- *Corresponding Author:
- Liqiao Chi
Department of Dermatology, Qingpu Branch of Zhongshan Hospital Affiliated to Fudan University, Qingpu, Shanghai 201700, China
E-mail: clq202309@163.com
| This article was originally published in a special issue, “Exploring the Role of Biomedicine in Pharmaceutical Sciences” |
| Indian J Pharm Sci 2024:86(1) Spl Issue “173-181” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
To investigate the effects of 5-aminolevulinic acid photodynamic therapy on serum interleukin-6, interleukin-21, interleukin-23 and T cells 17/regulatory T cell balance in moderate to severe acne patient. 70 patients with moderate to severe acne who visited our dermatology outpatient clinic from January 2023 to August 2023 were selected as the research object and were divided into the experiment group (n=35) and the control group (n=35); the experiment group were treated with 5-aminolevulinic acid-based photodynamic therapy, while the control group was given 1 mg/bid isotretinoin capsules. The patients of the two groups were treated for 6 w; enzyme-linked immunosorbent assay to detect the serum interleukin-6, interleukin-21 and interleukin-23 level. Flow cytometry to detect the percentage of helper T cells 17 and regulatory T cell. Statistical Package for the Social Sciences software to analyze the spearman correlation between interleukin-6, interleukin-21, and interleukin-23 level with T cells 17/regulatory T cell balance. There were no statistical difference in the comparison of general information between the experiment and control groups (p>0.05). The therapeutic effect of the experiment group was more than the control group (p<0.05). Before treatment, serum interleukin-6, interleukin-21, and interleukin-23 levels have no statistical difference (p>0.05) between the two groups. After treatment, there were no statistical difference in serum interleukin-6, interleukin-21 and interleukin-23 levels (p>0.05). Serum interleukin-6, interleukin-21 levels were positive correlation with regulatory T cell/T cells 17 balance, while interleukin-23 levels were negative correlation with regulatory T cell/T cells 17 balance. Serum interleukin-6, interleukin-21, interleukin-23 level and peripheral blood T cells 17/regulatory T cell balance were associated to the therapeutic effect of moderate and severe acne patients after treatment. 5-aminolevulinic acid-based photodynamic therapy significantly improved the therapeutic effect of moderate and severe acne, but had no effect on serum interleukin-6, interleukin-21, interleukin-23 and peripheral blood T cells 17/regulatory T cell balance.
Keywords
Acne, 5-aminolevulinic acid photodynamic therapy, interleukin-6, interleukin-21, interleukin-23, T regulatory cell/T cells 17 balance
Acne is a commonly seen chronic inflammatory disease of follicular sebaceous glands, which occurs in sebaceous gland-rich areas. As a multifactorial skin disease, the incidence of acne is as high as 39.2 % among adolescents and adults in mainland China[1]. With improving living standards and changes in dietary habits, there is a growing trend in the incidence of acne[2]. Moderate to severe acne, characterized by pustules, cysts, and nodules, can lead to pigmentation and disfiguring scars, causing significant psychological distress and adversely affecting the life quality and mental well-being of patients. For moderate to severe acne, clinical management often involves the systemic use of antibiotics and retinoids[3]. However, concerns about the adverse effects of retinoic acid preparations and the impact on fertility in men and women of childbearing age, as well as the continued emergence of antibiotic resistance, have limited the use of retinoic acid preparations and antibiotics[4].
5-Aminolevulinic Acid-Photodynamic Therapy (5-ALA-PDT) has gradually emerged as a treatment modality for moderate to severe acne and has shown certain clinical efficacy[5,6], but the mechanism of its action, especially the immunological mechanism, has not been fully elucidated. Some study suggests that the functional interplay between helper T Cells 17 (Th17) and Regulatory T Cells (Treg), with their mutual antagonism, in maintaining body immune homeostasis plays a pivotal role. Their imbalance leads the transitional activation of Th17 cells, which is the key to the pathogenesis of acne[7]. Th17 cells contribute to the development of acne by secreting various cytokines[8], whereas Treg cells secrete a variety of anti-inflammatory cytokines to prevent excessive inflammatory response and reduce its damage to body functions[9].
Inflammatory factors in the immune response play a very crucial role. Interleukin (IL)-6 belongs to pro-inflammatory factors, which inhibits Treg cell differentiation and T cell apoptosis by activating the immune system, recruiting monocytes, stimulating endothelial and smooth muscle cell expression[10]; IL-21 is mainly synthesized and secreted by Natural Killer (NK) cells and activated Cluster of Differentiation (CD) 4+ T cells, regulates various immune responses by affecting multiple immune cells[11]; IL-23 primarily acts on Th17 cells, in Th17 cells proliferation and stability playing a crucial role. It can also promote the production of cytokines in Th17 cells, participating in the progression of various diseases[12].
Given these factors, this investigate aims to assess the change of serum IL-6, IL-21, IL-23, and peripheral blood Treg/Th17 cell balance in patient with moderate to severe acne before and after 5-ALA-PDT treatment. This research aims to gain further insight into the immunological mechanisms of 5-ALA-PDT treatment for moderate to severe acne, providing an experiment basis and theoretical support for treatment of moderate to severe acne.
Materials and Methods
Materials:
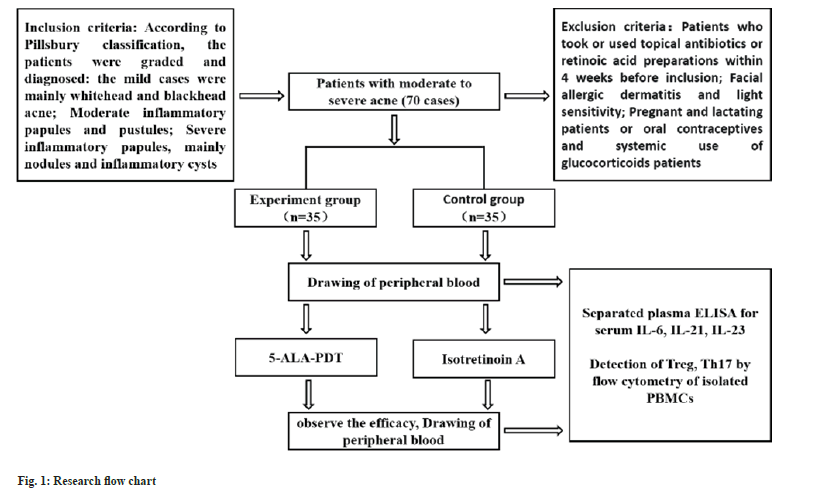
After approval by the hospital Medical Ethics Committee, 70 moderate to severe acne patients who visited the dermatology outpatient clinic at our hospital from January 2023 to August 2023 were selected as study subject. They were divided into a control group and experiment group, each consisting of 35 patients. The study workflow is depicted in fig. 1.
Inclusion and exclusion criteria:
Inclusion criteria: Refer to Pillsbury classification for grading and diagnosing the patients; in mildly, whiteheads and blackhead pimples predominate; in moderately, inflammatory papules and pustules predominate and in severely, inflammatory papules with nodules and inflammatory cysts predominate.
Exclusion criteria: Patients who took or used antibiotics and retinoic acid preparations within 4 w before enrollment; patients with facial atopic dermatitis and photosensitivity; patients who were pregnant and lactating or taking oral contraceptives and patients with systematic application of glucocorticoids. The control group should also exclude patients with hyperlipidemia, liver and kidney function abnormalities.
Treatment:
The control group was given 10 mg bid isotretinoin capsules for 6 w. The experiment group was given 5-ALA-PDT: first, the lesions were pretreated with sterile disposable needles, then fresh gel was used to make 5 % Aminolevulinic Acid (ALA) gel, which was evenly applied to the lesions, sealed with plastic wrap, and then irradiated with laser light at a wavelength of 635 nm for 60 min after avoiding the light for 30 min, with the total energy of the laser light being 126 J/cm2, and the area not easily reached was irradiated additionally for 20 min. The total laser energy was 126 J/cm2, and for the areas not easily reached by light, supplemental irradiation was performed for 20 min, once every 2 w, and the treatment was stopped after healing.
Evaluation of efficacy:
The assessment of lesion improvement was categorized as follows; ≥90 % reduction in lesions was classified as “cured”; 70 %-89 % reduction was classified as "excellent effective"; 30 %-69 % reduction was classified as "improved" and <30 % reduction or worsening was classified as "ineffective".
Detection of serum IL-6, IL-21 and IL-23 levels:
Before each treatment, take 3 ml of fasting venous blood from patients in the early morning by using heparin anticoagulation tube, centrifuged at 3000 rpm for 15 min, take the serum preserved at -80°. The serum was measured the level of IL-6, IL- 21, and IL-23 by Enzyme-Linked Immunosorbent Assay (ELISA).
Peripheral blood Treg and Th17 cell ratio assay:
Single nucleated cells were separated from the remaining blood cells using lymphocyte isolation solution, and 1640 complete culture solution with 10 % fetal bovine serum, ionomycin (10 ng/ml), add Phorbol Myristate Acetate (PMA) (1 μM) sequentially, culture in incubator at 37°, 5 % Carbon dioxide (CO2), protected from light for 3 h, then add Blefeldin A (10 mg/ml), continue culture for 1 h, and the incubation was terminated.
Cell staining: Complete stimulation of Peripheral Blood Mononuclear Cell (PBMC) was mixed with Fluorescein Isothiocyanate (FITC)-CD4, Peridinin Chlorophyll Protein (PerCP)-CD3 antibody, culture for 20 min at room temperature under light protection, washed twice use phosphate buffer, fixed with fixation rupture agent, ruptured the membrane and added PE-IL-10, APC-foxp3, PE-Cy5-IL-17, PE-Cy7-IL23, incubated at room temperature under light protection for 20 min and washed twice. Using flow cytometry, 10 000 cells were acquired with cell quest software for analysis, and the results were expressed as percentages.
Flow data analysis: BD Software Cell Quest can be used to analyze, first CD4 circle gate to analyze the CD4+ T cell subpopulation, followed by labeling the Treg cell subpopulation with CD25, foxp3, and combining with IL-10 for the detection of Treg cytokine secretion function; after the CD3 and CD4 circle gates, the percentage of IL-17 and IL-23 in CD4+ T cells were detected, which is the Th17 cells.
Statistical methods:
By Statistical Package for the Social Sciences (SPSS) 26.0 statistical analysis software analyze data. For measurement data, difference between groups were compared used t-test, result was presented as x̄ ±s. For count data, difference between group were compared used the Chi Square (χ2) test, result was presented as n (%); p<0.05 represents statistical significance.
Results and Discussion
Age, gender, duration of disease, family history, degree of disease, cumulative site and clinical manifestations of patients were analyzed for differences in experiment group and control group. The findings showed the two group have no statistical difference (p>0.05) (Table 1), which means that the grouping was reasonable and the results after treatment were comparable.
| Indicator | Experiment group (n=35) | Control group (n=35) | t/χ2 | p |
|---|---|---|---|---|
| Gender | 0.058 | 0.81 | ||
| Male | 15 (42.9) | 16 (45.7) | ||
| Female | 20 (57.1) | 19 (54.3) | ||
| Age | 22.06±2.485 | 21.11±3.488 | -1.303 | 0.198 |
| Duration of disease (months) | 18.23±2.129 | 17.63±2.276 | -1.139 | 0.259 |
| Family history | 0.108 | 0.743 | ||
| No | 29 (82.9) | 30 (85.7) | ||
| Yes | 6 (17.1) | 5 (14.3) | ||
| Degree of disease | 0.062 | 0.803 | ||
| Moderate | 13 (37.1) | 12 (34.3) | ||
| Severe | 22 (62.9) | 23 (65.7) | ||
| Cumulative area | 0.791 | 0.852 | ||
| Cheeks | 11 (31.4) | 14 (40) | ||
| Nose | 12 (34.3) | 12 (34.3) | ||
| Frontal | 8 (22.9) | 6 (17.1) | ||
| Perioral | 4 (11.4) | 3 (8.6) | ||
| Clinical manifestations | 0.265 | 0.876 | ||
| Pustules | 12 (34.3) | 10 (28.6) | ||
| Cysts | 11 (31.4) | 12 (34.3) | ||
| Nodules | 12 (34.3) | 13 (37.1) |
Table 1: Comparison of general information of Patients in the experiment group gnd control group
In order to investigate purpose, the effectiveness of 5-ALA-PDT therapy treating moderate to severe acne, firstly, we compared the experiment and control group effective rate at different time points, which showed that, in experiment group the effective rate was greater than the control group at the 2nd and 4th w (p<0.05), and no significant difference between the experiment and control group in the effectiveness at 6 w (p>0.05), no difference between the two groups in the total efficiency (p>0.05) (Table 2). To further compare the efficacy between experiment and control group at different time point, result showed that between the two groups the difference in efficacy at w 2, 4 and 6 was no significant difference, while the experiment group total effectiveness was remarkably better than the control group (p<0.05) (Table 3).
| Time | Group | Number of people | Effective | Ineffective | Effective rate | χ2 | p |
|---|---|---|---|---|---|---|---|
| 2 w | Experiment | 35 | 15 | 20 | 42.86 | 4.242 | 0.039 |
| Control | 35 | 7 | 28 | 20.00 | |||
| 4 w | Experiment | 34 | 25 | 9 | 73.53 | 5.534 | 0.019 |
| Control | 35 | 16 | 19 | 45.71 | |||
| 6 w | Experiment | 31 | 29 | 2 | 93.55 | 0.451 | 0.502 |
| Control | 34 | 29 | 5 | 85.29 | |||
| Total | Experiment | 35 | 33 | 2 | 94.43 | 0.635 | 0.426 |
| Control | 35 | 30 | 5 | 85.71 |
Table 2: Comparison of effective rate between experiment group and control group
| Time | Group | Number of people | Cured | Excellent effective | Improved | Ineffective | χ2 | p |
|---|---|---|---|---|---|---|---|---|
| 2 w | Experiment | 35 | 1 | 5 | 9 | 20 | 5.213 | 0.157 |
| Control | 35 | 0 | 2 | 5 | 28 | |||
| 4 w | Experiment | 34 | 3 | 9 | 13 | 9 | 6.235 | 0.101 |
| Control | 35 | 1 | 5 | 10 | 19 | |||
| 6 w | Experiment | 31 | 5 | 15 | 9 | 2 | 6.027 | 0.110 |
| Control | 34 | 2 | 10 | 17 | 5 | |||
| Total | Experiment | 35 | 9 | 15 | 9 | 2 | 7.976 | 0.047 |
| Control | 35 | 3 | 10 | 17 | 5 |
Table 3: Comparison of efficacy between experiment group and control group
To find out effectiveness of 5-ALA-PDT therapy on IL-6, IL-21, IL-23 level, ELISA assay was performed to measure the level of them in whole blood supernatant. The results revealed no difference between the experiment and the control group before treatment in serum IL-6, IL-21 and IL-23 levels (p>0.05); After treatment, there was no difference in the same efficacy between the experiment and control group in the serum IL-6, IL-21, IL-23 level (p>0.05); after treatment, in cured, excellent effective and improved groups the levels of serum IL-6, IL-21 were lower than before treatment (p<0.05), while compared with before treatment the level of IL-23 were higher (p<0.05); in ineffective group the serum IL-6, IL-21 ,IL- 23 level were not different from those before treatment (p>0.05) and there were differences in serum IL-6, IL-21 and IL-23 level between the same group after treatment with different curative effects group (p<0.05). The IL-6, IL-21 levels gradually decreased with the improvement of curative effect, while the levels of IL-23 gradually increased with the improvement of curative effect (Table 4-Table 6).
| Efficacy | Experiment group | Control group | |
|---|---|---|---|
| Before treatment | ~ | 110.505±26.681bcd | 105.599±26.307bcd |
| After treatment | Cured | 22.875±4.271acde | 23.765±3.002acde |
| Excellent effective | 46.264±11.259abde | 45.017±14.291abde | |
| Improved | 79.347±12.4abce | 83.971±18.522abce | |
| Ineffective | 105.55±5.67bcd | 102.472±5.348bcd |
Note: ap<0.05, comparison of pre-treatment with the same group; bp<0.05, comparison of cure with the same group; cp<0.05, comparison of apparent effect with the same group; dp<0.05, comparison of improvement with the same group and ep<0.05, comparison of ineffectiveness with the same group
Table 4: Comparison of Serum Il-6 (Ng/L) levels between experiment Group and control group
| Efficacy | Experiment group | Control group | |
|---|---|---|---|
| Before treatment | ~ | 259.031±28.545bcd | 263.926±22.688bcd |
| After treatment | Cured | 38.614±4.144acde | 38.946±3.603acde |
| Excellent effective | 126.171±12.793abde | 132.911±8.706abde | |
| Improved | 201.432±23.184abce | 197.653±±20.003abce | |
| Ineffective | 257.865±19.169bcd | 255.320±11.501bcd |
Note: ap<0.05, comparison of pre-treatment with the same group; bp<0.05, comparison of cure with the same group; cp<0.05, comparison of apparent effect with the same group; dp<0.05, comparison of improvement with the same group and ep<0.05, comparison of ineffectiveness with the same group
Table 5: Comparison of Serum Il-21 (Ng/L) levels between experiment group and control group
| Efficacy | Experiment group | Control group | |
|---|---|---|---|
| Before treatment | ~ | 278.919±21.589bcd | 273.032±14.142bcd |
| After treatment | Cured | 552.726±18.871acde | 530.077±14.274acde |
| Excellent effective | 488.753±10.338abde | 484.588±11.097abde | |
| Improved | 389.338±10.174abce | 390.243±6.289abce | |
| Ineffective | 272.100±5.445bcd | 269.848±3.532bcd |
Note: ap<0.05, comparison of pre-treatment with the same group; bp<0.05, comparison of cure with the same group; cp<0.05, comparison of apparent effect with the same group; dp<0.05, comparison of improvement with the same group and ep<0.05, comparison of ineffectiveness with the same group
Table 6: Comparison of Serum Il-23 (Ng/L) levels between experiment group and control group
For investigate the effectiveness of 5-ALAPDT therapy on Treg/Th17 balance, the Treg, Th17 percentages of in blood cells were detected used flow cytometry, Treg/Th17 values were calculated. The result showed that before treatment, hasn't difference in Treg, Th17 and Treg/Th17 between the experiment group and the control group (p>0.05); after treatment, the experiment group and the control group had the same efficacy there was no difference in Treg, Th17, Treg/Th17 (p>0.05); After treatment, Th17 was higher than before treatment in the cured, excellent effective and improved group (p<0.05), compared with before treatment, the Treg, Treg/Th17 was lower (p<0.05), compared with the before treatment, there was no difference between Treg, Th17, Treg/Th17 in the ineffective group (p>0.05); there was a significant difference in Treg, Th17, Treg/Th17 among different efficacy group after treatment among the same group (p<0.05), and Treg and Treg/Th17 gradually decreased, while Th17 gradually increased with the improvement of the efficacy (Table 7-Table 9).
| Efficacy | Experiment group | Control group | |
|---|---|---|---|
| Before treatment | ~ | 4.391±0.765bcd | 4.353±0.806bcd |
| After treatment | Cured | 2.041±0.152acde | 2.017±0.204acde |
| Excellent effective | 2.852±0.251abde | 2.852±0.364abde | |
| Improved | 3.682±0.288abce | 3.640±0.384abce | |
| Ineffective | 4.445±0.403bcd | 4.454±0.282bcd |
Note: ap<0.05, comparison of pre-treatment with the same group; bp<0.05, comparison of cure with the same group; cp<0.05, comparison of apparent effect with the same group; dp<0.05, comparison of improvement with the same group and ep<0.05, comparison of ineffectiveness with the same group
Table 7: Comparison of Treg Percent changes between experiment group and control group
| Efficacy | Experiment group | Control group | |
|---|---|---|---|
| Before treatment | ~ | 1.071±0.136bcd | 1.088±0.183bcd |
| After treatment | Cured | 1.460±0.0332acde | 1.453±0.050acde |
| Excellent effective | 1.329±0.061abce | 1.329±0.060abce | |
| Improved | 1.211±0.057abce | 1.202±0.032abce | |
| Ineffective | 1.090±0.0848bcd | 1.080±0.0436bcd |
Note: ap<0.05, comparison of pre-treatment with the same group; bp<0.05, comparison of cure with the same group; cp<0.05, comparison of apparent effect with the same group; dp<0.05, comparison of improvement with the same group and ep<0.05, comparison of ineffectiveness with the same group
Table 8: Comparison of Th17 percent changes between experiment group and control group
| Efficacy | Experiment group | Control group | |
|---|---|---|---|
| Before treatment | ~ | 4.246±1.252bcd | 4.242±1.558bcd |
| After treatment | Cured | 1.399±0.117acde | 1.391±0.187acde |
| Excellent effective | 2.150±0.207abce | 2.155±0.331abce | |
| Improved | 3.044±0.248abce | 3.029±0.335abce | |
| Ineffective | 4.105±0.689bcd | 4.122±0.145bcd |
Note: ap<0.05, comparison of pre-treatment with the same group; bp<0.05, comparison of cure with the same group; cp<0.05, comparison of apparent effect with the same group; dp<0.05, comparison of improvement with the same group and ep<0.05, comparison of ineffectiveness with the same group
Table 8: Comparison of Th17 percent changes between experiment group and control group
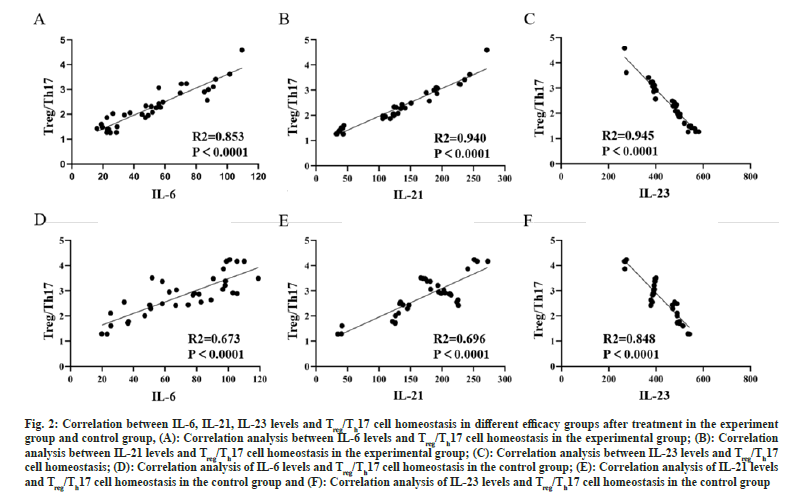
In order to investigate whether there is a correlation between IL-6, IL-21, IL-23 levels and Treg/Th17 cell balance, spearman correlation analysis was done by SPSS statistical analysis software analysis. The result showed that serum IL-6, IL-21 level were positive correlated with Treg/Th17 cell homeostasis in both experiment groups and control groups, while IL-23 levels were negative correlated with Treg/Th17 cell homeostasis (fig. 2).
Fig. 2: Correlation between IL-6, IL-21, IL-23 levels and Treg/Th17 cell homeostasis in different efficacy groups after treatment in the experiment group and control group, (A): Correlation analysis between IL-6 levels and Treg/Th17 cell homeostasis in the experimental group; (B): Correlation analysis between IL-21 levels and Treg/Th17 cell homeostasis in the experimental group; (C): Correlation analysis between IL-23 levels and Treg/Th17 cell homeostasis; (D): Correlation analysis of IL-6 levels and Treg/Th17 cell homeostasis in the control group; (E): Correlation analysis of IL-21 levels and Treg/Th17 cell homeostasis in the control group and (F): Correlation analysis of IL-23 levels and Treg/Th17 cell homeostasis in the control group
Photodynamic Therapy (PDT) is used to treat various types of location-related cancers and non-tumor diseases by applying a photosensitizer externally and then irradiating locally with a specific wavelength of light, after absorbing light, photosensitizers react with oxygen in a series ways, and play a therapeutic role through cytotoxic effects or intentional cell biological behaviors[13]. 5-amino-ketovalerate has become a commonly used photosensitizer due to its advantages of easy synthesis, easy local use and easy absorption[14]. More and more studies have shown that 5-ALAPDT can treat various skin diseases, such as refractory condyloma acuminatum[15], diabetic foot ulcer infection[16], and psoriasis[17]. Moderate and severe acne is also a kind of skin disease with multiple and severe skin lesions and easy to leave pigmentation and scars. This research revealed that the experiment group therapeutic efficacy was significantly more favorable than the control group, which indicated that ALA-PDT was effectively treat moderate to severe acne, which was in line with Zhang et al.[18] findings.
Some studies had shown that 5 % ALA-PDT therapies in treatment of acne are clinically effective, which is conducive to the improvement of skin lesion symptom in patients, and at the same time, it can significantly reduce patient’s serum IL- 1β, IL-6, and CRP levels[19]. It has also been shown that 5-ALA-PDT has good efficacy in patients with high-risk Human Papilloma Virus (HPV) infection with condyloma acuminatum, which can increase serum IL-17, IL-23 level, reduce IL-10 level[20]. However, in this study, it was found that, there were no difference in the IL-6, IL-21, IL- 23 level in the same efficacy group between the experiment and control group after treatment, there were difference in IL-6, IL-21, IL-23 level between same group with different efficacies after treatment, which indicated that the 5-ALAPDT treatment did not affect the inflammatory factor levels, the inflammatory factor level were related to the efficacy of treatment, which was in contradiction to the findings of other scholars as mentioned above. Results of the study, which contradicts the results of other scholars mentioned above. Since 5-ALA-PDT therapy can improve the efficacy, there are differences in the inflammatory factor level in different efficacies group, and the inflammatory factor level were not grouped by efficacy to be compared after treatment in their study, which may be the reason for the contradictory results.
Th17 cell are a new identified subpopulation of T cell that secrete IL-17[21]; in the immune system Treg cells are fundamental cells and belong to a class of CD4+ T cell subpopulations with low proliferative capacity[22]. Th17 cells, Treg cells are derived from the same precursor cells, they require tumor growth factor-Beta (β) signaling to initial differentiation[23]. Eventually differentiation cells perform contrary functions: Th17 cells induce inflammation and autoimmunity, while Treg cells suppress these processes, maintain immune homeostasis[23]. With the increasing research on these two types of cells, relevant studies have reported that abnormalities in Treg/Th17 cell balance in the development of inflammatory diseases play a crucial role[21,24]. The finding of this study indicated that the Treg/Th17 ratio in cured, efficacious, improved groups after treatment was smaller than before treatment, as well as the Treg/ Th17 ratio after treatment gradually reduced with the improvement of the efficacy of the treatment, suggesting the Treg/Th17 cells imbalance is involved in the moderate to severe acne development, which is in line with the findings of other scholars mentioned in the previous section. After treatment, there was no difference in the Treg/Th17 ratio in the same efficacy between two group, suggesting that 5-ALA-PDT therapy did not affect the Treg/Th17 cell balance.
In conclusion, serum IL-6, IL-21, IL-23 level and peripheral blood Treg/Th17 cell balance were associated with post-treatment efficacy in moderate to severe acne patient. 5-ALA-PDT therapy significantly improved the therapeutic effect of moderate and severe acne, but has no effect on patient’s serum IL-6, IL-21, IL-23 level and peripheral blood Treg/Th17 cell balance. Because of the limited numbers of cases collected in this research, the sensitivity of individual patients to external drugs is different, and the influence of multiple factors such as lesion site, quantity, drug concentration and treatment time, it is necessary to conduct a high quality, multicenter, large sample randomized double-blind controlled experiment for verification.
In addition, the combination of ALA-PDT treatment with acne medications may greatly improve the treatment outcome, after permitting further research. Serum IL-6, IL-21, IL-23 level and peripheral blood Treg/Th17 cell balance were associated with post-treatment efficacy in moderate to severe acne patient. 5-ALA-PDT therapy significantly improved the therapeutic effect of moderate and severe acne, but has no effect on patient’s serum IL-6, IL-21, IL-23 level and peripheral blood Treg/Th17 cell balance.
Funding:
The work was supported by Qingpu District Science and Technology Development Fund Project of Yangtze River Delta Digital Trunk Line (QKY2023-14).
Conflict of interests:
The authors declared no conflict of interests.
References
- Li D, Chen Q, Liu Y, Liu T, Tang W, Li S. The prevalence of acne in mainland China: A systematic review and meta-analysis. BMJ Open 2017;7(4):e015354.
[Crossref] [Google Scholar] [PubMed]
- Chen L, Huang X, Xiao Y, Su J, Shen M, Chen X. Prevalence and risk factors of atopic dermatitis, psoriasis, acne and urticaria in China. Zhong Nan Da Xue Xue Bao 2020;45(4):449-55.
[Crossref] [Google Scholar] [PubMed]
- Working group for acne diseases, Chinese society of dermatology. Guideline for diagnosis and treatment of acne (the 2019 revised edition). J Clin Dermatol 2019;48(9):583-8.
- LI L, Ran Y, Li J, Xiong L, Zhou G, Zhang Y, et al. Topical retinoids for acne vulgaris-efficacy and safety: A systematic review. Chin J Dermatol 1995;7:12-5.
- Chen X, Song H, Chen S, Zhang J, Niu G, Liu X. Clinical efficacy of 5-aminolevulinic acid photodynamic therapy in the treatment of moderate to severe facial acne vulgaris. Exp Ther Med 2015;10(3):1194-8.
[Crossref] [Google Scholar] [PubMed]
- Zhang LL, Wang XL. 5-aminolevulinic acid photodynamic therapy in the treatment of moderate to severe acne: Review and update of therapeutic mechanism. Dermatol Bull 2022;39(1):45-9.
- Melnik BC, John SM, Chen W, Plewig G. T helper 17 cell/regulatory T-cell imbalance in hidradenitis suppurativa/acne inversa: The link to hair follicle dissection, obesity, smoking and autoimmune comorbidities. Br J Dermatol 2018;179(2):260-72.
[Crossref] [Google Scholar] [PubMed]
- Mias C, Mengeaud V, Bessou-Touya S, Duplan H. Recent advances in understanding inflammatory acne: Deciphering the relationship between Cutibacterium acnes and Th17 inflammatory pathway. J Eur Acad Dermatol Venereol 2023;37:3-11.
[Crossref] [Google Scholar] [PubMed]
- Firlej E, Kowalska W, Szymaszek K, Rolinski J, Bartosinska J. The role of skin immune system in acne. J Clin Med 2022;11(6):1579.
[Crossref] [Google Scholar] [PubMed]
- Tanaka T, Narazaki M, Kishimoto T. Interleukin (IL-6) immunotherapy. Cold Spring Harbor Perspect Biol 2018;10(8):a028456.
[Crossref] [Google Scholar] [PubMed]
- Ren HM, Lukacher AE, Rahman ZS, Olsen NJ. New developments implicating IL-21 in autoimmune disease. J Autoimmun 2021;122:102689.
[Crossref] [Google Scholar] [PubMed]
- Liu T, Li S, Ying S, Tang S, Ding Y, Li Y, et al. The IL-23/IL-17 pathway in inflammatory skin diseases: From bench to bedside. Front Immunol 2020;11:594735.
[Crossref] [Google Scholar] [PubMed]
- Rkein AM, Ozog DM. Photodynamic therapy. Dermatol Clin 2014;32(3):415-25.
[Crossref] [Google Scholar] [PubMed]
- Kwiatkowski S, Knap B, Przystupski D, Saczko J, Kędzierska E, Knap-Czop K, et al. Photodynamic therapy–mechanisms, photosensitizers and combinations. Biomed Pharmacother 2018;106:1098-107.
[Crossref] [Google Scholar] [PubMed]
- Zhang L, Zeng Q, Li J, Chen N, Tang H, Lei X, et al. ALA-PDT combined with oral acitretin in the treatment of refractory condyloma acuminatum in anal canal. Photodiagnosis Photodyn Ther 2022;40:103048.
[Crossref] [Google Scholar] [PubMed]
- Li X, Kou H, Zhao C, Zhu F, Yang Y, Lu Y. Efficacy and safety of ALA-PDT in treatment of diabetic foot ulcer with infection. Photodiagnosis Photodyn Ther 2022;38:102822.
[Crossref] [Google Scholar] [PubMed]
- Yi F, Zheng X, Fang F, Zhang J, Zhou B, Chen X. ALA-PDT alleviates the psoriasis by inhibiting JAK signalling pathway. Exp Dermatol 2019;28(11):1227-36.
[Crossref] [Google Scholar] [PubMed]
- Zhang Y, Wu H, Tu C, Sun Y, Xiao B, Guo H, et al. The assessment of psychology, quality of life in acne patients and evaluation of ALA-PDT for moderate to severe acne. Photodiagn Photodyn Ther 2021;33:102099.
[Crossref] [Google Scholar] [PubMed]
- Gao CY, Qian Q, Shen YH. Effects of photodynamic therapy with 5-aminolevulinic acid on skin lesion, IL-1β, IL-6 and CRP levels in patients with acne. Hebei Med J 2019;41(18):2840-2.
- Zhang XY, Jian JW, Dong HL. Effect of 5-aminolevulinic acid photodynamic therapy on serum IL-17, IL-23, IL-10 and Treg/Th17 cell balance in patients with condyloma acuminatum at high risk of HPV infection. Chin J Health Lab Tec 2020;30(19):2382-5.
- Yan JB, Luo MM, Chen ZY, He BH. The function and role of the Th17/Treg cell balance in inflammatory bowel disease. J Immunol Res 2020;2020:8813558.
[Crossref] [Google Scholar] [PubMed]
- Goschl L, Scheinecker C, Bonelli M. Treg cells in autoimmunity: From identification to Treg-based therapies. Semin Immunopathol 2019;1(41):301-14.
[Crossref] [Google Scholar] [PubMed]
- Lee GR. The balance of Th17 vs. Treg cells in autoimmunity. Int J Mol Sci 2018;19(3):730.
[Crossref] [Google Scholar] [PubMed]
- Thomas R, Qiao S, Yang X. Th17/Treg Imbalance: Implications in lung inflammatory diseases. Int J Mol Sci 2023;24(5):4865.
[Crossref] [Google Scholar] [PubMed]