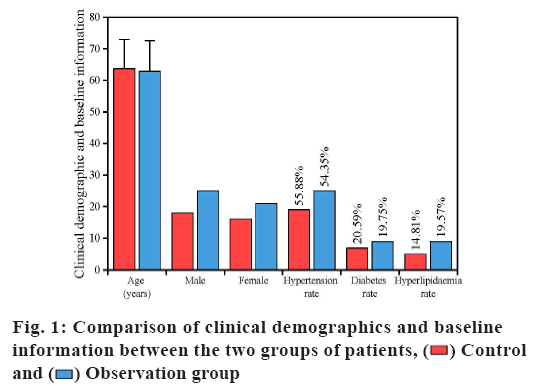
Comparison of the levels of relevant stress products before and after treatment between the two groups is explained below. The serum levels of SOD, GSH-Px, MDA and AOPP in both groups were not statistically significant, compared to before treatment (p>0.05). The expression of MDA and AOPP in the serum was reduced and GSH-Px and SOD were increased in both groups at the 8 h postoperative moment compared to the pre-treatment period (p<0.01). At the 8 h postoperative moment, MDA and AOPP in the observation group were lower and GSH-Px and SOD were higher than those in the control group (p<0.01), as shown in fig. 3.
Comparison of the incidence of postoperative ischemic reperfusion injury between the two groups is shown below. In the control group, reperfusion injury occurred in 9 cases after surgery, with an incidence of 26.47 %, while, reperfusion injury occurred in 3 cases after surgery in the observation group with an incidence of 6.52 %. The comparison between the groups was statistically significant (χ2=6.102, p<0.05) (Table 1).
| Group | Number of occurrences | Incidence (%) | χ2 | p |
|---|---|---|---|---|
| Control (n=34) | 9 | 26.47 | 6.102 | 0.014 |
| Observation group (n=46) | 3 | 6.52 |
Table 1: Comparison of the Incidence of Postoperative Reperfusion Injury between the Two Groups of Patients
Comparison of the occurrence of MACE between the two groups of patients during the follow-up period is described below. Postoperative follow-up revealed 1 case of cardiac death, 9 cases of unstable angina, 6 cases of non-fatal infarction and 6 cases of non-fatal heart in the control group of 34 patients. Of the 46 patients in the observation group, there were no cardiac deaths, 3 cases of unstable angina, 1 case of non-fatal infarction and 2 cases of non-fatal heart. There were 22 cases (64.71 %) of MACE in the control group and 17 cases (36.96 %) of MACE in the observation group during the follow-up period, with statistically significant differences (χ2=6.025, p<0.05), as shown in Table 2. This result confirms the good prognosis of STEMI patients treated with acute PCI after post- ischaemic adaptation management.
| Group | Number of MACE cases | Incidence | χ2 | p |
|---|---|---|---|---|
| Control (n=34) | 22 | 64.71 | 6.025 | 0.014 |
| Observation group (n=46) | 17 | 36.96 |
Table 2: Comparison of the Occurrence of Mace Between the Two Groups of PATIENTS During the follow-up Period
In recent years, ischaemic reperfusion methods such as thrombolysis and PCI have been used extensively in the clinical management of cardiovascular diseases, saving the lives of numerous patients with ischaemic myocardial infarction, however, PCI itself has the disadvantage of myocardial cell damage, leading to the limited use of PCI in the treatment of STEMI[11]. Post-ischaemic adaptation is a defense mechanism that occurs in the body in response to ischaemia which has been a hot topic of research in recent years in the clinical application of PCI for the treatment of cardiovascular disease. Post-ischaemic adaptation can improve the ischaemic tolerance of myocardial cells in patients with myocardial infarction in a short period of time, which can effectively defend patients against myocardial cell damage from myocardial infarction[12]. Since Thuny et al.[13] first introduced the concept of post-ischaemic adaptation management at the turn of the century, this process of opening the vessel less frequently and briefly before prolonged reperfusion of the vessel from the onset of myocardial ischaemia has gained importance in clinical research. Clinical studies have shown that post-ischaemic adaptation treatment has the ability to transiently restore coronary blood flow, enhance myocardial tolerance to prolonged ischaemia, reduce myocardial infarct size, decrease myocardial apoptosis, improve myocardial cell endothelial function and alleviate tissue oedema, thereby reducing reperfusion injury in ischaemic patients[14].
LPO is one of the main reactive oxygen radicals that cause damage to the body and its high expression not only leads to a decrease in the fluidity of cell membranes in tissues and organs, but also reduces the solubility of serum proteins, nucleic acids and enzymes, which are important factors in inducing apoptosis in cardiomyocytes to produce oxidative stress in the body[15]. OH is also one of the most aggressive oxygen radicals that can attack many molecules in the body[16]. OH mainly causes systolic dysfunction that can induce injury in isolated rabbit myocardium[17]. In contrast, NO is mainly produced by endothelial Nitric Oxide Synthase (eNOS), which acts as an important vasodilator with protective effects on the heart. Bai et al.[18] demonstrated that baicalin could promote NO production by microvascular endothelial cells through activation of the Phosphatidylinositol 3-Kinase (PI3K)- Protein kinase B (Akt)-eNOS pathway to reduce MIRI. In the present study, we also confirmed the relevant results. Compared to the pre-treatment period, LPO and OH were lower and NO were higher in the serum of STEMI patients at the 8 h post-PCI moment. Also, LPO and OH were significantly lower and NO were higher in patients undergoing post-ischaemic adaptation than in the control group at the 8 h post-procedure moment. These results suggest that adaptive preconditioning can effectively reduce the levels of LPO and OH reactive oxygen radicals and increase the levels of NO in patients, thus acting as a preventive measure against ischaemic reperfusion injury.
MDA is a pro-oxidant enzyme in the body that disproportionates hydrogen oxide and water into LPOs that promote the production of oxygen radicals. In contrast, SOD is an antioxidant enzyme in the body, which, under normal conditions, converts LPOs into hydrogen oxide and water, acting as a scavenger of oxygen free radicals[19]. Therefore, MDA and SOD can be used as indicators of the body’s ability to scavenge oxygen radicals in patients with myocardial injury. AOPP is a bis-tyrosine, a product of the oxidation of serum albumin by reactive free radicals, whose levels are closely related to the body’s oxidative stress response. Scholar Liang et al.[20] showed that AOPP content was positively correlated with the degree of oxidative stress response which was an important indicator of the degree of lipid oxidation in the organism. GSH-Px is a widely distributed catalytic hydrogenolytic enzyme in the human body, which catalyzes the reduction of glutathione to form oxygen radicals to protect the function of cell membranes in tissues and organs[21]. The study by Song et al.[22] showed that under normal conditions, GSH-Px and AOPP could specifically regulate the level of oxygen free radicals in a balanced state, but once the level of GSH-Px was reduced or AOPP was increased, it would lead to a large accumulation of free radicals in the body, thus producing tissue damage. A study by Zhao et al.[23] found that Shenxian-shengmai oral liquid could reduce the expression of Reactive Oxygen Species (ROS) and MDA and promote the expression of SOD and GSH-Px in cardiac myocytes of rats in an ischemia-reperfusion model, thereby protecting the myocardium from oxidative damage by ischemia- reperfusion. In the present study, we found that the expression of SOD and AOPP in the serum of the post- ischemic adaptation-treated group was lower and GSH- Px and MDA were higher than those of the untreated group at the 8 h postoperative moment. This result suggests that ischaemia-adapted preconditioning can effectively enhance serum SOD and reduce serum MDA in patients, thereby improving the ability to scavenge oxygen free radicals to prevent ischaemic reperfusion injury.
The further follow-up results revealed 9 cases of reperfusion injury in the postoperative period in patients who had not undergone post-ischaemic adaptation, while only 3 cases occurred in the treated group with post-ischaemic adaptation. The incidence of MACE during the follow-up period was lower in the observation group than in patients without post- ischaemic adaptation. These results suggest that post- ischaemic adaptation is not only a safe and effective means of reducing MIRI, but may also improve the clinical prognosis of STEMI patients undergoing PCI to some extent.
In conclusion, although the mechanism of post- ischaemic adaptive management in the therapy of STEMI patients undergoing PCI is not fully understood, current clinical studies suggest that it may be related to the reduction of ROS production, diminution of cellular tissue inflammatory factor expression, inhibition of thrombin activation in the ischaemic area and activation of protective signaling pathways for reperfusion injury[24,25]. The results of this study suggest that post- ischaemic adaptation is not only a reliable and feasible means of reducing MIRI, but can also somewhat ameliorate the prognosis of clinical treatment of STEMI patients with PCI, making it an effective pre-treatment option for clinical treatment of STEMI patients with PCI and worthy of clinical promotion. However, there are some limitations to this study, such as the fact that it was a retrospective study comparing only 3 mo after reperfusion without long-term postoperative follow- up and failed to observe the effect of multiple balloon dilatations simulating post-ischaemic adaptation on the long-term prognosis of patients. In the future, large randomised controlled prospective studies are still needed to confirm the cardioprotective effect of post- ischaemic adaptation.
Funding:
This study was supported by Medical and Health Science and Technology program of Zhejiang Province (NO.2020KY087).
Conflict of interests:
The authors declared no conflict of interest.
References
- Hausenloy DJ, Yellon DM. Myocardial ischemia-reperfusion injury: A neglected therapeutic target. J Clin Invest 2013;123(1):92-100.
[Crossref] [Google Scholar] [PubMed]
- Feng GR. Therapeutic value of urokinase combined with atorvastatin calcium tablets in patients with ST-segment elevation myocardial infarction. Chin Pharmacoecon 2016;(13):256-9.
- Zhao X. Principles of treatment of acute myocardial infarction combined with multiple vascular lesions. Med Philos 2015;14(4):203-8.
- Qiao FB, He YL, Lu F. Effect of tirofiban in patients with myocardial infarction complicated by metabolic syndrome undergoing PCI. Guizhou Med 2017;14(9):314-7.
- Chen ZG, Wang GY, Shen XB. Clinical efficacy assessment of delayed PCI for acute ST-segment elevation myocardial infarction. Contemp Med 2017;6(3):113-6.
- Hao QQ, Wang LL, An SB. Effect of recombinant urokininogen combined with tirofiban in the interventional treatment of acute myocardial infarction. Chin J Clin Pharmacol 2017;12(10):398-400.
- Cohen MV, Downey JM. Is it time to translate ischemic preconditioning’s mechanism of cardioprotection into clinical practice? J Cardiovasc Pharmacol Ther 2011;16(3-4):273-80.
[Crossref] [Google Scholar] [PubMed]
- Chinese Medical Association Cardiovascular Branch. Guidelines for the diagnosis and treatment of acute ST-segment elevation myocardial infarction. Chin J Cardiovasc Dis 2010;38(6):675-90.
- Minamino T. Cardioprotection from ischemia/reperfusion injury-Basic and translational research. Circ J 2012;76(5):1074-82.
- Yue F, Zhang CY, Xu ZL. Clinical manifestations and analysis of myocardial ischemia-reperfusion injury after emergency PCI. China Mod Physician 2016;46(5):94-7.
- Staat P, Rioufol G, Piot C, Cottin Y, Cung TT, L’Huillier I, et al. Postconditioning the human heart. Circulation 2005;112(14):2143-8.
[Crossref] [Google Scholar] [PubMed]
- Lønborg J, Kelbæk H, Vejlstrup N, Jørgensen E, Helqvist S, Saunamäki K, et al. Cardioprotective effects of ischemic post conditioning in patients treated with primary percutaneous coronary intervention, evaluated by magnetic resonance. Circ Cardiovasc Interv 2010;3(1):34-41.
[Crossref] [Google Scholar] [PubMed]
- Thuny F, Lairez O, Roubille F, Mewton N, Rioufol G, Sportouch C, et al. Post-conditioning reduces infarct size and edema in patients with ST-segment elevation myocardial infarction. J Am Coll Cardiol 2012;59(24):2175-81.
[Crossref] [Google Scholar] [PubMed]
- Zhu WC, Qi XY, Dang Y. Research progress of intracoronary thrombolysis on improving myocardial perfusion in ST-segment elevation myocardial infarction. Chin J New Drugs 2017;12(4):246-9.
- Zou QW. Study on the changes of blood SOD, NO and LPO levels in patients with peptic ulcer. China Mod Doct 2015;12(4):202-8.
- Zeitz O, Maass AE, van Nguyen P, Hensmann G, Kögler H, Möller K, et al. Hydroxyl radical-induced acute diastolic dysfunction is due to calcium overload via reverse-mode Na+-Ca2+ exchange. Circ Res 2002;90(9):988-95.
[Crossref] [Google Scholar] [PubMed]
- Haizlip KM, Hiranandani N, Biesiadecki BJ, Janssen PM. Impact of hydroxyl radical-induced injury on calcium handling and myofilament sensitivity in isolated myocardium. J Appl Physiol 2012;113(5):766-74.
[Crossref] [Google Scholar] [PubMed]
- Bai J, Wang Q, Qi J, Yu H, Wang C, Wang X, et al. Promoting effect of baicalin on nitric oxide production in CMECs via activating the PI3K-AKT-eNOS pathway attenuates myocardial ischemia–reperfusion injury. Phytomedicine 2019;63:153035.
[Crossref] [Google Scholar] [PubMed]
- Engelhard K, Werner C, Eberspächer E, Bachl M, Blobner M, Hildt E, et al. The effect of the α2-agonist dexmedetomidine and the N-methyl-D-aspartate antagonist S (+)-ketamine on the expression of apoptosis-regulating proteins after incomplete cerebral ischemia and reperfusion in rats. Anesth Analg 2003;96(2):524-31.
[Crossref] [Google Scholar] [PubMed]
- Liang J, Deng TN, Yu LL. Serum levels of AOPP and IMA in patients with pre-eclampsia and their relationship with renal function. J Doubtful Dis 2015;18(11):24-8.
- Shi YN, Hou RT, Zhang N. Effect of Tongxinluo on GSH-PX SOD and MDA in patients with type 2 diabetes mellitus combined with coronary heart disease. Hebei Med 2016;12(3):667-71.
- Song Y, Zhao GZ, Zhao BX. Effect of different timing of interventional electrodes on HSP 70, MDA, SOD and GSH-PX in the liver of rats with simulated major disorders. Acupunct Res 2015;13(4):184-9.
- Zhao Y, Zhang X, Luan J, Zhao B, An N, Sun N, et al. Shenxian-Shengmai oral liquid reduces myocardial oxidative stress and protects myocardium from ischemia-reperfusion injury. Cell Physiol Biochem 2018;48(6):2503-16.
[Crossref] [Google Scholar] [PubMed]
- Tarantini G, Favaretto E, Marra MP, Frigo AC, Napodano M, Cacciavillani L, et al. Post conditioning during coronary angioplasty in acute myocardial infarction: The POST-AMI trial. Int J Cardiol 2012;162(1):33-8.
[Crossref] [Google Scholar] [PubMed]
- Zhou YF, Zhao CM, Xue F. Effect of post-ischemic adaptation on two-dimensional structure and left ventricular systolic function in acute myocardial infarction. Chin J Clin Physicians 2016;9(4):8130-4.
 Control and
Control and  Observation group
Observation group