- *Corresponding Author:
- Man Li, S. Zhang
Department of Anesthesiology, Chinese People’s Armed Police Force Hospital of Beijing, Haidian, Beijing 100600,China
E-mail: feng15233421582@163.com
| This article was originally published in a special issue, “Exploring the Role of Biomedicine in Pharmaceutical Sciences” |
| Indian J Pharm Sci 2024:86(1) Spl Issue “222-234” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
To observe the effects of general anesthesia combined with different anterior muscle plane block methods on pain relief and cognitive function in patients undergoing thoracoscopic lobectomy. 120 patients who were scheduled to undergo thoracoscopic lobectomy at a thoracic hospital from October 2022 to October 2023 were chosen and separated into a control group, namely the patient controlled intravenous anesthesia group; serratus muscle plane block group, namely single anterior serratus muscle plane block group and continuous insertion of serratius muscle plane block group. The time for first postoperative activity was shortened, and the total length of hospitalization was reduced (p<0.05). Relative to the patient controlled intravenous anesthesia group, the postoperative cognitive function of the single anterior serratus muscle plane block and continuous insertion of serratius muscle plane block groups was markedly improved, and the incidence of adverse events was markedly reduced (p<0.05). After thoracoscopic lobectomy, general anesthesia combined with anterior serratus muscle plane block is an important part of multimodal analgesia, which can provide patients with a good postoperative analgesia. The analgesic effect of single anterior serratus muscle plane block combined with patient-controlled intravenous analgesia mode is the best, and it can also reduce the incidence of adverse reactions caused by the total use of opioid drugs; the patient's comfort level is very high, and it can also enhance the early postoperative recovery and cognitive function, promoting the acceleration of rehabilitation process during the perioperative period.
Keywords
Anterior serratus muscle block, thoracoscopic lobectomy, analgesia, cognitive function
Lung cancer has taken a seat in the most common malignant tumors worldwide and is increasing year by year. Lobectomy combined with lymph node removal is a good treatment method[1,2]. The current thoracic surgery has evolved from the traditional open chest surgery to the minimally invasive surgery represented by the use of Visual Assisted Thoracoscopic Surgery (VATS) technology; the latter has been proven to be a more excellent and promising surgical method[3,4]. As the boost and popularization of minimally invasive surgical techniques, VATS surgeons can use modern high-definition camera technology to magnify the tissue inside the chest cavity through an incision of about 3-5 cm, thereby achieving its operation. In addition, the use of age-related closed cutting staplers is also being used. This greatly reduces the damage to chest surgery, and minimally invasive surgery has essentially reached a very high level[5,6]. However, up to 78 % of patients still undergo moderate or even harsh postoperative pain when using VATS treatment, so this defect cannot be ignored. Through research by relevant scholars, it has been found that the main reasons for this situation are twofold. Firstly, the thoracic nerve is dense, causing damage to the ribs and intercostal nerves due to local dilation during surgery or thoracoscopy. Secondly, damage to the peripheral nerves can lead to nerve degeneration, leading to the release of harmful inflammatory mediators. These inflammatory mediators alter the peripheral and central nervous system, ultimately leading to neuropathic pain[7,8]. The pain After Surgery (AS) affects the patient’s deep breathing, effective ventilation, and coughing and sputum excretion, while turbid phlegm can lead to atelectasis, pulmonary infection, and even pulmonary failure. And patients are limited due to pain during the early stages of surgery, which increases the probability of developing blood clots. Both of these situations can lead to longer hospital stays for patients, resulting in higher medical expenses and affecting their postoperative recovery rate[9,10]. There is an urgent need for a safe and effective analgesic method as a component of multimodal analgesia after VATS surgery. Therefore, the study utilized general anesthesia combined with different methods of Anterior Serratus Muscle (ASM) plane block to analyze its impact on pain relief and cognitive function in patients undergoing Thoracoscopic Lobectomy (TL). The purpose is to explore the analgesic influence of single and continuous ASM plane block on general anesthesia during VATS surgery and the recovery of postoperative cognitive function, and to preliminarily explore the application of these two methods in promoting VATS surgery. Meanwhile, the method used in this study has a combined effect on enhancing analgesic effect and improving cognitive function, which has a significant improvement relative to previous studies and is therefore innovative.
Materials and Methods
Research subjects:
A study was conducted on 120 patients who were scheduled to undergo TL at a hospital. The American Society of Anesthesiologists (ASA) graded them as I to III. The experiment was actually approved by the Ethics Committee of the Thoracic Hospital, and all patients were informed and signed consent form.
Inclusion, exclusion, and reject criteria:
Inclusion criteria: Patients aged 18 y-65 y old and the Body Mass Index (BMI) is 20-25 were included.
Exclusion criteria: Contraindications for neurogenic block puncture, including allergic local anesthesia, severe abnormalities in coagulation related functions, systemic or puncture related infections, and neurological damage; long term alcohol consumption or long-term use of psychotropic and opioid drugs; adjuvant chemotherapy or radiation therapy has been performed before the surgery; due to any reason, continuous collaborative research cannot be conducted, such as inability to understand the scale, mental illness, language disorders, and inability to conduct follow-up visits AS have taken other experimental drugs or conducted other clinical trials within 3 mo and subjects who refuse experimental procedures.
Rejected criteria: Failure of Serratus Anterior Plane Block (SAPB); patients who need to undergo thoracotomy during surgery and undergo secondary surgery; AS patients who experience significant bleeding and patients who experience loss of contact during follow-up visits.
Grouping methods and pharmaceutical instruments:
Grouping method: This study used a random number table method and computer-generated random quantities to divide patients into three groups, with 50 patients in each group. It is divided into a Control Group (CG), the Patient Controlled Intravenous Analgesia (PCIA) group, which is the PCIA group; the Experimental Group (EG) SPB group, namely the single ASM plane block (SPB) group and the EG Continuous insertion of Serratus Muscle Plane Block (CSPB) group. The research group content was shown in fig. 1.
Fig. 1 shows 120 patients with VAT after inclusion and exclusion criteria. Three patients underwent intraoperative changes to open chest surgery (2 in the PCIA group and 1 in the CSPB group); two cases experienced loss of follow-up 2 mo after discharge (SPB group); in the end, 116 subjects completed the study (48 in the PCIA group, 49 in the SPB group, and 48 in the CSPB group). In addition, the main drugs and instruments are shown in Table 1.
Table 1 indicates that the main drugs include ropivacaine hydrochloride injection, which is produced by AstraZeneca Pharmaceuticals Limited in Sweden; sufentanil citrate injection, produced by Yichang Humanwell Pharmaceutical Co., Ltd; propofol injection, produced from AstraZeneca. The materials and instruments include the Datex Ohmeda anesthesia machine produced by Omeda in the United States; the Philips 580 ultrasound instrument produced by Philips in the Netherlands; disposable dual lumen bronchial intubation produced by Hangzhou Tampa Medical Technology Co., Ltd; 18G and 22G puncture needles produced by Bidi Medical Devices Co., Ltd. in the United States.
| Country | Name | Type | Producer |
|---|---|---|---|
| Sweden | Ropivacaine Hydrochloride injection | - | AstraZeneca AB |
| China | Sufentanil mesilate injection | - | Xuanchang Human well Pharmaceutical Co., Ltd |
| Sweden | Propofol injection | Diprivan 1 % w/v | AstraZeneca |
| America | Anesthesia machine | Datex-Ohmeda | Ohmeda |
| Holland | Ultrasound | Philips 580 | Philips |
| China | Disposable dual lumen bronchial intubation | - | Tampa Medical Technology Co., Ltd |
| America | Puncture needle | 18G and 22G | BD Medical Devices Co., Ltd |
Table 1: Schematic Diagram of Main Drugs and Instruments
Preoperative education and anesthesia methods:
Preoperative education: A fixed anesthesiologist on the day before surgery will provide necessary pain score related publicity and education during patient follow-up, so that patients can accurately use Visual Analog Scale (VAS) to describe and locate their actual pain level; promote and educate the Postoperative Recovery Quality Scale (QoR-40), while completing the actual QoR-40 score from the previous day (T0) and inform and ensure that the patient has actually learned the relevant usage methods of patient-controlled analgesia.
Anesthesia method: Before surgery, patients underwent a routine 8 h fasting and 2 h drinking ban. After entering the operating room and undergoing third-party verification, the healthy peripheral venous pathway was opened for routine electrocardiogram, heart rate (Beats Per Minute (BPM)), blood oxygen saturation, non-invasive blood pressure, and Bispectral Index (BIS) monitoring. All three groups were given intravenous infusion of 0.5 dexmedetomidine μg/kg to achieve sedation, and observe the arterial pressure of the injured upper limb in the radial artery puncture tube of the healthy upper limb, then give midazolam 0.05~0.1 mg/kg and sufentanil 0.5~1.0 μg/kg respectively, induction of general anesthesia with etomidate 0.2-0.3 mg/kg, and cisatracurin 0.3 mg/kg. Double lumen endobronchial intubation was performed after adequate oxygen and nitrogen supplementation, and fiber bronchoscopy was used for positioning and fixation; after connecting to the anesthesia machine meanwhile, it adjusts the tidal volume to 6-8 ml/kg, 12-14 BPM, 60 %-100 %, Positive End Expiratory Pressure (PEEP) 4 mmHg, and a 60 %-100 % oxygen concentration.
After protecting the tracheal intubation, help the patient roll over to the surgical position, complete surface positioning markers, and disinfect the tissue. Under the guidance of ultrasound, the affected side Z4 and Z7 (block area, including Z2~Z9, all located on the lateral cutaneous branch of the intercostal nerve) were subjected to thoracic paravertebral block. A 22G puncture needle was inserted into the plane and reached the corresponding paravertebral space under direct ultrasound vision. 0.375 % ropivacaine 10 ml was administered to each point. This indicates a significant downward pressure of the pleura towards the ventral side. Maintain anesthesia by intravenous injection of propofol with a target plasma concentration of 1-2 µg/ml, and intermittently inject 5-10 mg of cisatracurium; meanwhile, the patient’s blood pressure should be controlled below 20 % of the normal level, the BIS value should be kept in 40-60, and the end expiratory Partial Pressure Carbon dioxide (PETCO2) should be kept in 35-45 mmHg.
Ultrasound guidance: SPB group maintained their surgical position continuously AS and before extubation, with the fifth rib marked on the body surface. It disinfects the tissue and uses a linear high-frequency ultrasound probe to place it at the midaxillary line. At this point, two layers of muscles can be clearly seen, namely the superficial and deep latissimus dorsi and Serratus Anterior Muscles (SAM). Next, the 18 g puncture needle was inserted from the top to the bottom plane and reached the surface of the SAM under ultrasound direct vision. At this time, no blood or gas was extracted and a dose of 2 ml 0.375 % of ropivacaine was administered. Under ultrasound, a liquid dark area can be clearly seen. At this point, the fascia of the ASM is pushed open and drawn back again without blood or gas. Meanwhile, the remaining 15 ml of 0.375 % ropivacaine is slowly injected. The CSPB group underwent puncture using the same method as the SPB group and received 15 ml of 0.375 % ropivacaine. Then, an external catheter was inserted into the dura mater and left at a depth of 5 cm. After the skin was properly fixed, the actual position of the catheter was determined again using ultrasound.
Postoperative analgesia treatment: Three groups of patients were pulled out and connected with the analgesia pump when they recovered consciousness and met the indications for extubation after the operation, and then returned to the postoperative care unit of thoracic surgery. In the PCIA and SPB groups, 2~3 µg/kg sufentanil+12 mg butorphanol+0.9 % sodium chloride injection 150 ml was used, the background dose was 2 ml/h, Patient Controlled Analgesia (PCA) 2 ml was given, and the blocking time was 15 min. The CSPB group was connected to a continuous ASM block self-control analgesia pump, with a formula set at 300 ml of 0.2 % ropivacaine physiological saline, a background infusion dose of 6 ml/h, a PCA dose of 6 ml, and a locking time of 45 min. Three groups of patients underwent patient-controlled analgesia within 48 h AS. If the VAS was >4, the patient-controlled analgesia pump could be pressed once; if the VAS is >6, 10 mg morphine injection can be injected intramuscularly to compensate for the pain; in case of severe nausea and vomiting, 8 mg ondansetron can be injected intravenously, or the use of the analgesia pump can be temporarily stopped.
Observation indicators:
It records the patient’s basic information, including gender, age, BMI, length of surgery, and actual bleeding volume during surgery; it records the VAS scores of patients at rest and exercise at 1 h (T2), 6 h (T3), 12 h (T4), 24 h (T5), and 48 h (T6) AS; it records the time when the patient first underwent patient-controlled analgesia AS, the actual effective number of times the electronic analgesic pump was pressed 48 h AS, the actual total amount of opioid drugs used in the electronic pump, and whether postoperative pain relief was performed and the relevant number of times. It records the arterial Partial Pressure of Oxygen (PaO2), PaCO2, Lactic acid (Lac), and Glucose (Glu) levels of patients 12 h before (T1) and 24 h after (T5) surgery; all adverse reactions after operation were recorded, including nausea and vomiting, dizziness, urinary retention, constipation, related hematoma and infection under the puncture site, local anesthesia poisoning and different complications; it records the QoR-40 scale scores of the patient on the day before surgery (T0) and 48 h AS (T6); it records the actual time of the patient's first postoperative activity and the total number of days hospitalized; their follow-up recorded the actual incidence of chronic pain 2 mo AS (evaluated through telephone follow-up) and it records the cognitive function of patients AS.
Statistical processing:
Statistical Package for the Social Sciences (SPSS) 19.0 software was utilized for statistical analysis, and the measurement data consistent with normal distribution were revealed in the form of mean±standard deviation (x̄±s); the metric data of skewed distribution is represented by the Median Inter Quartile Range (MIQR). Meanwhile, one-way Analysis of Variance (ANOVA) was utilized for inter group comparison, t-test was utilized for pairwise comparison, percentage (%) was utilized for counting data, and Chi square (χ2) test was utilized. p<0.05 was set for indicating that the disparity is statistically notable.
Results and Discussion
The basic information of the patients participating in the research is that they are aged between 52 y and 68 y old; maintain MI values between 25 kg/m2 and 32 kg/m2; the surgical duration should be maintained between 127 min and 141 min; maintain intraoperative bleeding between 40 ml and 51 ml and the QoR-40 score remains between 193 and 199. Overall, the p values between each indicator of the three groups of patients are >0.05, indicating that the disparity is not statistically notable as shown in Table 2.
| Group | Number of cases | Gender (male/female) | Age (years) | BMI (kg/m2) | Surgical duration (min) | Intraoperative bleeding volume (ml) | QoR-40 score at T0 (points) |
|---|---|---|---|---|---|---|---|
| PCIA | 48 | 29.00/19.00 | 52.35±10.86 | 25.64±4.20 | 127.51±6.67 | 42.30±7.75 | 193.86±4.32 |
| SPB | 49 | 26.00/23.00 | 53.46±11.62 | 25.62±5.15 | 130.81±9.60 | 40.62±10.20 | 194.62±4.40 |
| p | - | 0.46 | 0.63 | 0.98 | 0.06 | 0.36 | 0.39 |
| CSPB | 48 | 28.00/20.00 | 56.33±11.63 | 25.95±5.32 | 129.77±7.81 | 40.11±10.35 | 194.69±4.64 |
| p | - | 0.83 | 0.08 | 0.75 | 0.13 | 0.24 | 0.37 |
Table 2: Schematic Diagram of the Basic Situation of three groups of Patients
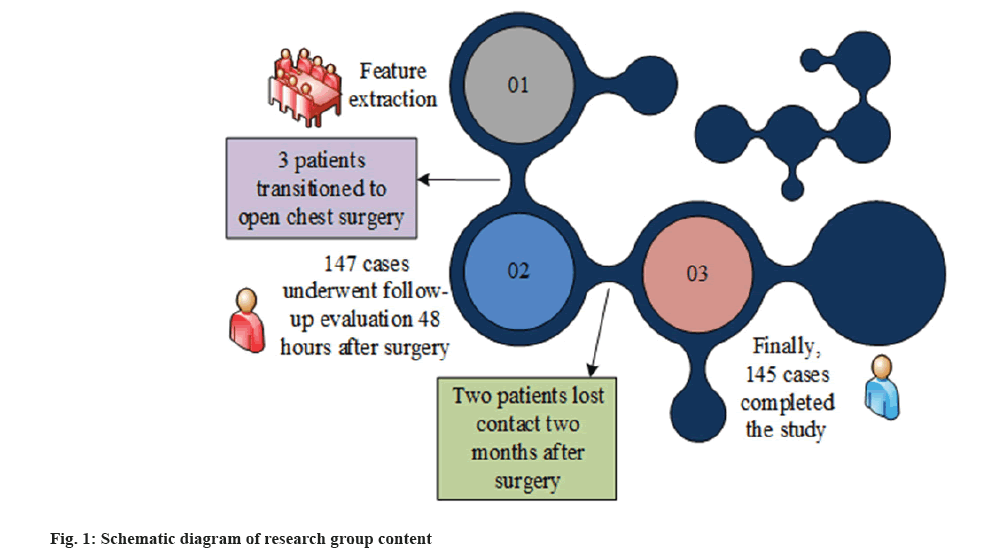
In addition, in the comparison of VAS among the patients participating in the experiment, the SPB group and CSPB group in the EG showed a significant downward trend in VAS scores at rest and exercise at T2, T3, T4, and T5 relative to the PCIA group in the CG. Among them, in the resting VAS score, the highest value in the SPB group appeared at T5, which was 2.2±0.4; the highest value in the CSPB group also appeared at T5, at 2.4±0.5, both lower than the 3.1±0.5 in the PCIA group. In the sports VAS score, the highest value in the SPB group appeared at T4, at 2.7±0.6; the highest value in the CSPB group also appeared at T4, at 3.3±0.3, which was lower than 4.5±0.5 in the PCIA group. In addition, in the resting VAS score at T6, the SPB group and CSPB group had scores of 1.7±0.5 and 1.8±0.5, respectively, which were lower than the PCIA group’s scores of 2.2±0.6; in the exercise VAS score, the SPB group and CSPB group had scores of 2.1±0.7 and 2.2±0.7, which were below the PCIA group’s scores of 2.3±0.6.
Meanwhile, there was a Significant Difference (SD) in resting and exercise VAS scores among the three groups of patients at T2, T3, T4, and T5 (p<0.05), while there was no Statistically SD (SSD) in resting and exercise VAS scores among the patients participating in the experiment at T6 (p>0.05). However, in the comparison in the EG SPB group and the CSPB group, SSD does not exist in scores at T2, T3, and T6 (p>0.05). There was a SD in scores at T4 and T5 (p<0.05), and the scores of the SPB group were markedly below the CSPB group as shown in fig. 2.
Fig 2: Comparison of VAS scores under rest and exercise at different times after surgery among three groups of patients *p<0.05, demonstrates that the disparity between the EG SPB group, CSPB group, and the CG PCIA group has SS and **p<0.05, indicates that the disparity in the EG SPB group and the CSPB group has SS,
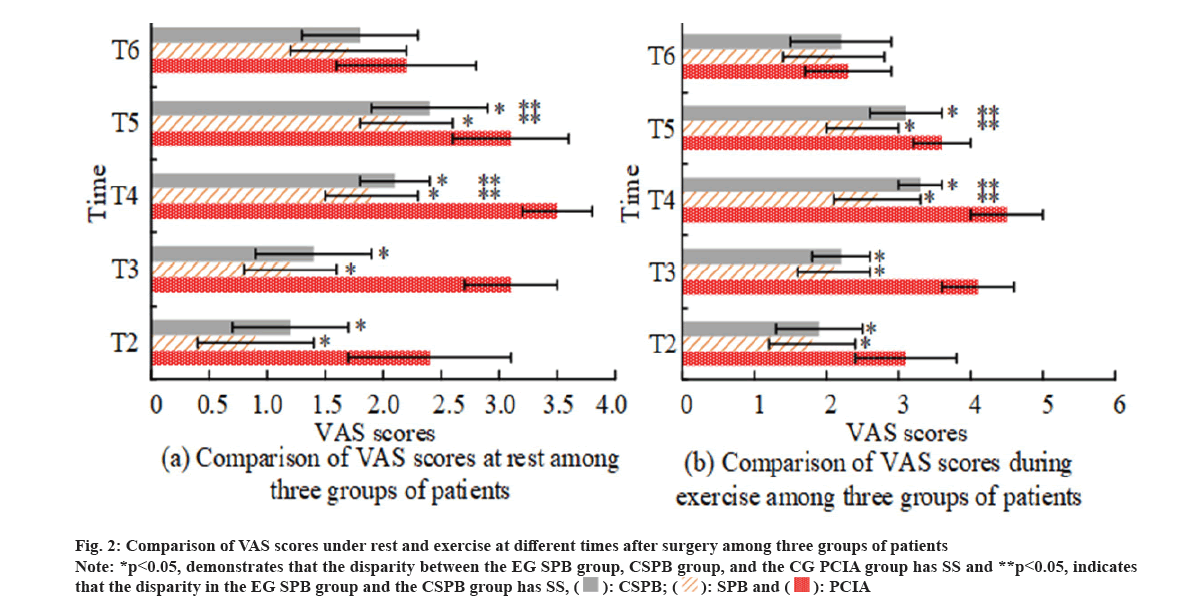
Based on the VAS scores at different time points, the time effect, grouping effect, and the VAS scores of resting pain, cough pain and analgesic pump consumption under the time grouping influence of the patients participating in the experiment showed that the F-values of the time effect under the three indicators were 42.38, 88.63, and 21.92, respectively; the F-values of grouping effects are 9.08, 7.72, and 13.28, respectively; the time grouping effects were 27.3, 13.57, and 112.44, respectively. Overall, the VAS scores at different time points AS exhibit different trends as they change. The p values of the three are all below 0.05, and the disparity has Statistical Significance (SS) as shown in fig. 3.
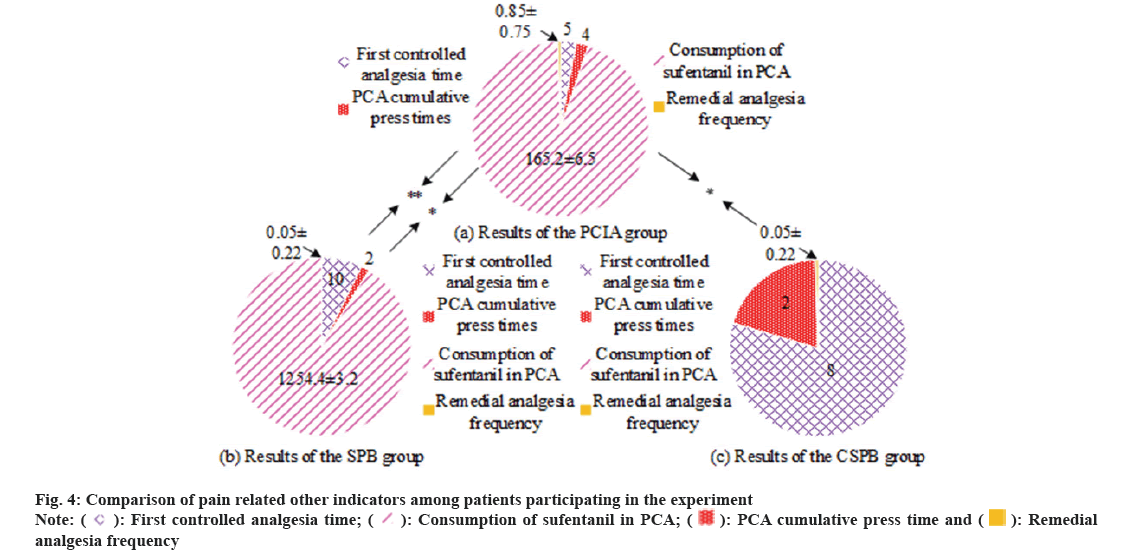
In the comparison of the first postoperative patient-controlled analgesia time among the three groups of patients, the PCIA group had 5 h, the SPB group had 10 h, and the CSPB group had 8 h; the MIQR values of the three groups were 2.5, 7.0, and 10.0, respectively, indicating a significant prolongation of the patient-controlled analgesia time in both EG. In the comparison of the cumulative quantity of PCA compressions within 48 h AS, the actual cumulative number of compressions in the PCIA group was 4, SPC group was 2, and CSPB group was 2. The MIQR values of the three groups were 2.5, 1.5, and 2.0, respectively. In the comparison of sufentanil consumption in PCA, the actual consumption in PCIA group was 165.2±6.5 μg, 124.4±3.2 for SPB group and CSPB group is 0 μg. In the comparison of rescue analgesia times, the PCIA group had 0.85±0.75 times, the SPB group had 0.05±0.22 times, and the CSPB group had 0.05±0.22 times. Overall, relative to the PCIA group, the disparity in the SPB group and the CSPB group in the first, second, and fourth indicator values have SS (p<0.05). The disparity in the SPB group and the PCIA group in the third indicator has SS (p<0.05), while the CSPB group PCA pump did not use opioid drugs, so it was not considered. Comparing the SPB group with the CSPB group, the disparities in the values of the first, second, and fourth indicators were statistically significant (p<0.05) as shown in fig. 4.
In the comparison of PaO2 among the three groups of patients, the values of PCIA group at T2, T4, and T5 were 92.71±3.45 mmHg, 90.50±2.56 mmHg, and 91.60±3.20 mmHg, respectively; the SPB group was 93.37±2.90 mmHg, 92.07±3.41 mmHg, and 92.71±2.34 mmHg, respectively; the CSPB group was 93.20±2.77 mmHg, 92.13±3.33 mmHg, and 92.81±2.18 mmHg, respectively. In Lac comparison, the values of the PCIA group at three time points were 1.44±0.21 mmol/l, 2.12±0.64 mmol/l, and 1.83±0.42 mmol/l, respectively; the SPB group was 1.31±0.55 mmol/l, 1.94±0.35 mmol/l, and 1.75±0.21 mmol/l, respectively; The CSPB group was 1.36±0.46 mmol/l, 2.00±0.31 mmol/l, and 1.77±0.43 mmol/l. In Glu comparison, the values of the PCIA group at three time points were 6.41±1.42 g/l, 7.61±1.50 g/l, and 6.83±1.31 g/l, respectively; the SPB group was 6.02±0.95 g/l, 7.82±1.72 g/l and 7.11±1.42 g/l, respectively; the CSPB group was 6.14±1.20 g/l, 7.58±1.89 g/l, and 7.08±1.55 g/l, respectively. Overall, there was no SSD in PaO2 between T2 and T5 among the patients participating in the experiment (p>0.05), while there was a SSD in T4 (p<0.05); after conducting pairwise comparisons between different groups at the same time point, it was found that there was no SSD among the patients participating in the experiment in the comparison of the three indicators (p>0.05). It is worth noting that when compared within each group, the Lac and Glu levels of patients at T4 and T5 were significantly improved relative to those at T1, and the disparity has SS (p<0.05). The specific content is illustrated in Table 3.
| Group | T2 | T4 | T5 | |
|---|---|---|---|---|
| PaO2 | PCIA | 92.71±3.45 mmHg | 90.50±2.56 mmHg | 91.60±3.20 mmHg |
| SPB | 93.37±2.90 mmHg | 92.07±3.41 mmHg | 92.71±2.34 mmHg | |
| ap | 0.37 | 0.01* | 0.06 | |
| CSPB | 93.20±2.77 mmHg | 92.13±3.33 mmHg | 92.81±2.18 mmHg | |
| - | bp | 0.44 | 0.01* | 0.06 |
| Lac | PCIA | 1.44±0.21 mmol/l | 2.12±0.64 mmol/l | 1.83±0.42 mmol/l |
| SPB | 1.31±0.55 mmol/l | 1.94±0.35 mmol/l | 1.75±0.21 mmol/l | |
| ap | 0.13 | 0.09 | 0.23 | |
| CSPB | 1.36±0.46 mmol/l | 2.00±0.31 mmol/l | 1.77±0.43 mmol/l | |
| - | bp | 0.28 | 0.24 | 0.49 |
| Glu | PCIA | 6.41±1.42 g/l | 7.61±1.50 g/l | 6.83±1.31 g/l |
| SPB | 6.02±0.95 g/l | 7.82±1.72 g/l | 7.11±1.42 g/l | |
| ap | 0.11 | 0.54 | 0.32 | |
| CSPB | 6.14±1.20 g/l | 7.58±1.89 g/l | 7.08±1.55 g/l | |
| - | bp | 0.31 | 0.93 | 0.39 |
Note: *p<0.05, indicates that the disparity has SS; ap represents the comparing between the SPB group and the PCIA group and bp represents the comparing in the CSPB group and the PCIA group
Table 3: Comparison Results of Pao2, Lac, and Glu Among Three Groups of Patients
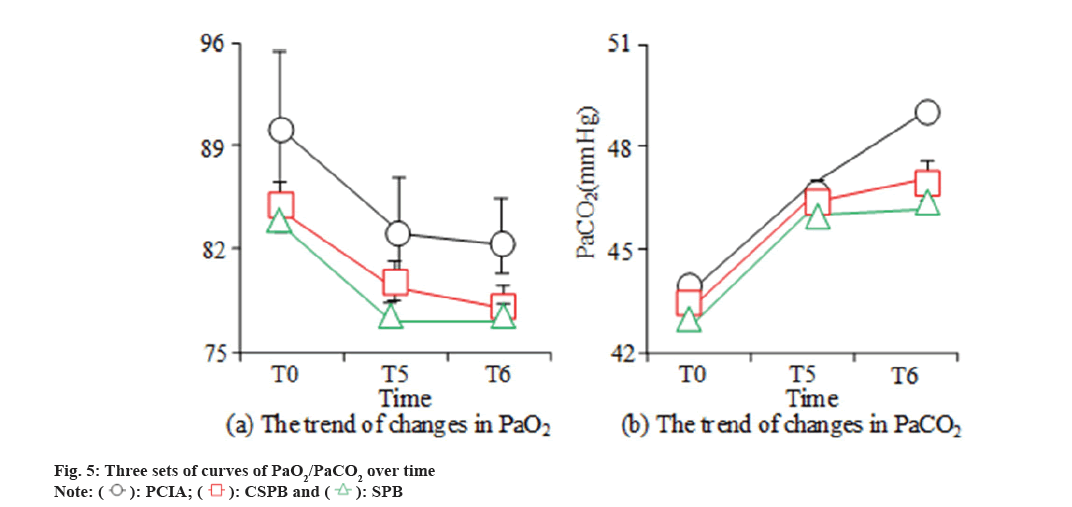
Due to the presence of statistically different time points in PaO2, PaO2 was extracted separately to compare the PaO2 and PaCO2 values of three groups of patients before and AS (T0, T5 and T6). Relative to the PCIA group, the PaO2 value of the CSPB group was 0.35 lower per day, but at this point, the p value was 0.56, and the disparity has SS (p>0.05); the PaO2 value of SPB is 0.21 lower, at which point the p value is 0.73, and the disparity does not have SS. The value of PaCO2 in the SPB group markedly grew at the time point T6 AS, with a p value of 0.03, indicating SSD (p<0.05 as shown in fig. 5.
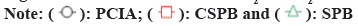
In the comparison of QoR-40 scale scores among the patients participating in the experiment, the total scores of SPB group and CSPB group at T6 were 185.1±4.1 and 188.6±3.6, respectively, which showed a significant improvement relative to the PCIA group. The disparities among the patients participating in the experiment have SS (p<0.05). Among them, the scores of emotional state, Physical Comfort (PC), psychological support, Self-Care Ability (SCA), and pain in the SPB group were 42.4±1.0, 53.8±1.7, 32.5±2.2, 24.0±0.8, and 34.2±0.9, respectively; the scores of the five indicators in the CSPB group were 42.5±1.8, 58.0±1.1, 31.5±1.7, 24.1±0.6, and 32.1±0.7, respectively. Overall, the scores of PC, SCA, and pain illustrated a growth, with SS (p<0.05). From the comparison in the SPB group and the CSPB group, the total QoR-40 scale score and PC score of the CSBP group showed a significant increase, and the disparity has SS (p<0.05). The score was markedly reduced, and the disparity has SS (p<0.05). The specific content was shown in fig. 6.
In the comparison of adverse reactions and postoperative chronic pain incidence, the PCIA group had 15 cases of nausea and vomiting, accounting for 31.6 %, and 13 cases of dizziness, accounting for 26.3 %. Both groups were much higher than the SPB and CSPB groups. Under chronic pain indicators, the number of cases in the PCIA group was 8, which was the same as that in the CSPB group, but higher than the 7 cases in the SPB group. Overall, the incidence of nausea, vomiting, and dizziness in the SPB and CSPB groups was diminished relative to the PCIA group, and the disparity has SS (p<0.05). Compared with the SPB group, the probability of nausea, vomiting, and dizziness in the CSPB group is smaller, and the disparity between the two has SS (p<0.05). The difference in chronic pain indicators among the three groups is not significant and does not have SS (p>0.05). The specific content is illustrated in Table 4.
| Nausea and vomiting | Dizzy | Chronic pain | ||||
|---|---|---|---|---|---|---|
| Number of cases | Proportion | Number of cases | Proportion | Number of cases | Proportion | |
| PCIA | 15.00 | 0.316 % | 13.00 | 0.263 % | 8.00 | 0.184 % |
| SPB | 9.00 | 0.179 % | 8.00 | 0.154 % | 7.00 | 0.153 % |
| aP | 0.00* | 0.00* | >0.05 | |||
| CSPB | 4.00 | 0.077 % | 2.00 | 0.051 % | 8.00 | 0.167 % |
| bp | 0.00* | 0.00* | >0.05 | |||
Note: *p<0.05, indicates that the difference has SS; ap represents the comparing in the SPB group and the PCIA group and bp represents the comparing in the CSPB group and the PCIA group
Table 4: Comparing of Adverse Reactions and Postoperative Chronic Pain Incidence among three Groups of Patients
In addition, in comparison of postoperative recovery indicators among the patients participating in the experiment, the first postoperative landing time and total hospitalization days of the PCIA group were 17.4±2.0 h and 12.4±2.5 d, respectively; the SBP group had 6.4±3.1 h and 7.8±1.7 d, respectively, while the CSPB group had 10.2±2.8 h and 9.1±2.0 d, respectively. Overall, relative to the PCIA group, the SPB group and CSPB group showed a significant decrease in the first time spent in the field, as well as a decrease in the total quantity of hospital days. The disparity has SS (p<0.05). Relative to the SPB group and the CSPB group, the CSPB group showcased an increase in the first time of physical activity and the total of days hospitalized, and the disparity in the two has SS (p<0.05) as shown in Table 5.
| First postoperative landing time | Total length of hospitalization | |
|---|---|---|
| PCIA | 17.40±2.00 h | 12.40±2.50 h |
| SPB | 6.40±3.10 d | 7.8±1.70 d |
| ap | 0.00* | 0.00* |
| CSPB | 10.20±2.90 d | 9.10±2.00 d |
| bp | 0.00* | 0.00* |
Note: *p<0.05, indicates that the disparity has SS; ap represents the comparing between the SPB group and the PCIA group and bp represents the comparison in the CSPB group and the PCIA group
Table 5: Comparing of Postoperative Recovery Indicators Among Patients Participating in the Experiment
Relative to the PCIA group, the CSPB group and SPB group illustrated shorter stay time in the Postanesthesia Care Unit (PACU), sedation and irritability score, and hospitalization time in the three groups of patients after anesthesia. The disparity has SS (p<0.05). The sedation and irritability scores of the CSPB and SPB groups were also significantly reduced, with the SPB group below the CSPB group, and the disparity has SS (p<0.05). In terms of postoperative complications, there was no SSD in the incidence of lung infection, atelectasis, and respiratory failure among the patients participating in the experiment (p>0.005) as shown in Table 6.
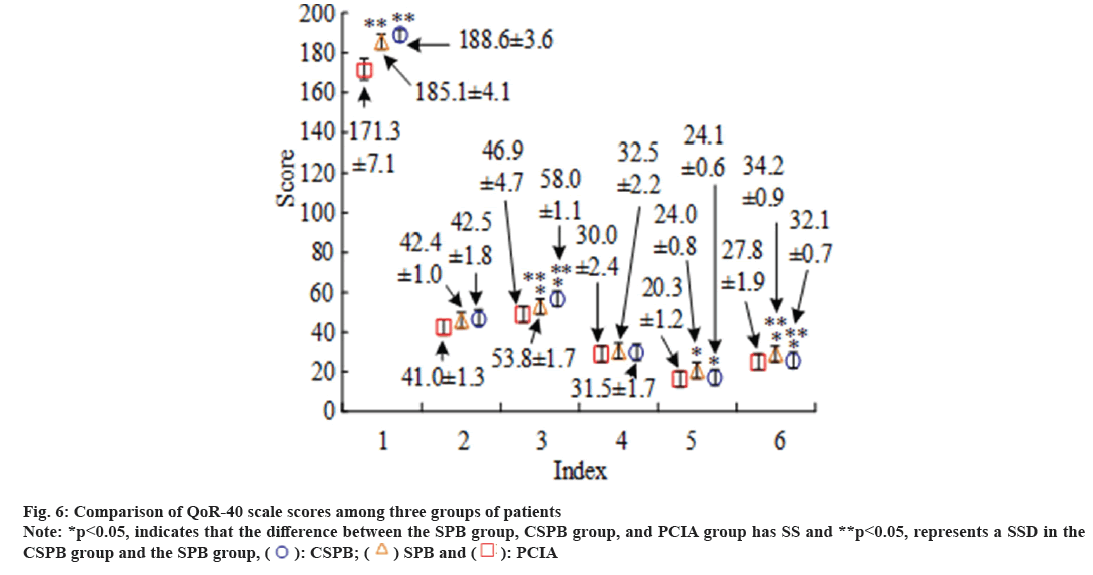
In the comparing of Ramsay sedation scores among the patients participating in the experiment, the values of PCIA group at T1 to T5 time points were 2.31±0.41, 2.52±0.40, 2.71±0.55, 3.62±0.53, and 4.01±0.51, respectively; the SPB group was 2.15±0.34, 2.25±0.37, 2.39±0.51, 3.33±0.48, and 2.85±0.45, respectively; the CSPB group was 2.22±0.36, 2.48±0.39, 2.64±0.52, 3.57±0.50, and 3.91±0.47, respectively. Overall, the disparities between the three groups do not have SS (p>0.05), while the disparities between time points within the group have SS (p<0.05), indicating that the Ramsay scores of the patients participating in the experiment continued to increase with the increase of postoperative time. The difference between groups and time points does not have SS (p>0.05) as shown in fig. 7.
In the comparing of cognitive function among patients participating in the experiment, the main comparison was the Mini-Mental State Examination (MMSE) score and the occurrence of cognitive adverse reactions. In the comparison of MMSE scores, the MMSE scores of the patients participating in the experiment illustrated a trend of first decreasing and then increasing, and all began to increase after the 1st d. Relative to the PCIA group, the CSPB group and SPB group showed a smaller decrease, and the disparity has SS (p<0.05). Overall, the disparities among patients participating in the experiment before surgery do not have SS (p>0.05), while the disparities among patients participating in the experiment AS have SS (p<0.05) as shown in Table 7.
| Comparison of PACU among three groups of patients | Comparison of postoperative complications | |||||
|---|---|---|---|---|---|---|
| PACU stay time | Calm and restless rating | Hospital stay | Incidence of pulmonary infections | Incidence of atelectasis | Respiratory failure incidence rate | |
| PCIA | 53.42±0.81ab | 5.12±0.18b | 15.72±0.82 | 3 (6.67 %) | 2 (3.33 %) | 2 (3.33 %) |
| CSPB | 41.49±1.04ab | 4.29±0.09 | 13.86±0.90 | 2 (3.33 %) | 2 (3.33 %) | 0 (0 %) |
| SPB | 36.89±0.85a | 4.06±0.04a | 11.79±0.87a | 2 (3.33 %) | 2 (3.33 %) | 0 (0 %) |
| p | <0.05 | <0.05 | <0.05 | >0.05 | >0.05 | >0.05 |
Note: ap<0.05 represents, relative to the PCIA group and bp<0.05 represents, relative to the SPB group
Table 6: Comparison of PACU Stay Time, Sedation and Restlessness Scores, Hospital Stay, and Postoperative Complications among three Groups of Patients
| T0 | T1 | T2 | T3 | T4 | T5 | T6 | |
|---|---|---|---|---|---|---|---|
| PCIA | 29.09±0.84 | 28.45±0.65 | 26.16±1.01 | 25.32±0.85 | 23.69±0.14 | 22.32±1.57 | 24.24±1.18 |
| CSPB | 29.06±0.77 | 28.11±1.12 | 27.69±0.69 | 26.14±0.45 | 25.55±1.18 | 24.96±0.14 | 25.88±0.65 |
| ap | 0.86 | 0.07 | p<0.05 | p<0.05 | p<0.05 | p<0.05 | p<0.05 |
| SPB | 29.02±0.73 | 28.95±1.21 | 27.85±0.77 | 26.64±0.64 | 25.97±1.21 | 25.44±1.31 | 26.98±1.52 |
| bp | 0.85 | 0.07 | p<0.05 | p<0.05 | p<0.05 | p<0.05 | p<0.05 |
Note: ap represents the comparing in the SPB group and the PCIA group and bp represents the comparing in the CSPB group and the PCIA group
Table 7: Comparing of Mmse Scores Among Patients Participating in the Experiment
In addition, in the comparing of adverse reactions among patients participating in the experiment, the incidence of adverse reactions in the PCIA group was 16.84 %; the incidence rates of SPB group and CAPB group were 4.08 % and 6.43 %, below those of PCIA group. The disparities among patients participating in the experiment have SS (p<0.05) (Table 8).
| Restlessness | Awakening period shiver | Respiratory depression | Hypoxemia | Adverse reaction rate | |
|---|---|---|---|---|---|
| PCIA | 2 (4.35 %) | 1 (2.08 %) | 4 (8.33 %) | 1 (2.08 %) | 0.1684 |
| SPB | 1 (2.04 %) | 0 (0 %) | 1 (2.04 %) | 0 (0 %) | 0.0408 |
| ap | 0.55 | 0.3 | 0.16 | 0.3 | <0.05 |
| CAPB | 1 (2.08 %) | 0 (0 %) | 2 (4.35 %) | 0 (0 %) | 0.0643 |
| bp | 0.56 | 0.3 | 0.4 | 0.3 | <0.05 |
Note: ap represents the comparing between the SPB group and the PCIA group and bp represents the comparing between the CSPB group and the PCIA group
Table 8: Comparison of Adverse Reactions among Patients Participating in the Experiment
The rapid recovery AS is a requirement for "quality" in today’s society and it is also a new requirement for patients and doctors in the current medical development. Its aim is to reduce the physical damage caused by surgery by suppressing stress, thereby reducing postoperative complications and shortening patient hospitalization time, to achieve rapid postoperative recovery[11,12]. In the concept of rapid recovery, the two key factors for its implementation are minimally invasive technology and fully effective pain relief, and painless management and risk-free surgery will always be the development trend in the field of surgery[13,14]. PCIA is a "self-management" treatment method for patients AS. The premise is that the anesthesiologist needs to set the corresponding background amount and injection speed in terms of the basic condition of patients. At present, the commonly used analgesia program after thoracic surgery is PCIA, which is mainly based on the infusion of opioids[15,16]. However, this conventional method is still relatively effective for patient’s pain relief at rest, but it is not useful for pain relief resulted from exercise, and often causes adverse reactions[17,18]. Currently, many studies have proven that the use of PCIA alone is no longer suitable for postoperative analgesia under thoracoscopy. The combination of various drugs and methods for multimodal analgesia has become a recognized analgesic method in the industry[19,20].
Therefore, the study quantified the management of preoperative Thoracic Paravertebral Nerve Block (TPVB) tissue, anesthesia induction medication, and postoperative analgesia, and compared SABP tissue with postoperative PCA methods and medication as variables. The experimental results showed that in the resting VAS score, the highest value in the SPB group appeared at T5, at 2.2±0.4; the highest value in the CSPB group also appeared at T5, at 2.4±0.5, both lower than the 3.1±0.5 in the PCIA group. In the sports VAS score, the highest value in the SPB group appeared at T4, at 2.7±0.6; the highest value in the CSPB group also appeared at T4, at 3.3±0.3, which was lower than 4.5±0.5 in the PCIA group. There was a SD in resting and exercise VAS scores among the patients participating in the experiment at T2, T3, T4, and T5 (p<0.05). In addition, the comparison of the first postoperative patient-controlled analgesia time among the three groups of patients showed that the PCIA group had 5 h, the SPB group had 10 h, and the CSPB group had 8 h. The MIQR values of the three groups were 2.5, 7.0, and 10.0, respectively, indicating a significant extension of the patient-controlled analgesia time in the two EG. Moreover, the value of PaCO2 in the SPB group grew at the time point of postoperative T6, with a p value of 0.03, indicating a SSD (p<0.05). Meanwhile, in the comparison of QoR-40 scale scores among the patients participating in the experiment, the total scores of SPB group and CSPB group at T6 were 185.1±4.1 and 188.6±3.6, respectively, which showed a significant improvement relative to the PCIA group. The disparities among the patients participating in the experiment have SS (p<0.05); the incidence of nausea, vomiting, and dizziness in the SPB group and CSPB group was significantly reduced relative to the PCIA group, and the disparity has SS (p<0.05). In the comparing of MMSE scores, the MMSE scores of the patients participating in the experiment indicated a trend of first decreasing and then increasing, and all began to increase after the 1st d. Relative to the PCIA group, the CSPB group and SPB group showed a smaller decrease, and the disparity has SS (p<0.05).
Overall, the analgesic effect of a single ASM plane block combined with patient-controlled intravenous analgesia mode is the best, and it can also reduce the incidence of adverse reactions caused by the total use of opioid drugs, resulting in high patient comfort. However, due to the fact that necessary double blind experiments were not conducted in actual work when studying the randomized controlled method, there is a possibility of improving the error. Therefore, additional double blind experiments are needed in the future.
Funding:
This work was supported by Key Scientific and Technological Research Program of Health Commission of Hebei Province for Effect of General Anesthesia Combined with Serratus Anterior Block on Cognitive Function in Patients after Pulmonary Lobectomy (No. 20220579).
Conflict of interests:
The authors declared no conflict of interests.
References
- Luan TM, Bang HT, Vuong NL, Dung LT, Tin NT, Tien TQ, et al. Long-term outcomes of video-assisted lobectomy in non-small cell lung cancer. Asian Cardiovasc Thoracic Ann 2021;29(4):318-26.
[Crossref] [Google Scholar] [PubMed]
- Masood F, Masood J, Zahir H, Driss K, Mehmood N, Farooq H. Novel approach to evaluate classification algorithms and feature selection filter algorithms using medical data. J Comp Cognit Eng 2023;2(1):57-67.
- Feray S, Lubach J, Joshi GP, Bonnet F, van de Velde M, Joshi GP, et al. PROSPECT guidelines for video-assisted thoracoscopic surgery: A systematic review and procedure-specific postoperative pain management recommendations. Anaesthesia 2022;77(3):311-25.
[Crossref] [Google Scholar] [PubMed]
- Aiolfi A, Nosotti M, Micheletto G, Khor D, Bonitta G, Perali C, et al. Pulmonary lobectomy for cancer: Systematic review and network meta-analysis comparing open, video-assisted thoracic surgery, and robotic approach. Surgery 2021;169(2):436-46.
[Crossref] [Google Scholar] [PubMed]
- Kiblawi R, Zoeller C, Zanini A, Ure BM, Dingemann J, Kuebler JF, et al. Video-assisted thoracoscopic or conventional thoracic surgery in infants and children: Current evidence. Eur J Pediatr Surg 2020;31(1):54-64.
[Crossref] [Google Scholar] [PubMed]
- Chen WC, Bai YY, Zhang LH, Liu YB, Liu CY, Liang JW, et al. Prevalence and predictors of chronic postsurgical pain after video-assisted thoracoscopic surgery: A systematic review and meta-analysis. Pain Ther 2023;12(1):117-39.
[Crossref] [Google Scholar] [PubMed]
- Xie D, Deng J, Gonzalez-Rivas D, Zhu Y, Jiang L, Jiang G, et al. Comparison of video-assisted thoracoscopic surgery with thoracotomy in bronchial sleeve lobectomy for centrally located non–small cell lung cancer. J Thorac Cardiovasc Surg 2021;161(2):403-13.
[Crossref] [Google Scholar] [PubMed]
- Selim J, Jarlier X, Clavier T, Boujibar F, Dusséaux MM, Thill J, et al. Impact of opioid-free anesthesia after video-assisted thoracic surgery: A propensity score study. Annal Thorac Surg 2022;114(1):218-24.
[Crossref] [Google Scholar] [PubMed]
- Rice D, Rodriguez-Restrepo A, Mena G, Cata J, Thall P, et al. Matched pairs comparison of an enhanced recovery pathway vs. conventional management on opioid exposure and pain control in patients undergoing lung surgery. Ann Surg 2021;274(6):1099-106.
[Crossref] [Google Scholar] [PubMed]
- Wei X, Yu H, Dai W, Xu W, Yu Q, Pu Y, et al. Discrepancy in the perception of symptoms among patients and healthcare providers after lung cancer surgery. Support Care Cancer 2022;30(2):1169-79.
[Crossref] [Google Scholar] [PubMed]
- Ljungqvist O, de Boer HD, Balfour A, Fawcett WJ, Lobo DN, Nelson G, et al. Opportunities and challenges for the next phase of enhanced recovery after surgery: A review. JAMA Surg 2021;156(8):775-84.
[Crossref] [Google Scholar] [PubMed]
- Bisch SP, Jago CA, Kalogera E, Ganshorn H, Meyer LA, Ramirez PT, et al. Outcomes of enhanced recovery after surgery (ERAS) in gynecologic oncology–A systematic review and meta-analysis. Gynecol Oncol 2021;161(1):46-55.
[Crossref] [Google Scholar] [PubMed]
- Stenberg E, dos Reis Falcao LF, O’Kane M, Liem R, Pournaras DJ, Salminen P, et al. Guidelines for perioperative care in bariatric surgery: Enhanced recovery after surgery (ERAS) society recommendations: A 2021 update. World J Surg 2022;46(4):729-51.
[Crossref] [Google Scholar] [PubMed]
- Mancel L, van Loon K, Lopez AM. Role of regional anesthesia in Enhanced Recovery after Surgery (ERAS) protocols. Curr Opin Anesthesiol 2021;34(5):616-25.
[Crossref] [Google Scholar] [PubMed]
- Dai L, Ling X, Qian Y. Effect of ultrasound-guided trans vs. abdominis plane block combined with patient-controlled intravenous analgesia on postoperative analgesia after laparoscopic cholecystectomy: A double-blind, randomized controlled trial. J Gastrointest Surg 2022;26(12):2542-50.
[Crossref] [Google Scholar] [PubMed]
- Heo MH, Kim JY, Kim JH, Kim KW, Lee SI, Kim KT, et al. Epidural analgesia vs. intravenous analgesia after minimally invasive repair of pectus excavatum in pediatric patients: A systematic review and meta-analysis. Korean J Anesthesiol 2021;74(5):449-58.
[Crossref] [Google Scholar] [PubMed]
- Xiao YK, She SZ, Xu LX, Zheng B. Serratus anterior plane block combined with general analgesia and patient-controlled serratus anterior plane block in patients with breast cancer: A randomized control trial. Adv Ther 2021;38(6):3444-54.
[Crossref] [Google Scholar] [PubMed]
- Lin R, Lin S, Feng S, Wu Q, Fu J, Wang F, et al. Comparing patient-controlled analgesia vs. non-PCA hydromorphone titration for severe cancer pain: A randomized phase III trial. J Natl Compr Cancer Netw 2021;19(10):1148-55.
[Crossref] [Google Scholar] [PubMed]
- Bliss Jr DP, Strandness TB, Derderian SC, Kaizer AM, Partrick DA. Ultrasound-guided erector spinae plane block vs. thoracic epidural analgesia: Postoperative pain management after Nuss repair for pectus excavatum. J Pediatr Surg 2022;57(2):207-12.
[Crossref] [Google Scholar] [PubMed]
- Wasfy SF, Kamhawy GA, Omar AH, Abd El Aziz HF. Bilateral continuous erector spine block vs. multimodal intravenous analgesia in coronary bypass surgery. A randomized trial. Egypt J Anaesth 2021;37(1):152-8.

 analgesia frequency
analgesia frequency