- *Corresponding Author:
- Shun Wang
Department of Acupuncture and Moxibustion, Heilongjiang University of Traditional Chinese Medicine, Harbin, Heilongjiang 150040, China
E-mail: hljwang123456@163.com
| This article was originally published in a special issue, “Clinical Advancements in Life Sciences and Pharmaceutical Research” |
| Indian J Pharm Sci 2024:86(5) Spl Issue “222-228” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
Multiple sclerosis is an autoimmune disease affecting the central nervous system with no current cure. This study aimed to investigate the clinical efficacy and safety of acupuncture and tuina combined with traditional Chinese medicine in patients with multiple sclerosis. A randomized controlled design was employed, with 120 multiple sclerosis patients divided into two groups, with 60 patients in each group. The treatment group was treated with acupuncture, massage combined with Chinese medicine Wendan decoction and the control group was treated with Western medicine. The treatment period was 12 w, with sessions 3 times per week. The primary outcome measure was the multiple sclerosis functional composite and secondary outcome measures included bladder function score, self-rating depression scale, quality of life score and the incidence of adverse events. The results showed that the treatment group performed significantly better than the control group in terms of multiple sclerosis functional composite, bladder function score, self-rating depression scale and quality of life (p<0.05). The incidence of adverse events in the treatment group was 6.67 %, which was significantly lower than the 18.33 % in the control group (p<0.05). In conclusion, acupuncture and tuina combined with traditional Chinese medicine demonstrated favorable clinical efficacy and safety in multiple sclerosis patients, improving neurological function, bladder function, mood and quality of life.
Keywords
Multiple sclerosis, acupuncture and tuina, traditional Chinese medicine, clinical observation
Multiple Sclerosis (MS) is an autoimmune disease affecting the central nervous system, characterized by multifocal, polymorphic and recurrent focal inflammation and demyelination of the brain, spinal cord and optic nerves[1]. The etiology of MS remains unclear but is thought to be associated with genetic, environmental, infectious and immunological factors. Clinical manifestations of MS are diverse and commonly include visual disturbances, limb numbness or weakness, ataxia, bladder dysfunction, and mood disorders[1]. The diagnosis of MS is primarily based on the McDonald criteria, which encompass clinical presentation, neuroimaging and cerebrospinal fluid analysis[2].
MS currently lacks a definitive cure and conventional Western medicine treatments mainly involve immunomodulators, immunosuppressants, corticosteroids and their primary goals are to control the frequency of relapses and delay disease progression. However, these drugs often exhibit unstable efficacy and are associated with numerous adverse reactions and side effects. As a result, many MS patients seek alternative or adjunctive therapies, such as acupuncture, massage and Traditional Chinese Medicine (TCM). Acupuncture and massage are integral components of TCM, known for their roles in regulating Qi and blood, unblocking meridians, balancing Yin and Yang and dispelling pathogenic factors. The therapeutic mechanisms of acupuncture and massage in treating MS may be related to several aspects. Stimulation of acupoints may regulate the neuroendocrine system, inhibit the release of inflammatory mediators and alleviate demyelination. Stimulation of acupoints can improve blood circulation, increase cerebral blood flow and promote neural repair. Stimulation of acupoints may regulate the immune system, suppress autoimmune responses and reduce immunoglobulin and complement deposition. Stimulation of acupoints may regulate emotions, alleviate depression and anxiety and enhance overall Quality of Life (QOL) [3,4].
Materials and Methods
Materials:
This study employed a randomized controlled design, enrolling a total of 120 MS patients who were divided into two groups with 60 patients in each group. Inclusion criteria includes patients meeting the McDonald criteria for diagnosing MS, aged between 18 and 65 y, with an Expanded Disability Status Scale (EDSS) score ranging from 2.0 to 6.5, absence of other severe conditions such as heart, liver, kidney or hematological diseases, no prior use of immunosuppressive agents or biologics for treating MS and voluntary participation in the trial with informed consent. Exclusion criteria included pregnancy or lactation, the presence of severe complications like severe infections or malignant tumors, contraindications for acupuncture or massage therapy, a history of allergies or intolerance to Chinese herbal medicine and the use of noninvestigational drugs or treatment methods during the trial. There was no significant difference in baseline characteristics between the two groups (Table 1).
| Index | Treatment group | Control group | p value |
|---|---|---|---|
| Gender (Male/female) | 28/32 | 26/34 | 0.72 |
| Age (y) | 41.3±8.7 | 40.5±9.2 | 0.59 |
| Weight (kg) | 63.4±10.3 | 64.2±11.1 | 0.67 |
| Height (cm) | 168.5±7.6 | 169.3±8.2 | 0.56 |
| Time of onset (mo) | 18.7±6.4 | 19.2±7.1 | 0.62 |
| Number of attacks (times) | 3.5±1.2 | 3.6±1.3 | 0.71 |
| EDSS score | 4.2±1.1 | 4.3±1.2 | 0.81 |
Table 1: Baseline Characteristics of two Patient Groups (n=60)
Methods:
Acupuncture and massage therapy: The treatment group patients received acupuncture and massage therapy in a supine position. Stainless steel needles with a length of 25 mm and a diameter of 0.25 mm were used for acupuncture. The following acupoints were selected for study including Baihui, Fengchi, Taiyang, Hegu, Quchi, Ganshu, Pishu, Shenshu, Sanyinjiao, Zusanli and others. Depending on the specific condition of the patient, acupoints were adjusted as needed. For patients with visual impairment, additional acupoints included Jingming, Sizhukong and Zanzhu[8]. For those with limb numbness or weakness, additional acupoints included Waiguan, Neiguan, Yanglingquan, and acupoints along the Foot Yangming meridian. For patients with ataxia, additional acupoints included Fengshi, Fengmen and Fengfu. For those with bladder dysfunction, additional acupoints included Qihai, Guanyuan, Zhongji and Zhongwan. For patients with emotional disorders, additional acupoints included Shenmen, Xinyu and Xinbao Yu.
Following the principles of TCM meridian theory, a balanced supplementation and drainage technique was used to stimulate the acupoints. Each acupuncture session lasted for 15 min, conducted three times a week, over a total of 12 w[9]. The massage therapy involved various traditional Chinese techniques including kneading, pressing, pinching and grasping. Following the principles of meridian theory, the massage began from the head and followed the pathways of the Foot Taiyang bladder meridian, Foot Shaoyang gallbladder meridian and Foot Yangming stomach meridian, moving downward until reaching the feet[10]. Simultaneously, based on the specific condition of the patient, the intensity and duration of massage were adjusted for corresponding areas[10]. For patients with visual impairment, the area around the eyes was massaged more intensively. For those with limb numbness or weakness, the extremities received increased attention. For patients with ataxia, the lumbar and back regions were massaged more intensely. For individuals with bladder dysfunction, the lower abdominal and perineal areas were given extra attention. For patients with emotional disorders, the chest and epigastric regions were massaged more intensively. Each massage session lasted for 30 min, conducted three times a w, over a total of 12 w.
Chinese medicine treatment:
Patients in the treatment group received acupuncture and massage therapy while concurrently taking a Chinese herbal decoction. Wendan decoction is a TCM formula primarily used for treating “restlessness and insomnia following a serious illness”. The formula consists of ingredients such as tangerine peel, Pinellia ternata, bamboo shavings, Aurantii Fructus Immaturus, Poria cocos and roasted licorice. It is effective in resolving phlegm, clearing heat, harmonizing the liver and gallbladder, eliminating restlessness and calming palpitations. Its action focuses on clearing rather than warming, distinctly different from formulas that warm and temper the gallbladder. In TCM, the liver is considered a firm organ that prefers free flow and detests suppression, while the gallbladder prefers tranquility and dislikes disturbance. Physiologically, the liver and gallbladder communicate with each other and their Qi has the characteristics of generating and ascending. If phlegm-heat evil Qi invades the liver and gallbladder, the loss of their mildness can lead to illness. Therefore, the name “Wendan decoction” is given to this formula, which can be used for the treatment of MS[11]. For individuals with bladder dysfunction, additional ingredients included Poria cocos and Alisma orientale[12]. For patients with emotional disorders, additional ingredients included Polygala tenuifolia and Longan aril. One dose of the decoction was taken daily, prepared by decoction in water, administered three times a week over a total of 12 w.
Conventional Western medicine treatment:
Patients in the control group received conventional Western medicine treatment, which primarily included the following categories. Firstly, immunomodulators such as interferon β-1a (Rebif), interferon β-1b (Betaferon) and glatiramer acetate (Copaxone). These were administered by subcutaneous or intramuscular injection, three times a w, over a total of 12 w, following the dosages and methods specified in the product instructions. Second, immunosuppressants such as mitoxantrone (Novantrone) and cyclophosphamide (Cytoxan). These were administered intravenously, once a month, for a total of three times, following the dosages and methods specified in the product instructions[13]. Third, corticosteroids such as methylprednisolone (Solu-Medrol) and dexamethasone (Decadron). These were administered intravenously or orally, once daily for 5 consecutive d, once a mo, for a total of three times, following the dosages and methods specified in the product instructions.
Observation index:
The main outcome measure in this study is the MS Functional Composite (MSFC), which comprises three components. Firstly, the 9-Hole Peg Test (9HPT) for assessing upper limb function; secondly, the 25-Foot Walk Test (25FWT) for evaluating lower limb function; and thirdly, the Paced Auditory Serial Addition Test (PASAT) for assessing cognitive function. A higher MSFC score indicates better neurological function. The secondary outcome measures in this study include the following. Bladder Function Score (BFS) which consists of three components including Frequency Index Score (FIS) for assessing urinary frequency, Incontinence Index Score (IIS) for evaluating urinary incontinence and Urgency Index Score (UIS) for assessing urinary urgency. Self-Rating Depression Scale (SDS) which comprises 20 items, with each item scored from 1 to 4, resulting in a total score range of 20 to 80. A higher SDS score indicates a greater degree of depression QOL score is based on 36 items covering four aspects including physical, psychological, social and environmental. A higher QOL score reflects a better QOL. The safety outcome measure in this study is the incidence of adverse events, including any adverse reactions caused by acupuncture, massage, Chinese herbal medicine or Western medicine treatments. Adverse events may encompass skin redness, bleeding, infection, nausea, vomiting, diarrhea, headache, dizziness, allergies and others[14].
Statistical methods:
Data processing and statistical analysis were performed using Statistical Package for Social Sciences (SPSS) 23.0 software in this study. Continuous variables are presented as mean±standard deviation and intergroup comparisons were conducted using the t-test or Analysis of Variance (ANOVA). Categorical data are expressed as frequencies or percentages and intergroup comparisons were made using the chi-square test or Fisher’s exact probability test. A significance level of p<0.05 was considered statistically significant.
Results and Discussion
Acupuncture and massage combined with TCM significantly improved the neurological function of MS patients. This conclusion was assessed using the MSFC score, which comprehensively reflects the neurological status of MS patients, including three components, viz. 25FWT, 9HPT and PASAT. These three components are used to evaluate motor function, hand-eye coordination and cognitive function, respectively. Scores for each component were converted to Z-scores and then averaged to obtain the MSFC. A higher MSFC indicates better neurological function.
According to the data in Table 2, the average MSFC score in the treatment group significantly improved after treatment. It increased from 0.34±0.12 before treatment to 0.56±0.14 after treatment. In contrast, the control group showed smaller improvement in MSFC, with an average score of 0.39±0.13 after treatment (compared to 0.33±0.11 before treatment), resulting in a modest increase of 0.06±0.07. These results indicate that combined treatment with acupuncture, massage and herbal decoctions can significantly enhance neurological function in patients with MS, including motor function, hand-eye coordination and cognitive function. This suggests that the MSFC significantly improves in the treatment group after receiving acupuncture, massage and herbal decoction therapy.
| Group | Pre-treatment | Post-treatment | Changing value | Rate of change |
|---|---|---|---|---|
| Treatment group | 0.34±0.12 | 0.56±0.14 | 0.22±0.09 | 64.71 % |
| Control group | 0.33±0.11 | 0.39±0.13 | 0.06±0.07 | 18.18 % |
| p-value | 0.82 | <0.01 | <0.01 | <0.01 |
Table 2: Mean MSFC Values and Changes before and after Treatment in both Groups (n=60)
BFS change serves as one of the secondary indicators for evaluating the impact of acupuncture, massage and herbal decoction treatment on bladder dysfunction in patients with MS. Bladder dysfunction is a common complication of MS and significantly affects patients’ QOL. In this study, BFS was used as the assessment parameter, comprising three components, FIS, IIS, and UIS, with a total score range of 0 to 15. A higher BFS indicates more severe bladder dysfunction.
Before treatment, there was no statistically significant difference in the average BFS values between the two patient groups (p>0.05), indicating similar baseline bladder function levels. However, after treatment, the average BFS value in the treatment group was significantly lower than that in the control group (p<0.05). The average BFS values and their changes before and after treatment for both groups are summarized in Table 3, visually reflecting the differences in bladder function between the two groups. These findings demonstrate that combined acupuncture, massage, and herbal decoction therapy (specifically the Wendan decoction) can significantly improve bladder dysfunction in MS patients, whereas conventional Western medication treatment does not yield significant efficacy (Table 4)[15,16].
| Group | Pre-treatment | Post-treatment | Changing value |
|---|---|---|---|
| Treatment group | 7.8±2.1 | 4.2±1.6 | -3.6±1.4 |
| Control group | 7.6±2.2 | 6.5±2.0 | -1.1±1.2 |
| p-value | 0.67 | <0.01 | <0.01 |
Table 3: Mean BFS Values and Changes before and after Treatment in both Groups (n=60)
| Group | Pre-treatment | Post-treatment | Changing value | Rate of change |
|---|---|---|---|---|
| Treatment group | 48.5±9.3 | 36.4±8.7 | -12.1±7.6 | -24.9±15.7 % |
| Control group | 47.8±9.5 | 43.2±9.1 | -4.6±6.8 | -9.6±14.2 % |
| p-value | 0.74 | <0.01 | <0.01 | <0.01 |
Table 4: Mean SDS Scores and Changes before and after Treatment in both Groups (n=60)
The evaluation of SDS is one of the secondary outcome measures used to assess the impact of acupuncture, massage and Chinese herbal medicine on the depressive state of MS patients. Depression is a common complication of MS, seriously affecting patients’ mental health and QOL. In this study, the SDS was used as the assessment tool. The SDS consists of 20 items, with each item scored from 1 to 4 points, resulting in a total score range of 20 to 80 points. A higher SDS score indicates a more severe level of depression[17]. The results showed that the baseline depression level was comparable between the two groups (p>0.05). After treatment, the average SDS score in the treatment group was significantly lower than that in the control group (p<0.05). This indicates that acupuncture, massage and herbal decoction therapy (specifically the Wendan decoction) can significantly improve the depressive state in patients with MS, whereas the efficacy of conventional Western medication treatment is not pronounced.
QOL assessment is one of the secondary outcome measures in this study, used to evaluate the impact of acupuncture, massage and Chinese herbal medicine on the QOL of MS patients. QOL refers to the subjective perception of patients in terms of physical, psychological, social and mental aspects and is an important indicator reflecting the health status and life satisfaction of patients. A higher QOL score indicates a better QOL. The results showed that there was no statistically significant difference in the mean QOL scores between the two groups before treatment (p>0.05), indicating that the baseline QOL was similar between the two groups. After treatment, the average QOL score in the treatment group was significantly higher than that in the control group (p<0.05). This indicates that acupuncture, massage and herbal decoction therapy can significantly improve the QOL in patients with MS, whereas the efficacy of conventional Western medication treatment is not pronounced. The mean QOL scores and their changes before and after treatment in both groups are presented in Table 5, and the data in Table 5, visually illustrate the differences in QOL between the two groups.
| Group | Pre-treatment | Post-treatment | Changing value | Rate of change |
|---|---|---|---|---|
| Treatment group | 63.2±12.4 | 75.6±10.8 | 12.4±9.6 | 19.6±15.2 % |
| Control group | 62.8±13.2 | 66.4±11.6 | 3.6±8.4 | 5.7±13.4 % |
| p-value | 0.82 | <0.01 | <0.01 | <0.01 |
Table 5: Mean QOL Scores and Changes before and after Treatment in both Groups (n=60)
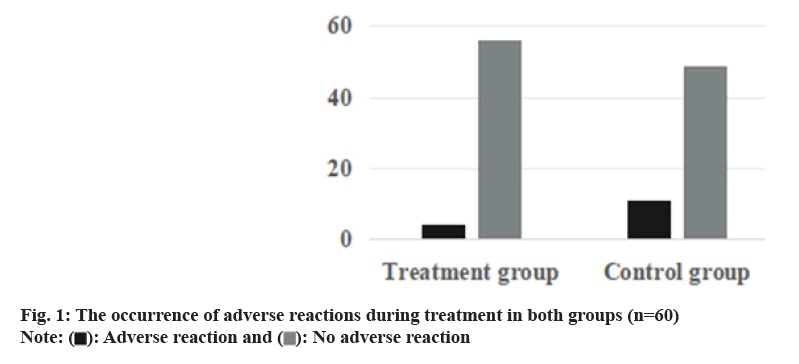
The incidence of adverse reactions in the treatment group was 6.67 %, which was lower than the 18.33 % observed in the control group and this difference was statistically significant (p<0.05) (fig. 1). The adverse reactions in the treatment group were primarily related to acupuncture and massage, resulting in mild skin redness, bleeding and infections, which resolved on their own after appropriate management. In the treatment group, adverse reactions related to Wendan decoction include mild nausea, vomiting and diarrhea. These adverse effects were mitigated through dose adjustments or compatibility modifications. In contrast, the control group experienced adverse reactions primarily due to Western medicine, such as headaches, dizziness, and allergies, with some patients requiring discontinuation or change of medication.
This study was to investigate the cli nical efficacy and safety of acupuncture and massage combined with Chinese medicine Wendan decoction in the treatment of MS[18,19]. The results demonstrate that this approach significantly improves patients’ neurological function, bladder function, depressive status and QOL with a lower incidence of adverse reactions compared to conventional Western medicine treatment[20]. It is suggested that acupuncture and massage combined with Wentan decoction is an effective and safe comprehensive treatment for MS, which can be used as an alternative or auxiliary treatment for MS. The improvement in neurological function in MS patients with acupuncture and massage combined with Chinese herbal medicine may be attributed to several factors. Firstly, it may regulate the neuroendocrine system by stimulating acupoints and meridians, suppressing the release of inflammatory mediators and alleviating demyelination. Secondly, it may enhance blood circulation by stimulating acupoints and meridians, increasing cerebral blood flow, and promoting nerve repair. Thirdly, it may modulate the immune system by stimulating acupoints and meridians, suppressing autoimmunity and reducing the deposition of immunoglobulins and complements. Fourthly, it may regulate emotions by stimulating acupoints and meridians, alleviating depression and anxiety, and improving QOL. These effects align with the theories and practices of acupuncture, massage and Chinese herbal medicine, as well as with the results of related research[21,22].
The improvement in bladder function in MS patients with acupuncture and massage combined with Chinese herbal medicine may be attributed to several factors. Firstly, it may regulate the neuro-muscular function of the bladder by stimulating acupoints and meridians, improving symptoms such as urinary frequency, incontinence, and urgency. Secondly, it may promote blood supply to the bladder by stimulating acupoints and meridians, enhancing the bladder’s resistance to complications like infections and stones. Third, the use of Wendan decoction to clear heat, diuresis, blood stasis, nourishing Yin tonifying kidney and other regulation of the bladder environment, balance bladder Yin and Yang. These effects align with the theories and practices of acupuncture, massage and Chinese herbal medicine as well as with the results of related research. The safety of acupuncture and massage combined with Chinese herbal medicine in MS patients may be attributed to several factors. Firstly, both the dosage and administration of acupuncture, massage and Chinese herbal medicine are in accordance with the principles and standards of TCM, avoiding excessive or unsuitable treatment. Secondly, the actions of acupuncture, massage and Chinese herbal medicine are mild, balanced and regulatory in nature, avoiding severe or adverse reactions. Thirdly, during the treatment process, patients’ responses and changes are closely monitored and any adverse reactions are promptly addressed or treatment plans adjusted[23,24]. These measures align with the theories and practices of acupuncture, massage and Chinese herbal medicine as well as with the results of related research [25,26]. While this study has achieved certain results, it has several limitations. Firstly, the sample size is relatively small and randomization may introduce bias, affecting the reliability of the results; secondly, the observation period is relatively short, making it difficult to assess long-term effects and relapse rates; thirdly, a placebo control group was not included, making it impossible to eliminate the influence of psychological factors; fourthly, other potential influencing factors, such as patients’ lifestyles, dietary habits and psychological states were not considered. Therefore, future clinical trials with larger sample sizes, longer durations and stricter designs are needed to validate the conclusions of this study.
Conflict of interests:
The authors declared no conflict of interests.
References
- Huang WJ, Chen WW, Zhang X. Multiple sclerosis: Pathology, diagnosis and treatments. Exp Ther Med 2017;13(6):3163-6.
[Crossref] [Google Scholar] [PubMed]
- Bertram-Ralph E. Treatments for multiple sclerosis. InnovAiT 2014;7(11):658-66.
- Torkildsen Ø, Myhr KM, Bø L. Disease?modifying treatments for multiple sclerosis: A review of approved medications. Eur J Neurol 2016;23:18-27.
[Crossref] [Google Scholar] [PubMed]
- Weideman AM, Tapia-Maltos MA, Johnson K, Greenwood M, Bielekova B. Meta-analysis of the age-dependent efficacy of multiple sclerosis treatments. Front Neurol 2017;8:577.
[Crossref] [Google Scholar] [PubMed]
- Giovannoni G. Disease-modifying treatments for early and advanced multiple sclerosis: a new treatment paradigm. Curr Opin Neurol 2018;31(3):233-43.
[Crossref] [Google Scholar] [PubMed]
- Satyal J, Pradeep KC, Shrestha R, Dhakal P. Acupuncture as a rehabilitative therapy in patient with multiple sclerosis: A case study. Annapurna J Health Sci 2021;1(2):36-8.
- Yong-ping F. Evaluation of curative effect of traditional chinese medicine on multiple sclerosis in clinical trial. J Liaoning Univ Tradit Chin Med 2011;5(7):8-15.
- Criado, Gonçalves, Jorge Pereira Machado ACMA, Greten H. Acupuncture treatment on gait problems in multiple sclerosis : A preliminary study. Medicine 2016;95(15):52-68.
- Chen H, Ma X, Si L, Chen Z, Lin X, Yang Y, et al. Traditional Chinese medicine in multiple sclerosis: Theory and practice. Curr Pharmacol Rep 2018;4:436-46.
- Guan H, Wang J, Zhu Y, Jia H, Zhang Y. Effectiveness of acupuncture for multiple sclerosis: A protocol for systematic review and meta-analysis. Medicine 2022;101(13):e29150.
[Crossref] [Google Scholar] [PubMed]
- Chen P, Zhao D. Discussion on the treatment of multiple sclerosis from the perspective of the liver. J Shandong Univ Tradit Chin Med 2023;47(1):33-7.
- Fangfang MA, Zhang H, Bingxue LI, Cheng P, Mingwei YU, Xiaomin WA. Acupuncture and moxibustion for malignant tumor patients with psychological symptoms of insomnia, anxiety and depression: A systematic review and Meta-analysis. J Tradit Chin Med 2023;43(3):441.
[Crossref] [Google Scholar] [PubMed]
- Liao Y, Du X, Fu Y, Liu L, Wei J, An Q, et al. Mechanism of traditional Chinese medicine in treating overactive bladder. Int Urol Nephrol 2023;55(3):489-501.
[Crossref] [Google Scholar] [PubMed]
- Wang Y, Feng W. Cancer-related psychosocial challenges. Gen Psychiatr 2022;35(5):e100871.
[Crossref] [Google Scholar] [PubMed]
- Nakaya N. Effect of psychosocial factors on cancer risk and survival. J Epidemiol 2014;24(1):1-6.
[Crossref] [Google Scholar] [PubMed]
- Negussie F, Giru BW, Yusuf NT, Gela D. Psychological distress and associated factors among cancer patients in public hospitals, Addis Ababa, Ethiopia: A cross-sectional study. BMC Psychol 2023;11(1):41.
[Crossref] [Google Scholar] [PubMed]
- Herschbach P, Keller M, Knight L, Brandl T, Huber B, Henrich G, et al. Psychological problems of cancer patients: A cancer distress screening with a cancer-specific questionnaire. Br J Cancer 2004;91(3):504-11.
[Crossref] [Google Scholar] [PubMed]
- Niedzwiedz CL, Knifton L, Robb KA, Katikireddi SV, Smith DJ. Depression and anxiety among people living with and beyond cancer: A growing clinical and research priority. BMC Cancer 2019;19:1-8.
[Crossref] [Google Scholar] [PubMed]
- NASA/MS Cooling Study Group. A randomized controlled study of the acute and chronic effects of cooling therapy for MS. Neurology 2003;60(12):1955-60.
[Crossref] [Google Scholar] [PubMed]
- Filippi M, Amato MP, Centonze D, Gallo P, Gasperini C, Inglese M, et al. Early use of high-efficacy disease?modifying therapies makes the difference in people with multiple sclerosis: An expert opinion. J Neurol 2022;269(10):5382-94.
[Crossref] [Google Scholar] [PubMed]
- Hua LH, Hersh CM, Tian F, Mowry EM, Fitzgerald KC. Clinical characteristics of a large multi-center cohort of people with multiple sclerosis over age 60. Mult Scler Relat Disord 2021;47:102637.
[Crossref] [Google Scholar] [PubMed]
- Salavisa M, Serrazina F, Ladeira AF, Correia AS. Discontinuation of disease-modifying therapy in MS patients over 60 years old and its impact on relapse rate and disease progression. Clin Neurol Neurosurg 2023;225:107612.
[Crossref] [Google Scholar] [PubMed]
- Lancaster K, Thomson SJ, Chiaravalloti ND, Genova HM. Improving mental health in Multiple Sclerosis with an interpersonal emotion regulation intervention: A prospective, randomized controlled trial. Mult Scler Relat Dis 2022;60:103643.
[Crossref] [Google Scholar] [PubMed]
- Norrbrink C, Lundeberg T. Acupuncture and massage therapy for neuropathic pain following spinal cord injury: An exploratory study. Acupunct Med 2011;29(2):108-15.
[Crossref] [Google Scholar] [PubMed]
- Romero SA, Emard N, Baser RE, Panageas K, MacLeod J, Walker D, et al. Acupuncture versus massage for pain in patients living with advanced cancer: A protocol for the IMPACT randomised clinical trial. BMJ Open 2022;12(9):e058281.
- Zhou Z, Wang Y, Zhang C, Meng A, Hu B, Yu H. Design and massaging force analysis of wearable flexible single point massager imitating traditional Chinese medicine. Micromachines 2022;13(3):370.
[Crossref] [Google Scholar] [PubMed]