- *Corresponding Author:
- Xiaoliu Shao
Quality Control Office, The Fourth Hospital of Shijiazhuang, Shijiazhuang, Hebei Province 050000, China
E-mail: shishouyan02199@163.com
| This article was originally published in a special issue, “Transformative Discoveries in Biomedical and Pharmaceutical Research” |
| Indian J Pharm Sci 2023:85(4) Spl Issue “232-238” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
To investigate the correlation between dilated fetal bowel detected by prenatal ultrasonography and fetal prognosis. In this retrospective study, a total of 157 pregnant women who underwent Doppler ultrasound obstetric examination in our hospital from August 2020 to August 2021 were included. All pregnant women were divided into the normal group and the dilation group according to the results of ultrasound diagnosis. The normal group was the pregnant women with normal fetal bowel diameter diagnosed by prenatal ultrasound. The dilation group was the pregnant women diagnosed with fetal bowel dilatation by prenatal ultrasound. Pregnant women in the dilation group were followed up until 1 mo after the delivery of the fetus. The dilation sites of all fetuses in the dilation group, pregnancy outcomes and neonatal Apgar scores were collected, and the correlation between fetal bowel dilatation and neonatal Apgar scores was analyzed. There was no significant difference in the above indices (p>0.05). The average inner diameter of the fetuses with duodenal canal dilatation, jejunal and ileal canal dilatation, and colonic canal dilation were negatively correlated with the neonatal Apgar score (r=-0.751, r=-0.723, r=-0.682, p<0.05). The incidence of premature birth, induced labor and polyhydramnios in fetuses with duodenal canal dilatation was significantly higher than that in fetuses with jejunal and colonic canal dilatation (p<0.05). Prenatal ultrasound diagnosis of dilated fetal bowel is correlated with fetal prognosis and has a predictive potential. Fetal duodenal dilatation or other abnormalities have a worse prognosis than small bowel or colonic dilatation alone, which is conducive to identify fetal status and implementation of preventive strategies.
Keywords
Prenatal ultrasound, fetus, bowel dilatation, ultrasound, hyperplasia
Dilated fetal bowel is characterized by fluid-filled bowel loops that are at least 15 mm in length or at least 7 mm in diameter and the identification of its cause remains a challenging issue. Dilated fetal bowel is attributable to congenital intestinal malformations or fetal fecal obstruction, and transient fetal bowel obstruction can present as dilated fetal bowel on ultrasound images, which can be spontaneously cured[1,2].
Currently, advances in prenatal ultrasound have led to high accuracy in detecting diseases of the unborn fetus. Although it is unavailable to examine the gastrointestinal tract in detail, ultrasound examination can be used to determine the presence or absence of strong intestinal echoes or bowel dilatation[3,4]. Nevertheless, bowel dilatation does not amount to an absolute intestinal malformation, so it cannot be served as an indication for induction of labor. Ultrasound images of fetal bowel distention are a sign of mechanical or functional bowel obstruction[5] and the prevalence is associated with the underlying disease, i.e., bowel atresia or stricture, volvulus, meconium ileus, pancolitis nerves nodular hyperplasia and meconium embolism syndrome. It is a demanding task to identify the difference between dilated small bowel loops and colon using ultrasound imaging, as well as the number and location of obstructions[6,7]. Thus, dilated fetal bowel may be associated with different postpartum outcomes, resulting in problematic prenatal management and parental counseling.
The robustness of these prenatal ultrasonography findings remains poorly understood. Some scholars believe that intestinal hyperechoic may be a normal finding and the value of intestinal dilation to predict postpartum outcomes is questionable[8]. Worse yet is, numerous studies have been conducted on the frequency of postpartum abnormalities in children with bowel abnormalities using prenatal ultrasonography. In view of the fore-mentioned knowledge, the present study was undertaken to analyze the correlation between dilated fetal bowel detected by prenatal ultrasound and fetal prognosis.
Materials and Methods
General information:
A total of 157 pregnant women who underwent Doppler ultrasound obstetric examination in our hospital from August 2020 to August 2021 were included in this retrospective study and all the pregnant women were singleton pregnancies. All pregnant women were divided into the normal group and the dilation group according to the results of ultrasound diagnosis. The normal group was the pregnant women with normal fetal bowel diameter diagnosed by prenatal ultrasound and 109 cases were included. The dilation group was the pregnant women diagnosed with fetal bowel dilatation by prenatal ultrasound, and 48 cases were included. This study complies with the Declaration of Helsinki and was approved by the Ethics Committee of our hospital and all subjects have signed the consent form.
Inclusion and exclusion criteria:
Participants were eligible if singleton pregnancy with natural conception; diagnosed as dilated fetal bowel by prenatal ultrasound[9]; had no other known diseases. Participants were excluded if they lost to follow-up.
Methods:
All included pregnant women received prenatal ultrasound screening, using Voluson™ E8 ultrasound (US, GE) color Doppler ultrasound diagnostic instrument, two-dimensional convex array probe frequency of 3.5-5.0 MHz and the ultrasound parameters were modified according to the conditions of pregnant women. The content of ultrasonography includes measuring fetal growth diameter and structure, location, inner diameter and extent of fetal intestinal dilatation. Using the first-stage fetal ultrasound procedure, the pregnant woman was placed in the supine position and the ultrasound probe was scanned over the abdomen. Pregnant women were followed up during pregnancy, the patients and their families were consulted about the possible diagnosis and treatment of postpartum fetuses and their pregnancy outcomes were counted.
Outcome measures:
Assessment criteria: According to the study of Nyberg et al., when the inner diameter of the small intestine exceeds 7 mm, the length exceeds 15 mm and the inner diameter of the colon exceeds 18 mm in the third trimester, it is defined as dilated fetal bowel. Baseline profiles such as age and Body Mass Index (BMI) of all eligible participants were analyzed.
Adverse outcomes: It includes preterm birth (delivery at <37 w of gestation), induction of labor (including delayed pregnancy, severe maternal disease, premature rupture of membranes without labor, etc.), stillbirth (no fetal heartbeat and no fetal limb movement on ultrasonography), craniocerebral deformation and atrophy, etc.), polyhydramnios (the vertical depth of the largest dark area of amniotic fluid >8 cm).
Fetal prognosis: Fetal prognosis was assessed by Apgar score, which included muscle tone, pulse, and response to stimulation, skin color and respiration. The full score ranges from to 10 points, with 8-10 points indicating no asphyxia that requires no special treatment, 4-7 points indicating mild asphyxia (if the amniotic fluid is contaminated with meconium, tracheal intubation is still required to remove secretions and meconium in the airway and ensure airway), ≤3 points indicating severe asphyxia that requires immediate resuscitation.
Statistical analysis:
GraphPad Prism 8 was used for graphics rendering; Statistical Package for the Social Sciences (SPSS) 26.0 software was used for data analysis. Measurement data were expressed as (x±s), and t-test was used to compare whether there was a statistical difference. Count data were analyzed using Chi-square (χ²) test. The correlation analysis between measurement data was performed by Pearson correlation analysis. All tests were 2-sided, with a significance level of p<0.05.
Results and Discussion
The dilation group included 48 pregnant women, aged 23-38 y, with an average age of (29.15±3.28) y, the diagnosis gestational age was 20-28 w, the average gestational age was (23.15±4.17) w, the BMI was (21.38±0.84) kg/m², the number of pregnancy were 39 cases of first birth, 9 cases of non-first birth; mode of delivery has 20 cases of normal delivery, 4 cases of operative vaginal delivery, 4 cases of elective cesarean section, 20 cases of emergency cesarean section, 22 cases of duodenal bowel dilation, 22 cases of duodenal bowel dilation, 15 cases of jejunal bowel dilation and 11 cases of colon bowel dilation. The normal group included 109 pregnant women, aged 23-37 y, with an average age of (29.58 ±3.47) y, BMI (21.41±0.79) kg/m², number of pregnancies were 91 cases of first birth, 18 cases of non-first birth; mode of delivery has 53 normal deliveries, 7 operative vaginal deliveries, 41 elective cesarean deliveries and 8 emergency cesarean deliveries. The baseline data between the two groups of pregnant women were generally balanced (all p>0.05) as shown in Table 1.
| Dilation group (n=48) | Normal group (n=109) | t | p | ||
|---|---|---|---|---|---|
| Age (year) | Range | 23-38 | 23-37 | - | - |
| mean | 29.15±3.28 | 29.58±3.47 | 0.727 | 0.468 | |
| Gestational age (weeks) | Range | 20-28 | - | - | - |
| Mean | 23.15±4.17 | - | - | - | |
| BMI (kg/m²) | 21.38±0.84 | 21.41±0.79 | 0.215 | 0.83 | |
| Number of pregnancies (times) | First birth | 39 (81.25) | 91 (83.49) | 0.117 | 0.723 |
| Non-first birth | 9 (18.78) | 18 (16.51) | - | - | |
| Mode of delivery | Normal delivery | 20 (41.67) | 53 (48.62) | - | - |
| Surgical vaginal delivery | 4 (8.33) | 7 (6.42) | - | - | |
| Elective cesarean section | 4 (8.33) | 41 (37.61) | - | - | |
| Emergency cesarean section | 20 (41.67) | 8 (7.34) | - | - | |
| Dilated site | Duodenal bowel | 22 (48.83) | - | - | - |
| Jejunal intestinal tube | 15 (31.25) | - | - | - | |
| Colon bowel | 11 (22.92) | - | - | - | |
Table 1: Baseline data of two groups of pregnant women.
The average inner diameter of the fetus with duodenal bowel dilation was 15.84±2.88 mm, and the neonatal Apgar score was 4.68±1.44 points; the average inner diameter of the jejunoileum dilated fetus was 15.35±3.94 mm, the neonatal Apgar score was 5.01±2.25 points; the average inner diameter of the fetus with colonic dilation was 14.01±4.53 mm and the neonatal Apgar score was 5.65±2.45 points; there was no significant difference in the above indices (p>0.05) as shown in Table 2.
| n | Average inner diameter (mm) | Apgar score | |
|---|---|---|---|
| Duodenal bowel | 22 | 15.84±2.88 | 4.68±1.44 |
| Jejunal intestinal tube | 15 | 15.35±3.94 | 5.01±2.25 |
| Colon bowel | 11 | 14.01±4.53 | 5.65±2.45 |
| t | 0.932 | 0.89 | |
| p | 0.401 | 0.418 |
Table 2: Inner diameter and neonatal apgar score of fetuses with dilated bowel at different sites.
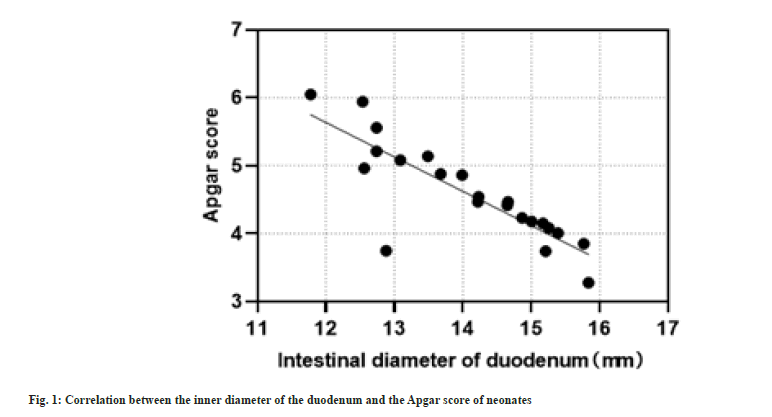
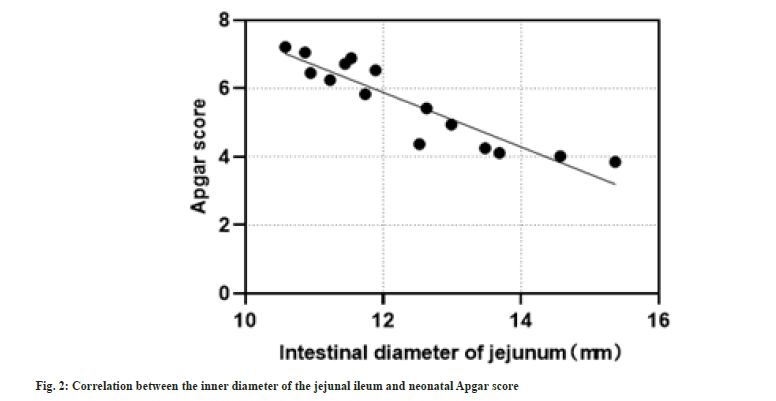
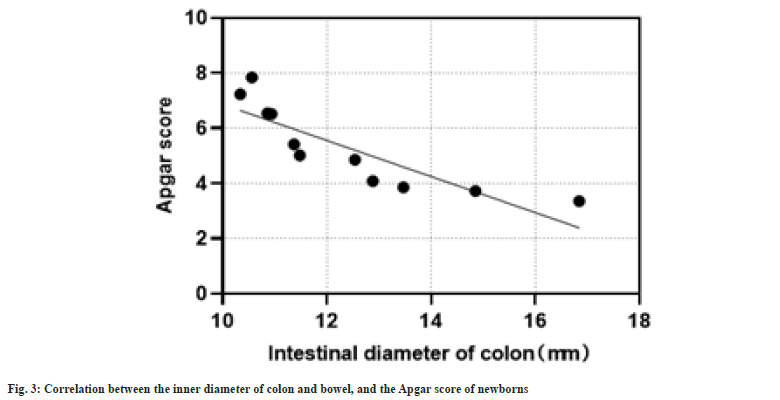
The average inner diameter of the fetuses with duodenal canal dilatation, jejunal and ileal canal dilatation and colonic canal dilation were negatively correlated with the neonatal Apgar score (r=-0.751, r=-0.723, r=-0.682, p<0.05) as shown in fig. 1-fig. 3.
There were 9 cases of premature birth, 8 cases of induced labor, 1 case of stillbirth, 14 cases of polyhydramnios, 1 case of premature birth, 3 cases of induced labor, 0 cases of stillbirth and 5 cases of polyhydramnios at the site of duodenal canal dilation. There were 1 case of preterm birth, 0 cases of induced labor, 1 case of stillbirth and 2 cases of polyhydramnios at the site of colonic dilatation and the differences were statistically significant. Among them, the incidence of premature birth, induced labor and polyhydramnios in fetuses with duodenal canal dilatation was significantly higher than that in fetuses with jejunal and colonic canal dilatation (p<0.05) as shown in Table 3.
| n | Premature birth | Induced labor | Stillbirth | Polyhydramnios | |
|---|---|---|---|---|---|
| Duodenal bowel | 22 | 9 (40.91) | 8 (36.36) | 1 (4.55) | 14 (63.64) |
| Jejunal intestinal tube | 15 | 1 (6.67) | 3 (20.00) | 0 (0.00) | 5 (33.33) |
| Colon bowel | 11 | 1 (9.09) | 0 (0.00) | 1 (9.09) | 2 (18.18) |
| χ² | - | 7.123 | 6.234 | 5.003 | 8.845 |
| p | - | 0.019 | 0.028 | 0.085 | 0.009 |
Table 3: Prognosis of fetuses with dilated bowel at different sites.
Dilated fetal bowel usually indicates the possibility of fetal bowel obstruction and fetal bowel obstruction may be present anywhere in the bowel. Its pathogenesis is not clear, with some intestinal obstruction being related to a single intrauterine intestinal obstruction, which spontaneously disappears without adverse consequences and some being related to factors such as congenital intestinal dysplasia or infection, which can lead to adverse pregnancy outcomes[10]. As recently evidenced, the pathophysiological pathway leading to intestinal distention in obstructive cases might be explained by the difficulty of passing intestinal contents through the intestine, followed by fluid accumulation and lumen dilation in the intestine[11].
In the event of obstruction due to occlusion of the lumen, both the intra-intestinal and extra-abdominal parts can be expected to distend. Instead, only the protruding portion of the extra-abdominal bowel may be dilated due to kinks at the level of the abdominal wall defect. Additionally, bowel protrusions may not function properly and dilation may represent stagnation of contents associated with insufficient peristalsis[12]. Overwhelming evidence confirmed that when fetal intestinal obstruction is accompanied by duodenal obstruction, the ultrasound image is a typical "double-bubble sign", which is easier to diagnose, and the accuracy approaches 100 %[13]. However, there is no single accurate diagnostic standard for small bowel and colonic obstruction, so the accuracy of predicting adverse fetal outcomes is low and the clinical application value is low. The variability of ultrasound equipment and techniques may be attributable the difficulty in obtaining an accurate diagnosis[14]. Prior reports have involved retrospective studies of prenatal ultrasonography of children with known surgical findings such as intestinal atresia or meconium peritonitis. Armed with the knowledge, this study attempted to elucidate the correlation between fetal bowel dilatation detected by prenatal ultrasonography and fetal prognosis.
Our findings are similar to those of Borsellino et al., who examined the accuracy of prenatal ultrasonography in determining the presence of any chest or abdominal abnormalities, and the results of this study suggest that the diagnosis of fetal bowel dilatation by prenatal ultrasonography is associated with fetal prognosis, and duodenal canal dilation, jejunal ileal canal dilatation, and colonic canal dilation were negatively correlated with neonatal Apgar scores. Previous studies have attempted to investigate a number of factors that are used to identify poor-prognosis fetal cases, among which prenatal ultrasonography diagnoses fetal bowel dilatation. Although no studies have verified the correlation between this and fetal prognosis, multiple potential factors have been reported[15,16].
To our best understanding, there is plenty of evidence supporting the relationship between prenatal ultrasound diagnosis of fetal bowel dilatation and fetal prognosis. The findings of the present study showed that bowel diameter was negatively correlated with Apgar score and all correlation coefficients were greater than 0.6 and Nazhang et al. also demonstrated that increased fetal gut diameter was associated with neonatal prognosis, which is consistent with the findings of the present study, further confirming the association of gut dilation with fetal prognostic value.
Additionally, the results of this study also showed that the incidence of preterm birth, induction of labor and polyhydramnios in fetuses with dilated duodenal canal was significantly higher than that in fetuses with dilated jejunal and colonic canals. It is suggested that the enlarged diameter of the fetal bowel is related to polyhydramnios, premature birth, induced labor and chromosomal abnormalities. Typical pregnant women with fetal atresia are accompanied by polyhydramnios. The amount of amniotic fluid reflects the severity of fetal duodenal obstruction and whether it is accompanied by intestinal obstruction that affects the absorption of amniotic fluid. Intestinal malformations of the fetus lead to obstruction of amniotic fluid swallowing, so such fetuses are prone to polyhydramnios[17,18]. It also suggests that according to the position of fetal intestinal dilation, the occurrence of adverse pregnancy outcomes in pregnant women can be targeted, which is collaborated by previous studies that fetuses with bowel dilatation detected prenatally possess a greater odd of poor prognosis than normal fetuses[19-21].
There are still several limitations in this study. First, the definition of "dilation" is inconsistent to the standard of other articles. Second, the fetal prognosis in this study is not sufficiently broad, the sensitivity and specificity of ultrasound in fetal intestinal dilatation are not elaborated more specifically and the diagnostic evaluation might have limited potential in the management or care of the mother or the fetus. Third, this study includes a small sample size; it is required to include a larger sample size in the subsequent studies to further validate the findings in the present study.
In conclusion, prenatal ultrasound diagnosis of dilated fetal bowel is correlated with fetal prognosis, and has predictive potentials. Fetal duodenal dilatation or other abnormalities have a worse prognosis than small bowel or colonic dilatation alone, which is conducive to identify fetal status and implementation of preventive strategies.
Funding:
Hebei Provincial Health and Health Commission Medical Science Research Project Project No.: 20191440.
Author’s contributions:
Jianqiang Su and Na Li have contributed equally to this work.
Conflict of interests:
The authors declared no conflict of interests.
References
- Husu S, Nelson N, Selbing A. Prenatal bowel dilatation: Congenital chloride diarrhoea. Arch Dis Child Fetal Neonatal Ed 2001;85(1):F65.
- Sipes SL, Weiner CP, Williamson RA, Pringle KC, Kimura K. Fetal gastroschisis complicated by bowel dilation: An indication for imminent delivery? Fetal Diagn Ther 1990;5(2):100-3.
[Crossref] [Google Scholar] [PubMed]
- Goruppi I, Arévalo S, Gander R, Molino JA, Oria M, Carreras E, et al. Role of intraluminal bowel echogenicity on prenatal ultrasounds to determine the anatomical level of intestinal atresia. J Matern Fetal Neonatal Med 2017;30(1):103-8.
[Crossref] [Google Scholar] [PubMed]
- Ronin C, Mace P, Stenard F, Loundou A, Capelle M, Mortier I, et al. Antenatal prognostic factor of fetal echogenic bowel. Eur J Obstet Gynecol Reprod Biol 2017;212:166-70.
[Crossref] [Google Scholar] [PubMed]
- Achiron R, Seidman DS, Zalel Y, Orvieto R, Sivan E, Lipitz S. Nonobstructive dilatation of the fetal bowel in twin gestations. Fetal Diagn Ther 2003;18(2):128-31.
[Crossref] [Google Scholar] [PubMed]
- Laird A, Shekleton P, Nataraja RM, Kimber C, Pacilli M. Incidence of gastro-intestinal anomalies and surgical outcome of fetuses diagnosed with echogenic bowel and bowel dilatation. Prenat Diagn 2019;39(12):1115-9.
[Crossref] [Google Scholar] [PubMed]
- Galani A, Zikopoulos A, Papandreou L, Mastora E, Zikopoulos K, Makrydimas G. Prenatal diagnosis of fetal jejunal atresia: A case report. Cureus 2021;13(10):e18947.
[Crossref] [Google Scholar] [PubMed]
- Robertson JA, Kimble RM, Stockton K, Sekar R. Antenatal ultrasound features in fetuses with gastroschisis and its prediction in neonatal outcome. Aust N Z J Obstet Gynaecol 2017;57(1):52-6.
[Crossref] [Google Scholar] [PubMed]
- Lap CC, Voskuilen CS, Pistorius LR, Mulder EJ, Visser GH, Manten GT. Reference curves for the normal fetal small bowel and colon diameters; their usefulness in fetuses with suspected dilated bowel. J Matern Fetal Neonatal Med 2020;33(4):633-8.
[Crossref] [Google Scholar] [PubMed]
- Lau TK, Fung YM, Fung TK. Fetal bowel dilatation-report of 3 cases with different perinatal outcomes. Aust N Z J Obstet Gynaecol 1997;37(3):323-4.
[Crossref] [Google Scholar] [PubMed]
- de Becdelievre A, Costa C, Jouannic JM, LeFloch A, Giurgea I, Martin J, et al. Comprehensive description of CFTR genotypes and ultrasound patterns in 694 cases of fetal bowel anomalies: A revised strategy. Hum Genet 2011;129:387-96.
[Crossref] [Google Scholar] [PubMed]
- Contro E, Fratelli N, Okoye B, Papageorghiou A, Thilaganathan B, Bhide A. Prenatal ultrasound in the prediction of bowel obstruction in infants with gastroschisis. Ultrasound Obstet Gynecol 2010;35(6):702-7.
[Crossref] [Google Scholar] [PubMed]
- Ruiz MJ, Thatch KA, Fisher JC, Simpson LL, Cowles RA. Neonatal outcomes associated with intestinal abnormalities diagnosed by fetal ultrasound. J Pediatr Surg 2009;44(1):71-5.
[Crossref] [Google Scholar] [PubMed]
- Babcook CJ, Hedrick MH, Goldstein RB, Callen PW, Harrison MR, Adzick NS, et al. Gastroschisis: Can sonography of the fetal bowel accurately predict postnatal outcome? J Ultrasound Med 1994;13(9):701-6.
[Crossref] [Google Scholar] [PubMed]
- Corteville JE, Gray DL, Langer JC. Bowel abnormalities in the fetus-correlation of prenatal ultrasonographic findings with outcome. Am J Obstet Gynecol 1996;175:724-9.
[Crossref] [Google Scholar] [PubMed]
- Adra AM, Landy HJ, Nahmias J, Gómez-Marín O. The fetus with gastroschisis: Impact of route of delivery and prenatal ultrasonography. Am J Obstet Gynecol 1996;174(2):540-6.
[Crossref] [Google Scholar] [PubMed]
- Zeng K, Li D, Zhang Y, Cao C, Bai R, Yang Z, et al. Prenatal diagnosis of megaduodenum using ultrasound: A case report. BMC Pregnancy and Childbirth 2021;21(1):370.
[Crossref] [Google Scholar] [PubMed]
- Dewberry LC, Hilton SA, Zaretsky MV, Behrendt N, Galan HL, Marwan AI, et al. Examination of prenatal sonographic findings: Intra-abdominal bowel dilation predicts poor gastroschisis outcomes. Fetal Diagn Ther 2020;47(3):245-50.
[Crossref] [Google Scholar] [PubMed]
- Ping LM, Rajadurai VS, Saffari SE, Chandran S. Meconium peritonitis: Correlation of antenatal diagnosis and postnatal outcome-an institutional experience over 10 years. Fetal Diagn Ther 2017;42(1):57-62.
[Crossref] [Google Scholar] [PubMed]
- Page R, Ferraro ZM, Moretti F, Fung Kee Fung K. Gastroschisis: Antenatal sonographic predictors of adverse neonatal outcome. J Pregnancy 2014;2014.
[Crossref] [Google Scholar] [PubMed]
- Lato K, Qweider M, Poellmann M, Knippel AJ, Bizjak G, Stressig R, et al. Fetal gastroschisis: A comparison of second vs. third-trimester bowel dilatation for predicting bowel atresia and neonatal outcomes. Ultraschall Med 2011;34(2):157-61.
[Crossref] [Google Scholar] [PubMed]