- *Corresponding Author:
- X. Ge
Department of Dermatovenereology, The First Affiliated Hospital of Bengbu Medical College, No. 287 Changhuai Road, Longzihu District, Bengbu, 233004, China
E-mail: dr_gexin0106@126.com
| This article was originally published in a special issue, |
| "Clinical and Experimental Studies on Drug and Intervention Repurposing in China" |
| Indian J Pharm Sci 2019:81(4)spl issue1;185-191 |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
In order to study the therapeutic effect of pregabalin on postherpetic neuralgia, patients with postherpetic neuralgia were studied. Pregabalin and other medicines for patients with neuralgia were analyzed in terms of physical pain, nausea and vomiting, quality of life, adverse reactions, sleep quality and satisfaction. The results showed that compared with other drugs in the treatment and drug response, pregabalin has a significant effect. In addition, many indicators of quality of life of patients after taking medicine were carefully studied. In conclusion, pregabalin has a good therapeutic effect on postherpetic neuralgia. Whether in alleviating physical pain or psychological problems such as emotional instability and irritability, pregabalin has a more significant positive effect on patients.
Keywords
Pregabalin, recovery, drug administration, detection
Postherpetic neuralgia is a common neuropathic pain in clinic[1]. It refers to the persistent pain after the clinical cure of acute herpes zoster for more than one month, or paroxysmal pain after acute stage for more than three months (that is, the onset of rash for four months)[2]. Its main characteristics are persistent and paroxysmal burning pain or deep jumping pain, spontaneous knife-like pain, abnormal pain and hyperalgesia. The incidence is 30-100/100 000 and increases with age[3].
Varicella zoster virus (VZV) manifests itself as varicella when it is first infected in childhood. When chickenpox is cured, most of the viruses are cleared[4]. A small amount of VZV pre-viral fragments will travel along the nerve roots from peripheral sensory nerve endings, and eventually host in spinal dorsal root ganglion or cerebral ganglion[5,6]. Because the virus integrates into the nucleus of neurons or surrounding satellite cells, it can escape the effect of high titer specific antibodies outside cells and remain in a latent state of nonreplication for a long time. However, it can be replicated in large quantities at any time[7]. Although the specific mechanism of VZV re-activation and replication is unknown, the decline of cellular immunity in vivo to a certain level is an important cause of herpes zoster attack. In middle-aged and elderly people and patients with low immune function, the number of memory cells and killer cells in vivo decreases significantly, and the incidence of herpes zoster increases accordingly[8]. Neuralgia can occur in 60~90 % of patients with herpes zoster in the acute stage[9]. Pain may be due to a large number of inflammatory mediators produced by obvious inflammation in the lesion area, which directly stimulates the peripheral sensory nerves in the lesion area. It may also be caused by severe inflammation that directly destroys axons and nerve cells, or by nerve damage caused by bleeding of inflamed neurons[10]. Acute neuralgia is usually aggravated by the progression of the lesion, and relieved after gradual absorption of the lesion. In addition to acute neuralgia, it can also be accompanied by abnormal pain[11].
Although the manifestations of acute pain vary greatly in different patients, most of them are significantly relieved or disappeared within a few days after the lesion is absorbed[12]. There is a significant correlation between the severity and duration of acute pain and the complication of herpes zoster, postherpetic neuralgia. The pathogenesis is still unclear[13]. Neuropathophysiological studies have found that the damage of nervous system caused by acute herpes zoster inflammation can lead to peripheral and central neuropathy. Degeneration of sensory organs in the lesion leads to abnormal synaptic regeneration in the central nervous system and hyperfunction of sensory organs is associated with hyperalgesia in the central nervous system. With the coming of population aging, the incidence of herpes zoster and postherpetic neuralgia increases year by year[14]. Because of its severe clinical symptoms and long duration, patients suffer from anxiety, depression and sleep disorders, which seriously affect their lives, so more and more researchers pay attention to it.
Pregabalin is a class of analogues of gammaaminobutyric acid (GABA), a neurotransmitter, and a continuing drug of gabapentin. The working mechanism of pregabalin for patients is similar to that of gabapentin[15]. In various animal experiments, pregabalin is effective against convulsions and pain relief, but the detailed mechanism of work is still not known accurately. Pregabalin is very close to GABA in molecular structure, but its internal working mechanism is different from GABA. In addition, pregabalin has different effects from other antiepileptic drugs[16]. In the required concentration, it will not react with GABA or GABA receptors, metabolize GABA or GABA by-products and have no effect on GABA absorption and decomposition[17]. It has no effect on sodium and calcium channels, and has no effect on glutamate absorption and excretion. At the same time, pregabalin does not react with amino acids such as glutamic acid and GABA, but pregabalin can replace H pregabalin and calcium receptor, hinder a class of subunits of central nervous system-dependent sodium channel α2-δ protein, and reduce sodium influx, which can reduce the release of neurotransmitters such as glutamate, norepinephrine and P product, and affect the neurotransmission function of GABA. In addition, pregabalin can greatly increase the expression level of GABA and increasing the dosage of pregabalin can significantly improve the activity of glutamate decarboxylase[18]. Pregabalin is a racemic compound with excellent liposolubility and can pass through the blood brain barrier. In terms of binding sites, the activity of (R) - isomers is only 1/10 of that of (S)- isomer[19].
To sum up, in this study, the recovery effect of pregabalin and other drugs in patients with postherpetic neuralgia was analysed. The results showed that, compared with other drugs, pregabalin was more effective in patients with postherpetic neuralgia. The innovative component lies in the perfect analysis of all indicators of pregabalin and other drugs after taking medicine and the feeling from the physical level to the psychological level. There are still some shortcomings in the process of this study, but the research results still provide some guidance for future research. Therefore, this research is a valuable research topic.
According to the selection requirements of clinical cases, 100 patients with postherpetic neuralgia were selected from January 2015 to December 2018 in the First Affiliated Hospital of Bengbu Medical College. All patients were randomly divided into experimental group and control group. The experimental group (n-50) was given pregabalin 160 mg/d orally, and the control group (n-50) was given carbamazepine 500 mg/d. The observation time was 4 w. The exclusion criteria were as follows, patients who have been treated earlier with pregabalin or carbamazepine or who have a history of allergies to pregabalin or carbamazepine, excipients or chemically similar drugs were excluded from the study. Secondly, patients with cardiovascular, liver, blood, endocrine or other systemic diseases and those who are difficult to complete clinical trials or to analyse the results of research were excluded. Thirdly, patients who cannot tolerate oral drugs or have a history of significant absorption disorders were excluded. Fourthly, patients who have taken other research drugs within 30 d before the start of the study were excluded. Fifthly, those who cannot complete the study due to mental illness or any other disease were excluded. Patients were excluded when the clinical process of this study was disturbed or when there was a significant risk to patients. Sixthly, patients with abnormal liver function, alanine aminotransferase and aspartate aminotransferase or serum creatinine >132.601 μmol/l are excluded from laboratory tests. Before treatment, diagnosis is needed to exclude other diseases. All patients need to undergo urine routine, blood routine, liver and kidney function and electrocardiogram examination, and sign the informed consent of the operation.
Pregabalin was purchased from Pfizer Pharmaceuticals in the United States. Carbamazepine was purchased from Beijing Novartis Pharmaceutical Co., Ltd.
Both groups of patients received the same routine treatment before the experiment began. Vitamin B2 tablets were taken orally for 30 mg twice a day. Methyldiamine needle was injected intramuscularly at 0.3 mg/d. On this basis, two groups of patients were given medicine according to the prescribed plan. In the experimental group, 80 mg of pregabalin was taken orally on the first day of treatment, which was increased to 160 mg on the second day, one tablet in the morning and one tablet in the evening. The patient was treated with pregabalin for 4 w.
Patients in the control group on the first day of treatment, before going to bed were given 80 mg carbamazepine orally. On the second day, carbamazepine dose was increased to 80 mg twice a day. From the d 3, it was increased to 80 mg thrice a day. This dose was given for 1 w. After a week, the dose gradually increased to 480 mg per day and the patients continued to take it three times a day until the end of the 4 w.
Drug withdrawal criteria for the 2 groups were, when adverse reactions occur, leading to patients cannot adhere to, drug was withdrawn. The medicine was stopped when other diseases occur in the process or the patient was requested to stop taking the medicine when it was found ineffective.
Pain index evaluation was through visual analogue scoring system (VAS) to evaluate pain. Pain was assessed 1 to 4 w before and after treatment. The pain was judged by the patient himself, and a straight line was chosen as the criterion (generally 15 cm). On the one hand, it means painless. On the other hand, it means very painful. Patients choose the pain value according to their own situation, and leave a mark at the corresponding position of the straight line. The distance between no pain markers is the patient's pain score. All markers were weighted according to VAS scoring system. VAS weighting= (pre-treatment VASpost- treatment VAS)/pre-treatment VAS. In addition, in the care of the observers, the patients carefully fill in the pain questionnaire, and the total score is from 0 to 45, as shown in Table 1.
| Therapeutic criteria | Cure | Markedly effective | Effective | Invalid |
|---|---|---|---|---|
| VAS weighting | >75 % | 50-75 % | 25-50 % | <25 % |
Table 1: Criteria for evaluating efficacy
Sleep quality was assessed using duration of sleep (h). The continuous sleep quality of patients was studied before and 1 to 4 w after treatment. Under the guidance of the observer, the patient fills in the questionnaire for the duration of sleep at night.
The quality of life of the patients in the two groups was assessed by using the Chinese quality of life scale, and the quality of life of the patients before and 4 w after medication was evaluated. Under the guidance of observers, all questionnaires were filled out and judged by the patients, and the influence of subjective factors was minimized, and all questionnaires were withdrawn.
All adverse reactions, including nausea and vomiting, dizziness, ataxia, peripheral oedema and sleepiness, were recorded at any time throughout the day in the experimental group and the control group. If there are uncontrollable adverse reactions, the drug should be stopped immediately and other measures should be taken as soon as possible. Blood routine and liver function tests are needed before and after the experiment was completed for 4 w.
The first is the nature and frequency of pain. Because in most cases, the physical pain of patients with postherpetic neuralgia is between moderate and severe, the physical unbearability of patients is accompanied by obvious fluctuations and changes in their emotions and psychology. Pain was characterized by spontaneous knife cutting or tearing pain. More than 40 % of patients with postherpetic neuralgia suffer from spontaneous knife cutting or tearing pain when pain occurs. Patients have almost no normal sleep time at night, which has a great impact on the quality of life. Many patients showed significant pain in the skin of the ward. Even if touched lightly with a cotton swab, it can cause heart tear and lung pain. As a result, most patients refused to wear clothes again for fear that the contact of clothes will bring them unbearable pain. Acupuncture-like pain accompanied by continuous burning is a general degree of pain, which will disturb normal rest sometimes. The patient may have hypersensitivity or paralysis of the skin in the ward. Although the frequency of pain is related to different types of post-herpes zoster neuralgia and neurological damage, the frequency of spontaneous pain in most patients is not clinically related, nor is it necessarily related to exercise. For this reason, most patients need to maintain a state of extreme tension at any time. Pain occurs, but it is not clear when it will occur, as shown in Table 2. The frequency of pain in most patients is less than 10 times/min, and each time is about several seconds. Some severe cases may occur more than 10 times/min. Persistent pain is more common in clinic.
| Classification | Description |
|---|---|
| Light | Patients can perceive symptoms, which are easily tolerated and can cause slight discomfort, but do not affect daily activities |
| moderate | Patients' discomfort is enough to affect their daily activities |
| severe | Extreme pain can cause significant functional impairment or loss of function, or interfere with normal daily activities |
Table 2: Classification criteria for severity of pain in patients
The second is symptoms associated with pain onset. In addition to pain symptoms, most patients with postherpetic neuralgia would experience varying degrees of ant sense, contraction, twitching and itching in the affected area. In terms of personal psychology and emotions, patients also have abnormal fluctuations and changes, such as depression, anxiety, inattention, irritability and so on. Due to the body level pain and treatment cannot bring ideal results, patients' normal life and sleep quality is greatly disturbed, and there is a significant resistance to treatment. More than 60 % of patients have a tendency to hurt themselves. In addition, due to the abnormal performance of patients, family life, adaptability and activity ability have been significantly reduced.
The third is diagnosis and clinical classification. Most patients with postherpetic neuralgia have a history of acute herpes zoster, and in the patient's affected area, skin pigments or traces with varying degrees of depth and shallowness left behind by herpes can be clearly seen. Especially according to the characteristics and nature of the pain complained by patients, only a few patients have no obvious skin pigments or traces in the ward, which will bring difficulties to doctors in diagnosis. At this time, it is necessary to carefully understand its past medical history and carefully examine the local skin. Researchers proposed postherpetic neuralgia subtype and classified it into irritation type, paralysis type, mixed type and non-irritation type. These 4 types of pain have certain diagnostic significance in clinic. Different kinds of postherpetic neuralgia may have different effects on the treatment methods, which indicates that the clinical treatment ideas should be different.
Noxious receptor excitation is mainly caused by excessive excitation of peripheral noxious receptor. Pain sensitivity is its characteristic clinical manifestation. Light touch can produce intense and unbearable pain, but denervation is not obvious. The clinical manifestation is obvious hyposensation or loss of superficial sensation, while the pain is not obvious. Central integrative pain is characterized by secondary sensitization or other abnormal changes of the central nervous system. It can be characterized by both type I and type II in clinic. No irritation or paralysis clinical examination show no significant change in sensation or abnormal pain, but the pain in the affected area is still obvious. This may be related to the type of damaged nerve fibres. Classification of subtypes of postherpetic neuralgia is of great value in clinical diagnosis. Different treatment schemes for different types of patients with postherpetic neuralgia have different results, which not only warns that clinical treatment thinking should be treated differently, but also helps to diagnose and follow-up in-depth treatment of postherpetic neuralgia.
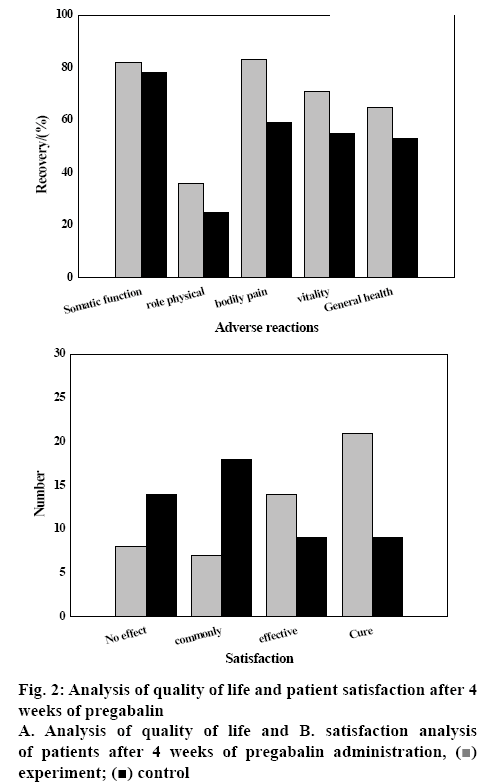
The analysis of body pain after taking pregabalin is shown in (fig. 1A), which indicated that the physical pain of patients after taking pregabalin decreases gradually over time. Compared to carbamazepine, the effect of pregabalin is more obvious, which indicated that pregabalin has a good effect in the treatment of postherpetic neuralgia. This is very important for the patient's continuous recovery after herpes zoster, which fully verifies that pregabalin has a good effect on postherpetic neuralgia.
The duration of persistent sleep after taking pregabalin was analysed and as shown in fig. 1B, the stable continuous sleep time of patients after taking pregabalin increased with time. By the 4 w, the sleeping time of the experimental group was about 6 h, while that of the control group was only 4 h. Over time, patients' sleep time would reach the normal level, sufficiently indicating that compared to carbamazepine, pregabalin has a significant effect on the treatment of postherpetic neuralgia.
Analysis of nausea and vomiting after taking pregabalin is shown in fig. 1C. Nausea and vomiting reactions of patients after taking pregabalin or carbamazepine were significantly different. Over time, the vomiting situation of patients in the experimental group has changed greatly. At the 4 w, fewer than 10 people vomited. The number of vomiting in the control group was close to 20. Thus, it can be seen that compared to carbamazepine, pregabalin has obvious therapeutic effect on postherpetic neuralgia.
The analysis of adverse reactions after taking pregabalin is shown in fig. 1D. From the picture, it can be seen that after taking pregabalin or carbamazepine, patients have different degrees of somnolence, oedema, vertigo and other adverse symptoms. Compared to the control group, the patients in the experimental group have more effect than carbamazepine, especially on oedema, which showed that pregabalin has a good effect on the adverse reactions of postherpetic neuralgia, which is very important for the continuous rehabilitation of patients after herpes zoster.
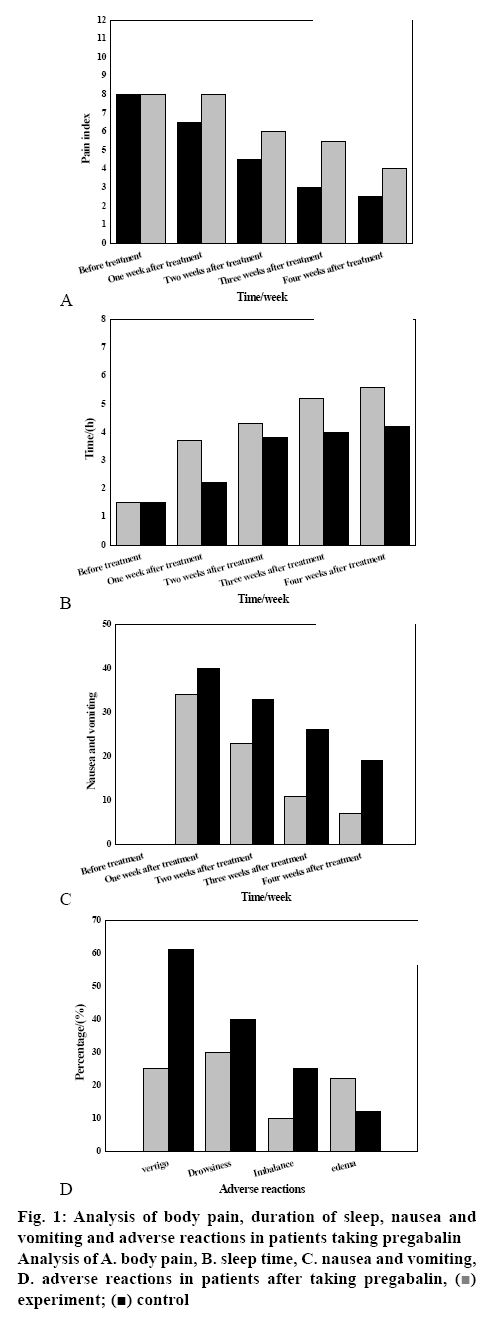
The quality of life of the patients after 4 w of administration of pregabalin was analysed as shown in (fig. 2A). The quality of life of patients after taking pregabalin or carbamazepine has been improved to varying degrees, manifested in physical function, physical role, body pain, vitality, general health, social function, emotional role, mental health and so on. The recovery effect of the experimental group was more pronounced than that of the control group. Thus, it can be seen that pregabalin has obvious therapeutic effect on postherpetic neuralgia compared with other drugs.
Survey and analysis of patient satisfaction after 4 w of administration of pregabalin are shown in fig. 2B. The satisfaction rate of the experimental group is higher than that of the control group. Most of the patients were satisfied, and most of them were cured and good. The patient's personal feedback was sufficient to illustrate the therapeutic effect of the drug and prove that pregabalin has a good effect on postherpetic neuralgia.
In this study, the effects of pregabalin or carbamazepine on postherpetic neuralgia were studied. The recovery indicators such as body pain, nausea and vomiting, quality of life, adverse reactions, sleep quality and satisfaction was analysed in detail. The results showed that compared to carbamazepine, pregabalin has better therapeutic effect and greatly alleviates the pain of patients. There are still some shortcomings in the research process in this study, such as the insufficient number of experimental samples, the different degree of illness of each patient and the different physical quality of the patients themselves, which would have an impact on the experiment. However, the innovation of this study lies in the detailed and effective study of the whole process of pregabalin treatment on the physical and psychological levels of patients and follow-up visits. The results provide valuable guidance for the continuous study of postherpetic neuralgia, so this study is a meaningful research topic.
References
- Mallick-Searle T, Snodgrass B, Brant JM. Postherpetic neuralgia: epidemiology, pathophysiology, and pain management pharmacology. J Multidiscip Healthc 2016;9:447.
- Goodman CW, Brett AS. Gabapentin and pregabalin for pain-is increased prescribing a cause for concern? N Engl J Med 2017;377(5):411-4.
- Wang BC, Liu D, Furnback WE, Bifa F, Dong P, Xie L, et al. The cost-effectiveness of pregabalin versus gabapentin for peripheral neuropathic pain (pNeP) and postherpetic neuralgia (PHN) in China. Pain Ther 2016;5(1):81-91.
- Price N, Namdari R, Neville J, Proctor KJ, Kaber S, Vest J, et al. Safety and efficacy of a topical sodium channel inhibitor (TV-45070) in patients with postherpetic neuralgia (PHN): a randomized, controlled, proof-of-concept, crossover study, with a subgroup analysis of the Nav1. 7 R1150W genotype. Clin J Pain 2017:33(4):310.
- Shinde SS, Seisler D, Soori G, Atherton PJ, Pachman DR, Lafky J, et al. Can pregabalin prevent paclitaxel-associated neuropathy?-An ACCRU pilot trial. Support. Care Cancer 2016;24(2):547-53.
- Liu Q, Chen H, Xi L, Hong Z, He L, Fu Y, et al. A Randomized, Double‐blind, Placebo‐controlled Trial to Evaluate the Efficacy and Safety of Pregabalin for Postherpetic Neuralgia in a Population of Chinese Patients. Pain Pract 2017;17(1):62-9.
- Schug SA, Parsons B, Almas M, Whalen E. Effect of concomitant pain medications on response to pregabalin in patients with postherpetic neuralgia or spinal cord injury-related neuropathic pain. Pain Physician 2017;20:E53-E63.
- Baron R, Allegri M, Correa-Illanes G, Hans G, Serpell M, Mick G, et al. The 5% lidocaine-medicated plaster: its inclusion in international treatment guidelines for treating localized neuropathic pain, and clinical evidence supporting its use. Pain Ther 2016;5(2):149-69.
- Mehta N, Bucior I, Bujanover S, Shah R, Gulati A. Relationship between pain relief, reduction in pain-associated sleep interference, and overall impression of improvement in patients with postherpetic neuralgia treated with extended-release gabapentin. Health Qual Life Out 2016;14(1):54.
- Shimony N, Amit U, Minz B, Grossman R, Dany MA, Gonen L, et al. Perioperative pregabalin for reducing pain, analgesic consumption, and anxiety and enhancing sleep quality in elective neurosurgical patients: a prospective, randomized, double-blind, and controlled clinical study. J Neurosurg 2016;125(6):1513-22.
- Emir B, Johnson K, Kuhn M, Parsons B. Predictive modeling of response to pregabalin for the treatment of neuropathic pain using 6-week observational data: a spectrum of modern analytics applications. Clin Ther 2017;39(1):98-106.
- Robertson K, Marshman LAG, Plummer D. Pregabalin and gabapentin for the treatment of sciatica. J Clin Neurosci 2016;26:1-7.
- Raman S, DeAngelis C, Bruera E, Chow R, Lechner B, Chow E. Does pregabalin still have a role in treating cancer-induced bone pain. J Clin Oncol 2016;34(6):524-6.
- Smith TJ, Marineo G. Treatment of postherpetic pain with scrambler therapy, a patient-specific neurocutaneous electrical stimulation device. Am J Hosp Palliat Care 2018;35(5):812-3.
- Mathieson S, Maher CG, Mclachlan AJ. Trial of Pregabalin for Acute and Chronic Sciatica. N Engl J Med 2017;376(12):1111.
- Evoy KE, Morrison MD, Saklad SR. Abuse and Misuse of Pregabalin and Gabapentin. Drugs 2017;77(4):1-24.
- Martinez V, Pichard X, Fletcher D. Perioperative pregabalin administration does not prevent chronic postoperative pain: systematic review with a meta-analysis of randomized trials. Pain 2017;158(5):775-83.
- Croker R, Smyth D, Walker AJ, Goldacre B. The clinician impact and financial cost to the NHS of litigation over pregabalin: a cohort study in English primary care. BMJ Open 2018;8(6):e022416.
- Chen RW, Liu H, An JX, Qian XY, Jiang YD, Cope DK, et al. Cognitive effects of electro-acupuncture and pregabalin in a trigeminal neuralgia rat model induced by cobra venom. J Pain Res 2017;10:1887-97.
 experiment;
experiment;  control
control