- *Corresponding Author:
- Qiaoqiao Hu
Department of Critical Care Medicine, Xuzhou Central Hospital, Xuzhou, Jiangsu Province 221009, China
E-mail: zzyyzzyxk@163.com
| This article was originally published in a special issue, “Integrative Approaches in Biomedical Sciences for Drug Discovery and Development” |
| Indian J Pharm Sci 2024:86(6) Spl Issue “1-8” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
This study explores the effect of a modified prone ventilation strategy combined with pharmacological treatment on respiratory mechanics and hemodynamics in individuals with severe pneumonia. The study included 70 patients with severe pneumonia admitted between 2021 and 2023, they were randomly divided into a conventional treatment group and a combined treatment group. The conventional treatment group received standard antibiotic therapy supplemented by a routine prone ventilation strategy, while the combined treatment group received additional antiviral drugs and a modified prone ventilation strategy. Clinical indicators, blood gas analysis, respiratory mechanics, and hemodynamic parameters were compared between the two groups. The results showed that the combined treatment group demonstrated a more significant improvement in oxygenation and a reduction in complications (p<0.05), indicating that the optimization of prone ventilation strategy combined with pharmacological treatment has a significant therapeutic effect on individuals with severe pneumonia.
Keywords
Respiratory mechanics, hemodynamics, prone ventilation, optimization strategy, pneumonia
Severe pneumonia is a critical clinical condition often accompanied by respiratory failure and high mortality[1-4]. Traditional antibiotic therapy can alleviate the inflammatory response to some extent, but in severe cases, monotherapy may not be sufficient to adequately improve the patient’s respiratory mechanics and hemodynamic status[5-8]. In recent years, prone ventilation strategy has been widely applied in the treatment of severe pneumonia, improving the ventilation-perfusion ratio in the lungs and enhancing oxygenation[9-12]. Furthermore, the combined use of antiviral drugs has gradually become part of the comprehensive treatment for severe pneumonia[13]. This study aims to investigate the effects of a modified prone ventilation strategy combined with pharmacological treatment on respiratory mechanics and hemodynamics in individuals with severe pneumonia, providing a reference for clinical practice.
Materials and Methods
General information:
The subjects of this study were 70 patients with severe pneumonia admitted to a tertiary hospital between 2021 and 2023, randomly divided into a conventional treatment group (35 cases) and a combined treatment group (35 cases). Patients in the conventional treatment group received standard doses of antibiotics, supplemented by a routine prone ventilation strategy (with position changes every 2 h). The combined treatment group, in addition to this, received antiviral drugs (such as Arbidol, Ribavirin, etc.,) and a modified prone ventilation strategy. The modified ventilation strategy involved the use of pressure-sensitive air cushions to dynamically adjust patient positioning and optimize lung ventilation. Both groups received conventional supportive care, including oxygen therapy, position management, nutritional support, and more. Clinical indicators, blood gas analysis (e.g., partial Pressure of Oxygen (PaO2), partial Pressure of Carbon Dioxide (PaCO2), peripheral Oxygen Saturation (SpO2)), respiratory mechanics (peak inspiratory pressure (Ppeak), plateau pressure (Pplat), mean airway pressure (Pmean)), and hemodynamic parameters (e.g., Heart Rate (HR), Mean Arterial Pressure (MAP)) were monitored and recorded for all patients[11].
Inclusion and exclusion criteria:
Inclusion criteria: All patients met the diagnostic criteria for severe pneumonia, all patients received prone ventilation, and all patients had normal psychological will and were able to cooperate with care.
Exclusion criteria: Patients with combined spinal diseases, pregnant women, and patients with severe hematologic instability were excluded from this study.
Methodology:
Routine group and research group used programmed management mode, both groups strengthened nutrition, drink more water, adequate rest, hyperthermia patients were given antipyretic drugs, and symptoms were given to stop cough, asthma, expectoration, mechanical ventilation treatment. Ventilator parameters were set to platform pressure Pplat 30-35 cm Water (H2O), 1 cm H2O=0.098 kPa, tidal volume 6-8 ml/kg estimated body weight, positive end-expiratory pressure ≥5 cm H2O, lung protection ventilation strategy, and patients were given analgesic sedation and other treatments, and the Richmond agitation sedation score was controlled as -4 to 3 points[14].
Conventional group was given conventional prone ventilation, assisting patients in horizontal prone position, filled with soft pillows in the bony prominences, helping them to put their palms, hanging naturally on the sides of the body, and lower limbs placed naturally, turning them over every 2 h and making sure that all tubes were clear after turning them over[15].
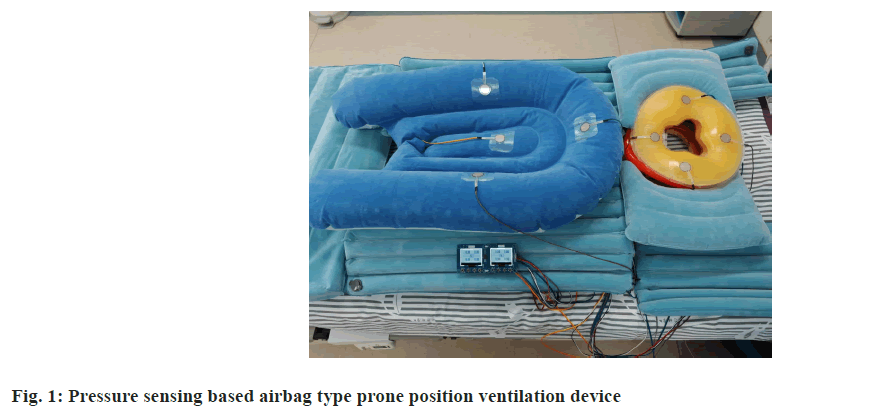
The study group was given modified prone ventilation, based on the control group, using a pressure-sensing based airbag prone ventilation device (fig. 1), which consists of a partial body airbag for the head, face, chest, abdomen, and iliac crest, with 8 flexible pressure sensors placed on top of the airbags, which monitors the real-time pressure and adjusts the airbag inflation volume to improve the patient’s comfort, and to avoid prolonged pressure in a certain area causing stress. The airbag is composed of 8 flexible pressure sensors above the airbag. During the treatment period, the flexible pressure sensors determine the pressure situation of the chest, adjust the pressure in time, maximize the suspension of the chest and abdomen, improve the ventilation status of the patient, and improve lung compliance. Both upper limbs were adjusted to a semi-flexed state, the lower limbs were placed naturally, and one of the lower limbs was adjusted to an upward and outward flexed state[16,17]. The inflatable pillow was alternately inflated and deflated every 1 h-2 h, and the patient’s head and trunk were tilted to one side for decompression. Ventilation was performed in the prone position for 16 h and in the supine position for 8 h. The cycle was repeated. If the patient developed abnormal respiratory function and severe hemodynamic fluctuations during this period, prone position ventilation therapy was terminated at an early stage[18].
The criteria for withdrawal were effective control or remission of lung disease, vital signs such as blood pressure, HR and body temperature near normal, liver and kidney function, blood gas analysis and acid-base balance at or near normal, and cough reflex recovery[19].
Observation indicators:
Among the clinical indicators, the mechanical ventilation time, hospitalization time, and lung infection control time of the two groups were observed.
Danish Radio Meter ABL9 blood gas analyser monitor the SpO2, PaCO2, PaO2, and PaO2/FiO2 in the prone position before, prone position 2, 4, 8, 12, 16 h in the 2 groups[20,21].
Hemodynamic indexes were observed in HR and MAP after prone position ventilation in both groups.
Respiratory mechanics indexes included the determination of airway plateau pressure, oxygenation index, partial pressure of carbon dioxide, and dynamic respiratory system compliance in both groups of patients after treatment[22].
Statistical processing:
Statistical analysis was performed using Statistical Package for the Social Sciences (SPSS) 20.0 software. Age measurements were expressed in the form of independent samples test was used between groups and paired samples test was used for all samples within groups. Count data were expressed as percent (%), and comparisons between groups were performed using the t-test, with p<0.05 being considered a statistically significant difference. Repeated-measures data were analysed using repeated-measures Analysis of Variance (ANOVA) and were used as test levels.
Results and Discussion
The results of the study showed that the combined treatment group had significantly better outcomes in improving oxygenation and respiratory mechanics compared to the conventional treatment group.
In blood gas analysis, the PaO2 value in the combined treatment group increased from a baseline of (68.24±8.25) to (90.97±6.25) mmHg, significantly higher than the 81.83±6.09 mmHg observed in the conventional treatment group.
The SpO2 in the combined treatment group increased from (89.21 %±5.14 %) to (97.52 %±2.56 %), while in the conventional treatment group, it increased from (89.98 %±5.06 %) to (95.73 %±3.83 %).
In terms of respiratory mechanics, the Ppeak and Pplat in the combined treatment group significantly decreased (p<0.05), indicating that the modified prone ventilation strategy was more effective in reducing airway pressure and improving lung compliance.
Additionally, the incidence of complications in the combined treatment group was significantly lower (p<0.05), suggesting that the combined treatment regimen has a higher safety profile.
Mechanical ventilation time, hospitalization time and lung infection control time of the patients in the study group and the conventional group after admission to the hospital record and record data for comparison, and compare the clinical indicators of the patients in the two groups as shown in Table 1. In the table, the mechanical ventilation time, hospitalization time and lung infection control time of the patients in the study group were more significant and shorter than those in the conventional group, and the differences were statistically significant (p<0.05).
| Group (n=35) | Mechanical ventilation time | Length of hospitalization | Time to control lung infection |
|---|---|---|---|
| Research | 5.67±0.78 | 11.21±0.93 | 6.12±1.01 |
| Conventional | 7.81±0.81 | 15.33±1.02 | 8.32±1.14 |
| t | 13.456 | 21.105 | 10.213 |
| p | <0.001 | <0.001 | <0.001 |
Table 1: Comparison of clinical indicators between the two groups of patients (Days) (x̄±s).
Arterial blood was collected from the study group and the conventional group before and after treatment, and the levels of PaCO2, PaO2, PaO2/FiO2, and SpO2 in the collected arterial blood were analysed by using the Danish radiometer ABL9 blood gas analyser. Comparison of the blood gas indexes of pneumonia between the two groups is shown in Table 2. The study group was ventilated in the modified prone position, and the conventional group was ventilated in the conventional prone position. PaCO2 is the arterial partial pressure of carbon dioxide, PaO2/FiO2 is the index of oxygenation, and SpO2 is the oxygen saturation of blood. p<0.05 compared with the pre-frontal position. G denotes the group, R is the study group, and C is the conventional group. A1-A6 were, respectively, the pre-prenatal position, prone position 2 h, prone position 4 h, prone position 8 h, prone position 12 h, and prone position 16 h.
| G | PaCO2/mmHg | |||||
|---|---|---|---|---|---|---|
| A1 | A2 | A3 | A4 | A5 | A6 | |
| R | 52.11±5.85 | 46.52±2.14 | 46.17±4.15 | 43.63±1.87 | 41.14±2.52 | 40.02±3.48 |
| C | 53.41±6.02 | 50.11±2.35 | 46.37±4.85 | 45.03±2.05 | 46.56±2.46 | 44.65±3.26 |
| G | PaO2/mmHg | |||||
| R | 68.24±8.25 | 73.52±8.14 | 75.96±8.29 | 83.63±7.59 | 86.14±7.98 | 90.97±6.25 |
| C | 67.96±7.79 | 72.74±9.08 | 75.35±8.15 | 77.76±7.45 | 79.95±7.86 | 81.83±6.09 |
| G | PaO2/FiO2 | |||||
| R | 153.25±12.21 | 169.63±13.52 | 179.33±15.32 | 189.52±11.43 | 215.39±10.09 | 227.68±13.17 |
| C | 151.98±10.98 | 170.14±11.83 | 178.25±14.99 | 179.46±12.58 | 199.52±11.14 | 203.82±14.63 |
| G | SpO2/% | |||||
| R | 89.21±5.14 | 90.24±4.79 | 92.85±4.52 | 95.15±3.52 | 96.93±2.96 | 97.52±2.56 |
| C | 89.98±5.06 | 90.95±4.57 | 92.89±4.49 | 92.01±6.44 | 93.06±3.24 | 95.73±3.83 |
Table 2: Comparison of blood gas indices of pneumonia in two groups of patients (x̄±s).
The difference in the data of PaCO2, PaO2, PaO2/FiO2, and SpO2 levels before prone position was statistically significant between the two groups (p<0.05), and the difference in the comparison of the time point interaction between the groups was statistically significant (p<0.05). Comparisons of PaCO2, PaO2, PaO2, PaO2, PaO2/FiO2, and SpO2 were statistically different between the two groups (p>0.05) in the pre-pronation, 2, 4, 8, 12, and 16 h periods.
Comparison of PaCO2, PaO2, PaO2/FiO2, and SpO2 before and after prone positioning between the study group and the conventional group showed that PaCO2 values of the study group decreased from (52.11±5.85) mmHg to (40.02±3.48) mmHg before prone positioning in the study group in the periods of 2, 4, 8, 12, and 16 h. The conventional group showed a decrease from (53.41±6.02) mmHg to (44.65±3.26) mmHg before prone positioning, (53.41±6.02) mmHg to (44.65±3.26) mmHg in both groups. 6.02 mmHg to (44.65±3.26) mmHg, (53.41±6.02) mmHg, (44.65±3.26) mmHg, PaCO2 values in both groups showed a uniform and slow decreasing trend. PaO2 values in the study group increased from (68.24±8.25) mmHg before prone position to (90.97±6.25) mmHg, whereas in the conventional group, PaO2 values increased from (67.96±7.79) mmHg before prone position to (81.83±6.09) mmHg. PaO2/FiO2 values in the study group increased from (153.25±12.21) mmHg before prone position to (227.68±13.17) mmHg in the study group and PaO2/FiO2 values increased from (151.98±10.98) mmHg before prone position to (203.82±14.63) mmHg in the conventional group. SpO2 values increased from 89.21 %±5.14 % to 97.52 %±2.56 % in the study group, and in the conventional group, SpO2 values increased from 89.98 %±5.06 % to 95.73 %±3.83 %. Thus, the PaCO2 group values of the study and conventional groups decreased with the increase in the duration of prone position ventilation, whereas those of the PaO2, PaO2/FiO2, and SpO2 groups increased with the increase in the duration of prone position ventilation, p<0.05. There was no statistical difference between the blood gas indices of the two groups of patients in the pre-pronation position, and during the initial 4 h of the prone position; however, with the increase in the prone position, the PaO2, PaO2/FiO2, and SpO2 groups of the observation group, PaO2/FiO2, and SpO2 were more significantly higher and PaCO2 was significantly lower than in the conventional group, and there was a statistically significant difference in the comparison between the two groups after 6 h of prone position ventilation, which indicated that modified prone position ventilation could better improve oxygenation.
In order to analyse the therapeutic effect of prone position ventilation optimization strategy on patients with severe pneumonia, hemodynamic monitoring of HR, MAP was used for patients in the study group and the conventional group. Comparison of HR and MAP at different time points in patients with severe pneumonia was shown in Table 3. Modified prone position ventilation was used in the observation group, and the control group was used in the conventional prone position. G is the group, R is the study group, and C is the conventional group. A1-A6 are before prone position, 2 h in prone position, 4 h in prone position, 8 h in prone position, 12 h in prone position, and 16 h in prone position, respectively, and N is the number of cases. HR, MAP is the number of cases is 35. As the duration of prone position increased, the HR values of the patients with severe pneumonia in the study group were consistently in the range of 88.35-89.00 min, whereas the HR values of the patients with severe pneumonia in the conventional group were consistently in the range of 87.49-87.56 min. The map values of the patients in the study group increased prone position time consistently in the range of (81.33-81.02) mmHg while the map values of the patients in the conventional group consistently in the range of (82.02-81.33) mmHg with small irregular fluctuations.
| G | n | Human resources/(minimum) | |||||
|---|---|---|---|---|---|---|---|
| A1 | A2 | A3 | A4 | A5 | A6 | ||
| R | 35 | 88.35±15.36 | 87.47±12.54 | 88.56±16.24 | 86.97±14.21 | 87.32±10.59 | 89.00±15.36 |
| C | 35 | 87.49±18.20 | 88.33±15.62 | 87.54±14.26 | 89.10±16.33 | 88.14±12.57 | 87.56±16.42 |
| MAP/mmHg | |||||||
| R | 35 | 81.33±12.24 | 80.57±14.02 | 81.02±13.65 | 80.75±13.44 | 80.87±11.97 | 81.02±15.46 |
| C | 35 | 82.02±14.36 | 81.78±12.25 | 81.45±15.32 | 80.98±12.57 | 81.12±11.24 | 81.33±10.98 |
Table 3: HR and MAP at different time points in patients with severe pneumonia (x̄±s).
It can be seen that the extension of the prone position, there is no difference in HR, MAP, in the prone position for 2, 4, 8, 12, 16 h. There is no difference in HR, MAP in the two groups with the prone position before, p>0.05. Therefore, it can be seen that, by the hemodynamic analysis of the two groups of patients, we have found that lateral ventilation does not affect the patient’s HR, MAP.
Comparing the respiratory mechanics indexes between the study group and the conventional group, Ppeak, Pmean, and Pplat indexes were selected as the physical monitoring indexes for patients with severe pneumonia. Comparison of respiratory function indexes in patients with pneumonia is shown in Table 4. The study group was ventilated in the modified prone position and the control group was ventilated in the conventional prone position. Ppeak is the peak airway pressure, Pmean is the mean airway pressure and Pplat is the plateau pressure. The p<0.05 when compared with the pre-prone position. Ppeak, Pmean and Pplat all tended to decrease slowly with increasing time in the prone position. Ppeak decreased by 39.90 % after 16 h of prone position compared to pre-prone position and Ppeak decreased by 24.67 % in conventional group compared to pre-prone position. The mean p value after 16 h in prone position decreased by 34.66 % in the study group and 24.67 % in the conventional group compared to the pre-prone position. After prone position, Pplat values were 41.64 % lower in the study group compared to pre prone position, whereas they were 29.66 % lower in the conventional group compared to pre prone position. The difference between the intertemporal interactions was statistically significant, p<0.01.There was no difference in the comparison of Ppeak, Pmean, and Pplat between the two groups before and at 2 h, 4 h, and time in the prone position, p>0.05. However, with the prolongation of the prone position ventilation time, Pmean, Ppeak, and Pplat of the patients in the study group declined more significantly than those in the observation group, which had a statistical difference, p<0.05. Therefore, prone position ventilation in both the conventional and study groups can improve the respiratory function of patients, and the modified prone position ventilation can reduce the Ppeak, Pmean, and Pplat of the patients more effectively than the conventional prone position ventilation, improve the lung compliance of the patients, and optimize the respiratory mechanical parameters.
| G | n | Ppeak | |||||
|---|---|---|---|---|---|---|---|
| A1 | A2 | A3 | A4 | A5 | A6 | ||
| R | 35 | 27.17±5.85 | 26.98±5.27 | 25.25±5.14 | 19.16±3.87 | 17.96±3.15 | 16.33±3.04 |
| C | 35 | 26.75±6.14 | 26.42±5.09 | 25.78±5.03 | 21.09±4.15 | 21.21±3.26 | 20.15±3.16 |
| Pmean | |||||||
| R | 35 | 20.14±5.17 | 19.95±4.96 | 17.86±4.55 | 16.14±3.49 | 13.52±2.86 | 13.16±2.03 |
| C | 35 | 19.89±5.12 | 19.67±4.68 | 18.06±4.38 | 18.08±3.22 | 17.38±2.47 | 15.21±2.25 |
| Airway platform pressure | |||||||
| R | 35 | 19.14±5.02 | 18.99±4.76 | 17.76±4.59 | 14.98±3.27 | 12.02±2.51 | 11.17±2.03 |
| C | 35 | 18.85±4.75 | 18.45±4.65 | 17.89±4.33 | 15.74±3.12 | 15.12±2.56 | 13.26±2.25 |
Table 4: Comparison of respiratory mechanics in pneumonia o2.
Complications occurring during the treatment of patients with severe pneumonia were recorded, and Table 5 shows the complication rates of the two groups. Among the 35 patients in the study group, there was 1 case of ventilator pneumonia and 1 case of pressure injury with a complication rate of 5.7 %, 1/35. In the conventional group, among the 35 patients, there were 2 cases of ventilator pneumonia, 1 case of catheter dislocation, and 5 cases of pressure injury, and thus the complication rate in the conventional group was 22.9 %, 8/35. It can be seen that the complication rate of the optimization strategy of prone ventilation studied in this paper was lower than that of the conventional prone ventilation method, and the total complication rate of the study group is lower than that of the control group, p<0.05, and the intervention method of the study group can effectively reduce the complication rate of patients with severe pneumonia.
| Group (n=50) | Ventilator pneumonia | Pipe separation | Stress injuries | Complication rate |
|---|---|---|---|---|
| Research | 1 (2.9) | 0 (0.00) | 1 (0.00) | 2 (5.7.00) |
| Conventional | 2 (5.7) | 1 (2.9) | 5 (14.3) | 8 (22.9.00) |
| χ² | / | / | / | |
| p | / | / | / | <0.001 |
Table 5: Comparison of complication rates between the two groups of patients.
This study demonstrates that a modified prone ventilation strategy combined with pharmacological treatment significantly improves oxygenation and respiratory mechanics in patients with severe pneumonia. The use of pressure-sensitive air cushions in the modified prone ventilation strategy allows for more dynamic adjustment of patient positioning, reducing the risk of lung injury and enhancing ventilation efficiency. The addition of antiviral drugs further enhances the treatment effect, reducing the incidence of complications from viral pneumonia. This combined strategy works synergistically through multiple mechanisms, not only significantly improving patient’s oxygenation index and shortening mechanical ventilation duration but also reducing the risk of complications during treatment.
One of the most notable outcomes of our research is the marked improvement in oxygenation indices observed in the combined treatment group. The modified prone ventilation strategy, which includes the use of pressure-sensitive air cushions, allows for more precise adjustments in patient positioning, thereby optimizing lung ventilation and reducing ventilator-associated lung injury[14]. This method contrasts with conventional prone ventilation, which typically involves less frequent adjustments and may not fully account for the dynamic changes in patient comfort and lung mechanics over time[15,16].
The addition of antiviral drugs to the treatment regimen further augments the therapeutic effect by targeting the viral components of pneumonia, which can be particularly relevant in cases where viral pathogens contribute to disease severity[17,18]. This dual approach-supporting both oxygenation and antiviral response-appears to synergize effectively, as evidenced by the significant reduction in mechanical ventilation time and hospital stay observed in the combined treatment group.
Our findings regarding respiratory mechanics are also noteworthy. The significant decrease in Ppeak, Pplat, and Pmean in the modified prone group suggests that this approach more effectively reduces airway pressures and improves lung compliance. This is crucial, as high airway pressures can lead to barotrauma, which is a common complication in mechanically ventilated patients[19,20]. By mitigating this risk, the modified prone ventilation strategy may contribute to a lower incidence of ventilator-associated complications.
Moreover, the hemodynamic stability observed in both treatment groups throughout the study period indicates that prone ventilation, whether modified or conventional, does not adversely affect cardiovascular function. This is an important consideration, as hemodynamic instability can be a limiting factor in the use of prone ventilation in certain patient populations[23,24].
The lower complication rate in the combined treatment group is another significant finding. By reducing the incidence of ventilator-associated pneumonia and pressure injuries, the modified prone ventilation strategy, in conjunction with pharmacological treatment, appears to enhance patient safety. This is a critical outcome, as complications can prolong hospital stays, increase healthcare costs, and negatively impact patient quality of life and survival.
This study shows that a modified prone ventilation strategy combined with antibiotic and antiviral therapy can significantly improve oxygenation, respiratory mechanics, and reduce the incidence of complications in patients with severe pneumonia. Compared with conventional treatment regimens, the combined treatment strategy exhibits more pronounced therapeutic effects, particularly in reducing the duration of mechanical ventilation and hospitalization. Future studies should further explore the optimal application of different prone ventilation strategies and drug combinations to optimize clinical treatment regimens for severe pneumonia.
Funding:
This study was supported by Xuzhou Science and Technology Plan Project No: KC21202.
Conflict of interests:
The authors declared no conflict of interests.
References
- Pozuelo-Carrascosa DP, Cobo-Cuenca AI, Carmona-Torres JM, Laredo-Aguilera JA, Santacruz-Salas E, Fernandez-Rodriguez R. Body position for preventing ventilator-associated pneumonia for critically ill patients: A systematic review and network meta-analysis. J Intensive Care 2022;10(1):9.
[Crossref] [Google Scholar] [PubMed]
- Wong MJ, Bharadwaj S, Lankford AS, Galey JL, Kodali BS. Mechanical ventilation and prone positioning in pregnant patients with severe COVID-19 pneumonia: Experience at a quaternary referral centre. Int J Obstetr Anesth 2022;49:103236.
[Crossref] [Google Scholar] [PubMed]
- Zhu X, Lu Z, Xiao W, Zhang J, Jia D, Yang M. The effect of prone position for ventilator-associated pneumonia in adult patients: A systematic review and meta-analysis. Emerg Crit Care Med 2021;1(1):37-44.
- Douglas IS, Rosenthal CA, Swanson DD, Hiller T, Oakes J, Bach J, et al. Safety and outcomes of prolonged usual care prone position mechanical ventilation to treat acute coronavirus disease 2019 hypoxemic respiratory failure. Crit Care Med 2021;49(3):490-502.
[Crossref] [Google Scholar] [PubMed]
- González-Seguel F, Pinto-Concha JJ, Aranis N, Leppe J. Adverse events of prone positioning in mechanically ventilated adults with ARDS. Respir Care 2021;66(12):1898-911.
[Google Scholar] [PubMed]
- Ashra F, Chen R, Kang XL, Chiang KJ, Pien LC, Jen HJ, et al. Effectiveness of prone position in acute respiratory distress syndrome and moderating factors of obesity class and treatment durations for COVID-19 patients: A meta-analysis. Intensive Crit Care Nurs 2022;72:103257.
[Crossref] [Google Scholar] [PubMed]
- Lurello AJ, Suarez-Carantona C, Oriol I, Sanchez-Diaz C, Coguan A. COVID-19 prone position in patients with severe acute respiratory distress syndrome: A retrospective study. Arch Wild Horse Zool 2012;58(3):277.
- Khanum I, Samar F, Fatima Y, Safia A. The role of conscious prone positioning in patients with moderate-to-severe covid-19: Experience from a developing country. Monaldi Chest Dis Arch 2021;91(2).
- Shelhamer MC, Wesson PD, Solari IL, Jensen DL, Steele WA, Dimitrov VG, et al. Prone positioning in moderate to severe acute respiratory distress syndrome due to COVID-19: A cohort study and analysis of physiology. J Intensive Care Med 2021;36(2):241-52.
[Crossref] [Google Scholar] [PubMed]
- Protti A, Santini A, Pennati F, Chiurazzi C, Ferrari M, Iapichino GE, et al. Lung response to prone positioning in mechanically-ventilated patients with COVID-19. Crit Care 2022;26(1):127.
[Crossref] [Google Scholar] [PubMed]
- Zhan Z, Cai H, Liang X, Lai S, Luo Y. Effects of 45 prone position ventilation in the treatment of acute respiratory distress syndrome: A protocol for a randomized controlled trial study. Medicine 2021;100(19):e25897.
[Crossref] [Google Scholar] [PubMed]
- Marklin GF, O'Sullivan C, Dhar R. Ventilation in the prone position improves oxygenation and results in more lungs being transplanted from organ donors with hypoxemia and atelectasis. J Heart Lung Transpl 2021;40(2):120-7.
[Crossref] [Google Scholar] [PubMed]
- Scaramuzzo G, Gamberini L, Tonetti T, Zani G, Ottaviani I, Mazzoli CA, et al. Sustained oxygenation improvement after first prone positioning is associated with liberation from mechanical ventilation and mortality in critically ill COVID-19 patients: A cohort study. Ann Intensive Care 2021;11(1):63.
[Crossref] [Google Scholar] [PubMed]
- Lee HY, Cho J, Quark Cui, Lee JJ, Park YS. Improvement in oxygenation status after prone positioning may be a predictor of survival in patients with acute respiratory distress syndrome. Crit Care Med 2020;48(12):1729-36.
- Matthews KS, Su H, Wang W, Bose S, Leaf DE. 2019 propensity to postural position and survival in mechanically ventilated patients with respiratory failure associated with coronavirus disease. Crit Care Med 2021;49(7):1026-37.
- Tatlow C, Haywood S, Hodgson C, Cunningham G, Conlon M, Ng HY, et al. Physical therapy-assisted covid ward-19 patients in the prone position: A retrospective cohort study. Phys Ther 2021;114:47-53.
- Chad T, Sampson C. Propensity to locate conscious patients on medical wards: A review of evidence from COVID-19 infected patients and its relevance to patients. Clin Med 2020;20(4);e97-103.
- Petit M, Fetita C, Gaudemer A, Treluyer L, Franchino G, Schmidt M. Anterior positioning in severe acute respiratory distress syndrome requiring extracorporeal membrane oxygenation. Crit Care Med 2021;50(2):264-74.
- Porta L, Cassano G, Gheda SA, Bellone A. Effect of exercise and postural changes on non-intubated respiratory failure patients with Covid-19 interstitial pneumonia. Acta Sci Med Sci 2021;5(12):2582.
- Chiumello D, Joao DC, Carpio P, Granata C, Pitimada M, Wendell G. Awake prone position reduces work of breathing in CPAP-supported COVID-19 ARDS patients. Ann Crit Care 202;11:1-10.
- Lee PH, Kuo CT, Hsu CY, Lin SP, Fu PK. Prognostic factors to predict ICU mortality in patients with severe ARDS who received early and prolonged prone positioning therapy. J Clin Med 2021;10(11):2323.
- Cammarota G, Rossi E, Vitali L, Simonte R, Sannipoli T, Anniciello F, et al. Effect of awake prone position on diaphragmatic thickening fraction in patients assisted by noninvasive ventilation for hypoxemic acute respiratory failure related to novel coronavirus disease. Crit Care 2021;25(1):305.
[Crossref] [Google Scholar] [PubMed]
- Singh P, Jain P, Deewan H. Awake prone positioning in COVID-19 patients. Indian J Crit Care Med 2020;24(10):914-8.
[Crossref] [Google Scholar] [PubMed]
- Zhang Z, Bai Y, Du Q. A case report of VV-ECMO combined with prone ventilation for Pneumocystis japonicus pneumonia. Medicine 2021;101(1):e28482.