- *Corresponding Author:
- Lin Wang
Department of Medical Genetics and Prenatal Diagnosis,
Taizhou People’s Hospital,
Taizhou,
Jiangsu 225300,
China
E-mail: 15852952922@sina.cn
| This article was originally published in a special issue, “New Advancements in Biomedical and Pharmaceutical Sciences” |
| Indian J Pharm Sci 2021:84(2) Spl Issue “246-251” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
To explore microRNA-193b-5p diagnostic value and clinical significance in hypertensive disorder complicating pregnancy. A total of 120 hypertensive disorder complicating pregnancy patients (observation group) in our hospital from January 2020 to December 2021 were enrolled was divided into three subgroups: Hypertensive disorders in pregnancy group (42 cases), mild preeclampsia group (43 cases) and severe preeclampsia group (35 cases). 120 healthy pregnant women receiving regular perinatal care were enrolled in the control group. 120 non-pregnant healthy women receiving physical examination were selected as the health control group. MicroRNA-193b-5p and neuregulin-1 levels in three groups were detected and association of microRNA-193b-5p and neuregulin-1 levels and clinical features and disease course was assessed. Receiver operating characteristic evaluated microRNA-193b-5p diagnostic value for hypertensive disorder complicating pregnancy adverse pregnancy outcomes. Serum microRNA-193b-5p and neuregulin-1 in observation group presented up-regulation relative to control group and health control group (p<0.05), while those in control group exhibited up-regulation relative to health control group (p<0.05). Serum microRNA-193b-5p and neuregulin-1 levels in the severe preeclampsia group presented up-regulation relative to mild preeclampsia group and hypertensive disorders in pregnancy group (p<0.05) and those in mild preeclampsia group presented up-regulation relative to hypertensive disorders in pregnancy group (p<0.05). Serum microRNA-193b-5p level in hypertensive disorder complicating pregnancy patients with different ages, body mass index at the time of enrollment and prognosis presented differential significance (p<0.05) and serum microRNA-193b-5p level in hypertensive disorder complicating pregnancy patients with different delivery gestational weeks, gravidity and parity presented no significance (p>0.05). Serum neuregulin-1 level in hypertensive disorder complicating pregnancy patients with different delivery gestational weeks and prognosis presented differential significance (p<0.05) and serum neuregulin-1 level in hypertensive disorder complicating pregnancy patients with different body mass index at the time of enrollment, gravidity and parity presented no significance (p>0.05). Receiver operating characteristic curve demonstrated that microRNA-193b-5p and neuregulin-1 had good predictive performance for adverse pregnancy outcomes of hypertensive disorder complicating pregnancy patients. Serum microRNA-193b-5p and neuregulin-1 play a synergistic mechanism in the onset and progression of hypertensive disorder complicating pregnancy and have association with the onset, progression and prognosis of hypertensive disorder complicating pregnancy, which can be used as valuable biomarkers for the diagnosis of hypertensive disorder complicating pregnancy.
Keywords
Hypertensive disorder complicating pregnancy, microRNA-193b-5p, neuregulin-1, diagnostic value, hypertension
Hypertensive Disorder Complicating Pregnancy (HDCP), with an incidence of 5.2 %-8.2 %, majorly results in maternal perinatal death [1]. HDCP seriously endangers the maternal and infant safety, leading to risk elevation of adverse pregnancy outcomes. However, its mechanism is unclear [2,3]. MicroRNA-193b-5p (miR-193b-5p) is one of the small non-coding singlestranded RNA members, which is involved in various pathophysiological processes such as the regulation of inflammatory response, cell differentiation and proliferation, cancer cell proliferation and migration, etc., [4,5]. It has been revealed that high-level miR-193b- 5p is associated with the pathogenesis of HDCP [6,7]. Human Neuregulin-1 (NRG-1) belongs to Epidermal Growth Factors (EGFs). NRG-1 exerts a vital role in vascular pathophysiology. NRG expresses in vascular endothelial cells and Vascular Smooth Muscle Cells (VSMCs) and also remarkably suppresses VSMC proliferation and migration in vitro [8]. Previously, NRG-1 participated in the pathogenesis of HDCP [9]. Herein, serum miR-193b-5p and NRG-1 levels in 120 HDCP patients were monitored and their relationship with the clinical parameters of HDCP patients and their diagnostic value for HDCP were analyzed.
Materials and Methods
General data:
A total of 120 HDCP patients (observation group) admitted to our hospital from January 2020 to December 2021 were selected.
Inclusion criteria: Meet the diagnostic criteria of HDCP in the 8th edition of the “Obstetrics and Gynecology” [10]; primiparas with a gestational period of more than 20 w and singleton gestation and no effective treatment before admission.
Exclusion criteria: Primary renal impairment; primary hypertension; complicated with acute and chronic infections, including hepatitis, tuberculosis, pneumonia, etc.; complicated with chronic diseases such as coronary heart disease, diabetes, etc., The patients aged 21-38 y old, average (32.26±2.17) y; the delivery gestational age was 34-39 w, average (36.57±1.56) w; the Body Mass Index (BMI) at the time of enrollment was 22- 29 kg/m2, average (26.89±1.37) kg/m2; gravidity was 0-5 times, average (2.21±0.16) times and parity was 0-3 times, average (2.12±0.33) times.
According to HDCP classification criteria, the observation group was divided into three subgroups: In the Hypertensive Disorders in Pregnancy (HDP) group (42 cases), urine protein was negative, hypertension occurred for the first time during pregnancy and blood pressure returned to normal within 3 mo postpartum. In the mild preeclampsia group (43 cases), urinary protein was ≥0.3 g/24 h, diastolic blood pressure ≥90 mmHg and/or systolic blood pressure ≥140 mmHg 20 w post-pregnancy and symptoms such as abdominal discomfort, blurred vision, headache, etc., may be present. In the severe preeclampsia group (35 cases), preeclampsia patients had one of the following adverse conditions: Urinary protein ≥2 g/24 h; diastolic blood pressure ≥110 mmHg and/or systolic blood pressure ≥160 mmHg; platelet <100×10°/l; liver and kidney function damage and persistent headache, epigastric pain or neurovisual dysfunction. At the same time, 120 healthy pregnant women who received regular perinatal care in the Obstetrics Department of our hospital during the same period were randomly selected as the control group. All of them were singleton pregnancy, full-term delivery and pregnancy complications were excluded by systematic obstetric examination. They aged 20- 39 y old, average (36.21±2.09) y; delivery gestational age was 36-40 w, average (37.42±1.26) w; the BMI at the time of enrollment was 22-28 kg/m2, average (26.01±1.09) kg/m2; gravidity was 0-5 times, average (2.11±0.24) times; parity was 0-3 times, average (2.27±0.24) times. In addition, 120 non-pregnant healthy women who underwent physical examination in our hospital during the same period were selected as the health control group, aged 21-40 y old, average (37.33±2.53) y; the BMI at the time of enrollment was 21-28 kg/m2, average (25.85±1.25) kg/m2. Age, gravidity, delivery gestational weeks and parity in observation group exhibited no significance relative to control group (p>0.05) and age and BMI among the three groups presented no difference (p>0.05). This study was approved by the ethics committee of the hospital and all subjects signed the informed consent.
Methods:
Detection of serum miR-193b-5p: The 5 ml of cubital venous blood was drawn from the subjects after admission, left standing at room temperature for 20 min and centrifuged at 3000 r/min for 10 min. The centrifugation radius was 15 cm and 3 ml of supernatant was collected and placed in a refrigerator at -80° for testing. Total RNA was extracted from cells by a TaqMan miRNA kit and serum miR-193b-5p level was detected by real-time fluorescence quantitative Polymerase Chain Reaction (PCR). Primers were designed according to the messenger RNA (mRNA) sequence of the target gene and the reverse transcription product was designed with the software Primer express 3.0. miR-193b-5p primers, forward: 5’-AGGAG GCAGCGCTCTC-3’; reverse: 5’-CTGCCCCAGTGCTGCT- 3’. After reverse transcription, the reverse transcription product was used as a template and the amplification was performed on a real-time quantitative PCR instrument. Reaction conditions: 85° for 3 min, 85° for 20 s and 42° for 40 s, a total of 35 cycles. The 2-ΔΔct method represented miR-193b-5p expression level and the average was taken from three times of experiments.
Detection of serum NRG-1 level: The 5 ml of fasting cubital venous blood was collected from subjects at the time of enrollment and the centrifugation method was the same as above. Serum NRG-1 level was detected by Enzyme-Linked Immunosorbent Assay (ELISA) with the HED-SY96S automatic microplate reader and the kit was purchased from Wuhan Service Bio Technology Co., Ltd.
Prognosis: Maternal and infant outcomes were tracked for all patients and the occurrence of adverse pregnancy outcomes such as eclampsia, postpartum hemorrhage, maternal death, intrauterine growth restriction, neonatal asphyxia, neonatal death, etc., were counted. Those with adverse pregnancy outcomes were unfavorable prognosis, with a total of 42 cases and those without adverse pregnancy outcomes were good prognosis, with a total of 78 cases.
Statistical analysis:
Statistical Package for the Social Sciences (SPSS) 20.0 statistical software was used for data analysis. Measurement data that conformed to the normal distribution were expressed as x±s. Comparisons among multiple groups were performed by variance analysis and pair wise comparisons between groups were performed using Least Significant Difference (LSD)-t test. Count data were expressed as the “n” or percent (%) and the comparison between groups was performed using the Chi-square (χ2) test. Pearson correlation was used for correlation analysis; logistic regression was used for risk factor analysis; Receiver Operating Characteristic (ROC) curve was used for predictive performance evaluation. p<0.05 was considered to be statistically significant.
Results and Discussion
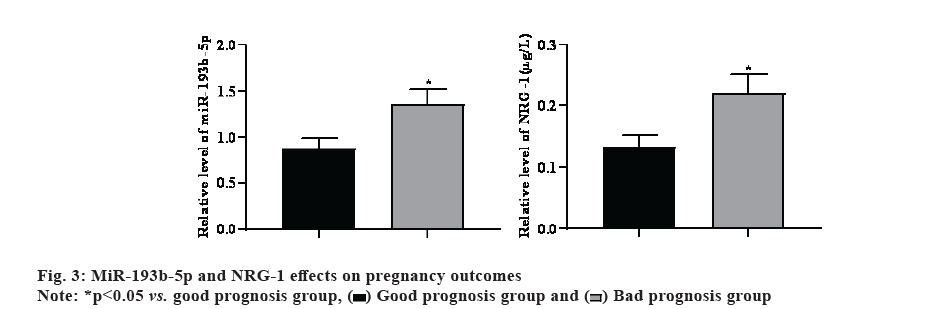
Serum miR-193b-5p and NRG-1 levels in observation group presented up-regulation relative to control group and health control group (p<0.05), while those in control group exhibited up-regulation relative to health control group (p<0.05) as shown in fig. 1.
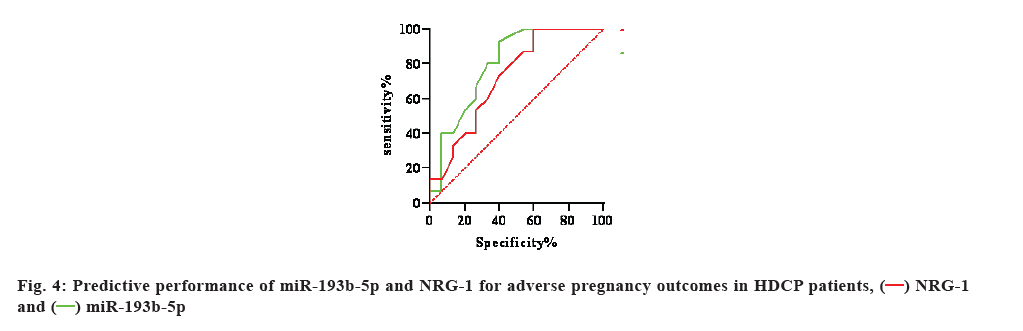
Serum miR-193b-5p and NRG-1 levels in severe preeclampsia group presented up-regulation relative to mild preeclampsia group and HDP group (p<0.05) and those in mild preeclampsia group exhibited upregulation relative to HDP group (p<0.05) as shown in fig. 2.
Serum miR-193b-5p level in HDCP patients with different ages, BMI at the time of enrollment and prognosis presented differential significance (p<0.05) and serum miR-193b-5p level in HDCP patients with different delivery gestational weeks, gravidity and parity presented no significance (p>0.05). Serum NRG-1 level in HDCP patients with different delivery gestational weeks and prognosis presented differential significance (p<0.05) and serum NRG-1 level in HDCP patients of different ages, BMI at the time of enrollment, gravidity and parity presented no significance (p>0.05), as shown in Table 1.
| Clinical parameters | n | MiR-193b-5p | t | p | NRG-1 | t | p |
|---|---|---|---|---|---|---|---|
| Age | 3.466 | 0.002 | 0.462 | 0.712 | |||
| >33 y old | 64 | 1.32±0.21 | 0.15 ±0.05 | ||||
| <33 y old | 56 | 1.08±0.24 | 0.17 ±0.04 | ||||
| BMI | 2.763 | 0.006 | 0.502 | 0.736 | |||
| >25 kg/m2 | 71 | 1.35±0.31 | 0.15 ±0.04 | ||||
| <25 kg/m2 | 49 | 1.07±0.18 | 0.16 ±0.04 | ||||
| Delivery Gestational w | 0.538 | 0.729 | 6.053 | 0 | |||
| >36 w | 76 | 1.23±0.14 | 0.05 ±0.02 | ||||
| <36 w | 44 | 1.26±0.19 | 0.14±0.03 | ||||
| Gravidity | 0.735 | 0.538 | 0.451 | 0.767 | |||
| >3 times | 49 | 1.25±0.16 | 0.15 ±0.04 | ||||
| <3 times | 71 | 1.22±0.19 | 0.16 ±0.03 | ||||
| Parity | 0.275 | 0.889 | 0.471 | 0.809 | |||
| >3 times | 44 | 1.18±0.29 | 0.14 ±0.03 | ||||
| <3 times | 76 | 1.20±0.26 | 0.16 ±0.05 | ||||
| Prognosis | 9.108 | 0 | 5.367 | 0 | |||
| Good | 78 | 0.91±0.25 | 0.07±0.02 | ||||
| Bad | 42 | 1.42±0.36 | 0.14±0.05 |
Table 1: Clinical Parameters of HDCP Patients
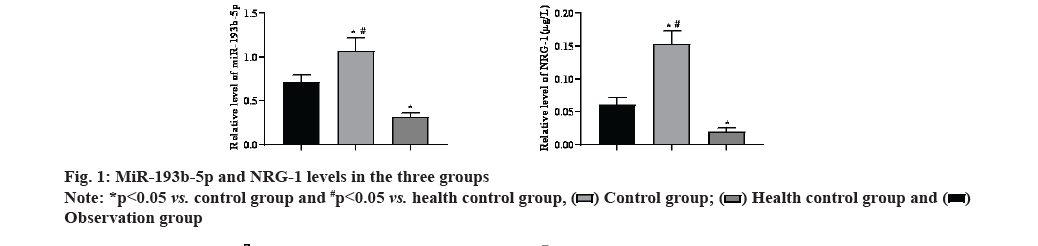
Serum miR-193b-5p and NRG-1 levels in bad prognosis group presented up-regulation relative to good prognosis group (p<0.05) as shown in fig. 3.
ROC curve analysis showed that serum miR-193b- 5p and NRG-1 had good predictive performance for adverse pregnancy outcomes in HDCP patients and their Area Under the Curve (AUC) for the diagnosis of HDCP was 0.798 (95 % Confidence Interval (CI): 0.634-0.962) and 0.720 (95 % CI: 0.534-0.905), respectively. The miR-193b-5p and NRG-1 values corresponding to the maximum value of Youden index were the cut-off points of HDCP, which were 1.15 and 0.117 μg/l, respectively. The sensitivity and specificity of diagnosing HDCP at this cut-off value were 73.33 % and 72.81 % as well as 74.26 % and 71.55 %, respectively as shown in Table 2 and fig. 4.
| Indicator | Sensitivity (%) | Specificity (%) | Yoden index | Positive predictive value (%) | Negative predictive value (%) | Diagnostic coincidence rate (%) |
|---|---|---|---|---|---|---|
| MiR-193b-5p | 72.93 | 72 | 0.4493 | 82.5 | 59.02 | 72.6 |
| NRG-1 | 74.59 | 75 | 0.4959 | 84.38 | 61.48 | 74.47 |
Table 2: Predictive Performance of MiR-193b-5p AND NRG-1 for Adverse Pregnancy Outcomes in HDCP Patients
As a common complication of pregnancy, HDCP has a high incidence. Clinically, the disease is mainly affected by pregnant women post-pregnancy (20 w) and manifested with edema, hypertension, proteinuria, convulsions, coma, etc. Pregnant women are in a hypercoagulable state due to increased coagulation factor activity, which facilitates placental abruption during labor, but can also cause postpartum hemorrhage [11]. It has been revealed that untreated disease can lead to placental abruption, maternal shock and even death [12].
The expression profile of miRNAs changes significantly during pregnancy, which is possibly involved in the physiological process of pregnancy. In HDCP patients, miRNAs also have corresponding changes. The results of this study demonstrated that serum miR-193b-5p level in HDCP patients presented up-regulation relative to control group and health control group and serum miR- 193b-5p level in control group presented up-regulation relative to health control group, indicating that miR- 193b-5p involves in HDCP onset and progression. Herein, miR-193b-5p level in HDCP patients increased with the severity of the disease, indicating that serum miR-193b-5p level can reflect the severity of HDCP. MiR-193b-5p presents elevation in a variety of tumors, mainly promoting cancer progression. For example, miR-193b-5p exhibits elevation in non-small cell lung cancer and breast cancer, and miR-193b-5p downregulation has a inhibitory effect on prostate cancer [13,14]. MiR-193b-5p presents up-regulation in colorectal cancer, and miR-193b-5p inhibition can significantly reduce proliferation of cancer cells [15]. At present, there are few reports on whether the changes of miR-193b- 5p expression are related to HDCP. Herein, when miR- 193b-5p was >1.15, it had high diagnostic performance in predicting poor pregnancy outcomes of HDCP patients (sensitivity: 73.33 %, specificity: 72.81 %, AUC: 0.798), indicating that miR-193b-5p is involved in the pathophysiological process of HDCP and has a high predictive value for poor pregnancy outcomes of HDCP patients.
NRG-1 is an Endocrine Gland-derived Vascular Endothelial Growth Factor (EG-VEGF)-related protein that exerts multiple regulatory roles in the heart through an erythroid viral oncogene homolog. NRG-1 is synthesized and released by endocardial and myocardial microvascular endothelial cells in response to mechanical stretch, hypoxia and signaling peptides, and is involved in paracrine intercellular communication in ventricular tissue [16]. NRG-1 plays an important role in vascular physiology and pathology [17]; NRG-1 distributes in vascular endothelial cells and VSMCs, whose receptors locates to potential VSMCs [18]; NRG-1 treatment can significantly reduce proliferation and migration of VSMCs stimulated by platelet derived growth factor in vitro [7]. EG-VEGF is a key factor in promoting the invasion of placental trophoblasts. EG-VEGF binds to primary cilia to initiate a signal cascade and promote placental development. NRG-1 elevation can suppress EG-VEGF expression and blocks downstream extracellular signal-regulated kinase signaling, resulting in insufficient trophoblast engraftment. In this study, NRG-1 level significantly increased in patients with severe preeclampsia and poor prognosis, indicating that NRG-1 elevation was related to the condition and prognosis of HDCP patients, high-levels NRG-1 predicted HDCP exacerbation and poor prognosis. Advanced age and obesity are highrisk factors for HDCP [19,20], and NRG-1 may play an interaction mechanism with HDCP high-risk factors in the pathogenesis of HDCP, which promotes the onset and progression of HDCP. Herein, when NRG-1 was >2.86, it had high diagnostic performance in predicting renal function damage in HDCP patients (sensitivity: 74.26 %, specificity: 71.55 %, AUC: 0.720), indicating that NRG-1 is involved in the pathophysiological process of HDCP has a high predictive value for poor pregnancy outcomes of HDCP patients.
In conclusion, serum miR-193b-5p and NRG-1 play a synergistic mechanism in the onset and progression of HDCP and present association with onset progression and prognosis of HDCP, which can be used as valuable biomarkers for the diagnosis of HDCP.
Acknowledgments:
The work was supported by Taizhou People’s Hospital.
Conflict of interests:
The authors declared no conflicts of interest.
References
- Gyselaers W. Maternal venous hemodynamic dysfunction in proteinuric gestational hypertension: Evidence and implications. J Clin Med 2019;8(3):335.
[Crossref] [Google Scholar] [PubMed]
- Lumbers ER, Pringle KG. Roles of the circulating renin-angiotensin-aldosterone system in human pregnancy. Am J Physiol Regul Integr Comp Physiol 2014;306(2):R91-101.
[Crossref] [Google Scholar] [PubMed]
- Irani RA, Xia Y. The functional role of the renin–angiotensin system in pregnancy and preeclampsia. Placenta 2008;29(9):763-71.
[Crossref] [Google Scholar] [PubMed]
- Lasda E, Parker R. Circular RNAs: Diversity of form and function. RNA 2014;20(12):1829-42.
[Crossref] [Google Scholar] [PubMed]
- Khordadmehr M, Shahbazi R, Sadreddini S, Baradaran B. MiR‐193: A new weapon against cancer. J Cell Physiol 2019;234(10):16861-72.
[Crossref] [Google Scholar] [PubMed]
- Lv Y, Lu C, Ji X, Miao Z, Long W, Ding H, et al. Roles of microRNAs in preeclampsia. J Cell Physiol 2019;234(2):1052-61.
[Crossref] [Google Scholar] [PubMed]
- Schuster J, Cheng SB, Padbury J, Sharma S. Placental extracellular vesicles and pre‐eclampsia. Am J Reprod Immunol 2021;85(2):e13297.
[Crossref] [Google Scholar] [PubMed]
- Clement CM, Thomas LK, Mou Y, Croslan DR, Gibbons GH, Ford BD. Neuregulin-1 attenuates neointimal formation following vascular injury and inhibits the proliferation of vascular smooth muscle cells. J Vasc Res 2007;44(4):303-12.
[Crossref] [Google Scholar] [PubMed]
- Wu N, Jin L, Cai J. Profiling and bioinformatics analyses reveal differential circular RNA expression in hypertensive patients. Clin Exp Hypertens 2017;39(5):454-9.
[Crossref] [Google Scholar] [PubMed]
- Wang CY, Tsai PY, Chen TY, Tsai HL, Kuo PL, Su MT. Elevated miR‐200a and miR‐141 inhibit endocrine gland‐derived vascular endothelial growth factor expression and ciliogenesis in preeclampsia. J Physiol 2019;597(12):3069-83.
[Crossref] [Google Scholar] [PubMed]
- Jung YJ, Cho HY, Cho S, Kim YH, Jeon JD, Kim YJ, et al. The level of serum and urinary nephrin in normal pregnancy and pregnancy with subsequent preeclampsia. Yonsei Med J 2017;58(2):401-6.
[Crossref] [Google Scholar] [PubMed]
- Ziyadeh FN, Wolf G. Pathogenesis of the podocytopathy and proteinuria in diabetic glomerulopathy. Curr Diabetes Rev 2008;4(1):39-45.
[Crossref] [Google Scholar] [PubMed]
- Grossi I, Salvi A, Abeni E, Marchina E, de Petro G. Biological function of MicroRNA193a-3p in health and disease. Int J Genomics 2017;2017.
[Crossref] [Google Scholar] [PubMed]
- Tsai KW, Leung CM, Lo YH, Chen TW, Chan WC, Yu SY, et al. Arm selection preference of microRNA-193a varies in breast cancer. Sci Rep 2016;6(1):1-3.
[Crossref] [Google Scholar] [PubMed]
- Chou NH, Lo YH, Wang KC, Kang CH, Tsai CY, Tsai KW. MiR-193a-5p and-3p play a distinct role in gastric cancer: MiR-193a-3p suppresses gastric cancer cell growth by targeting ETS1 and CCND1. Anticancer Res 2018;38(6):3309-18.
[Crossref] [Google Scholar] [PubMed]
- Vermeulen Z, Hervent AS, Dugaucquier L, Vandekerckhove L, Rombouts M, Beyens M, et al. Inhibitory actions of the NRG-1/ErbB4 pathway in macrophages during tissue fibrosis in the heart, skin and lung. Am J Physiol Heart Circ Physiol 2017;313(5):H934-45.
[Crossref] [Google Scholar] [PubMed]
- Odiete O, Hill MF, Sawyer DB. Neuregulin in cardiovascular development and disease. Circ Res 2012;111(10):1376-85.
[Crossref] [Google Scholar] [PubMed]
- Parodi EM, Kuhn B. Signalling between microvascular endothelium and cardiomyocytes through neuregulin. Cardiovasc Res 2014;102(2):194-204.
[Crossref] [Google Scholar] [PubMed]
- Dhawan D, Sharma S. Abdominal obesity, adipokines and non-communicable diseases. J Steroid Biochem Mol Biol 2020;203:105737.
- Ziętek M, Celewicz Z, Szczuko M. Short-chain fatty acids, maternal microbiota and metabolism in pregnancy. Nutrients 2021;13(4):1244.
[Crossref] [Google Scholar] [PubMed]
 Observation group
Observation group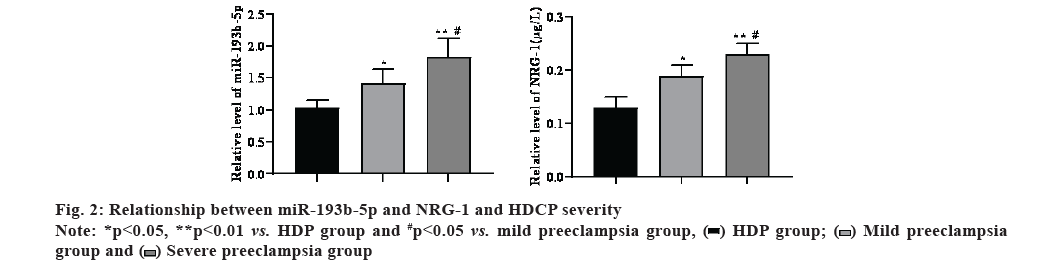
 group and
group and  Severe preeclampsia group
Severe preeclampsia group