- *Corresponding Author:
- Qing Liang Chen
Tianjin Medical University Heping, Wuqing, Tianjin 300070, Department of Cardiovascular Surgery, Tianjin Chest Hospital, Jinnan, Tianjin 300300, China
E-mail: doctor_chen068@163.com
| This article was originally published in a special issue, “Current Trends in Pharmaceutical and Biomedical Sciences” |
| Indian J Pharm Sci 2022:84(5) Spl Issue “322-327” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
To investigate the clinical efficacy of atorvastatin combined with ezetimibe in preventing restenosis after coronary artery bypass grafting. Total 100 patients in Tangshan Workers’ Hospital were randomly divided into observation group and control group. The control group received 100 mg aspirin, 75 mg clopidogrel and atorvastatin 20 mg once a day. The observation group was given 10 mg ezetimibe once a day in addition to the above drugs. The venous diameter, blood lipid level changes, inflammatory response, quality of life, adverse reactions and treatment effects were assessed. After treatment for 6 mo, hypersensitive C-reactive protein and interleukin-6 levels were lower in observation group than control group. Total cholesterol, triglyceride and low-density lipoprotein cholesterol levels were lower and high-density lipoprotein cholesterol level was higher in observation group than control group. The observation group exhibited higher rates of vein garft stenosis improvement, lower rates of disease progression, lower incidence of major adverse cardiovascular events and higher 36-Item Short-Form Health survey scores than control group. The efficacy of ezetimibe combined with atorvastatin in treating restenosis after coronary artery bypass grafting is good, which also controls blood lipids with low incidence of adverse reactions.
Keywords
Coronary artery bypass grafting, restenosis, atorvastatin, ezetimibe
Coronary Artery Bypass Grafting (CABG) is a vital means for the treatment of coronary heart disease, but the restenosis of grafted veins seriously affects the prognosis of the operation. At present, “dual-antiplatelet therapy” is mainly used for graft restenosis, but the risk of venous graft restenosis is still very high[1]. A randomized clinical trial showed that 3 mo after CABG, 14.3 % of patients taking aspirin antiplatelet for therapy had venous graft occlusion and 8.4 % of patients taking aspirin plus clopidogrel for “dual-antiplatelet therapy” still had venous graft occlusion[2]. The reason is that intimal hyperplasia caused by the proliferation and migration of transplanted vein-media smooth muscle cells is a key factor in restenosis[3].
At present, the drugs taken by patients after CABG have little effect on alleviating the intimal hyperplasia of the grafted vein[4]. Therefore, how to inhibit venous graft restenosis is still the focus and difficulty of coronary heart disease surgery. Clinical studies have revealed that statins, as methylglutaryl-Coenzyme A (CoA) reducing agents, can improve the condition of patients with intracranial artery stenosis[2], but the clinical efficacy underlying venous graft restenosis is still unclear. The study attempted to clarify clinical efficacy of atorvastatin combined with ezetimibe in preventing restenosis after CABG.
Materials and Methods
General data:
A total of 100 patients undergoing CABG in Tangshan Workers’ Hospital from January 2021 to December 2021 were enrolled, including 58 males and 42 females, who all signed informed consent.
Inclusion criteria: Age ≥18 y; first-time thoracotomy CABG, with or without cardiopulmonary bypass and at least one graft vessel using the great saphenous vein.
Exclusion criteria: Concurrent other cardiovascular surgery, such as valve replacement, valve repair or radiofrequency ablation, etc.; redo CABG; emergency CABG; vascular anastomosis using a stapler; performing coronary endarterectomy; left ventricular repair due to ventricular aneurysm; combined with malignant tumors or other serious systemic diseases; severe renal insufficiency (creatinine >200 μmol/l) and unable to tolerate dual-antiplatelet therapy, such as severe peptic ulcer; participated in other clinical studies.
Treatment methods:
The patients were randomly divided into control group and observation group. The control group received drugs after CABG were aspirin 100 mg, once a day; clopidogrel 75 mg, once a day and atorvastatin 20 mg, once a day. The observation group was given ezetimibe in addition to the above conventional drugs, 10 mg/ time, once/d and the treatment cycle was 6 mo.
Observation indicators:
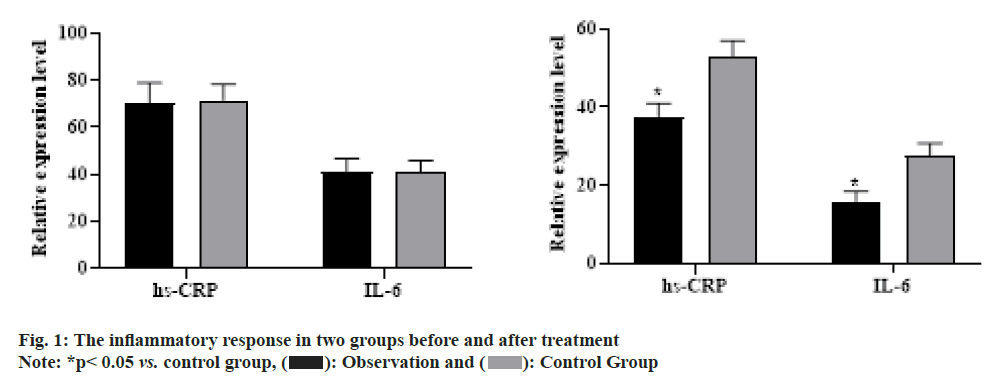
Multislice computed tomography angiography was performed 3 mo and 6 mo after the operation and the curved venous graft was “straightened” by computer reconstruction. The computed tomography angiography images of the venous graft were selected from 5 fixed measurement points (the anastomosis at both ends of the venous graft, the midpoint of the venous graft and 2 cm from the anastomosis), the inner diameter of the blood vessel was measured and the average value was obtained finally.
The levels of blood lipid indicators such as Triglyceride (TG), Total Cholesterol (TC), Low-Density Lipoprotein Cholesterol (LDL-C) and High-Density Lipoprotein Cholesterol (HDL-C), etc., in the two groups before and after treatment were observed.
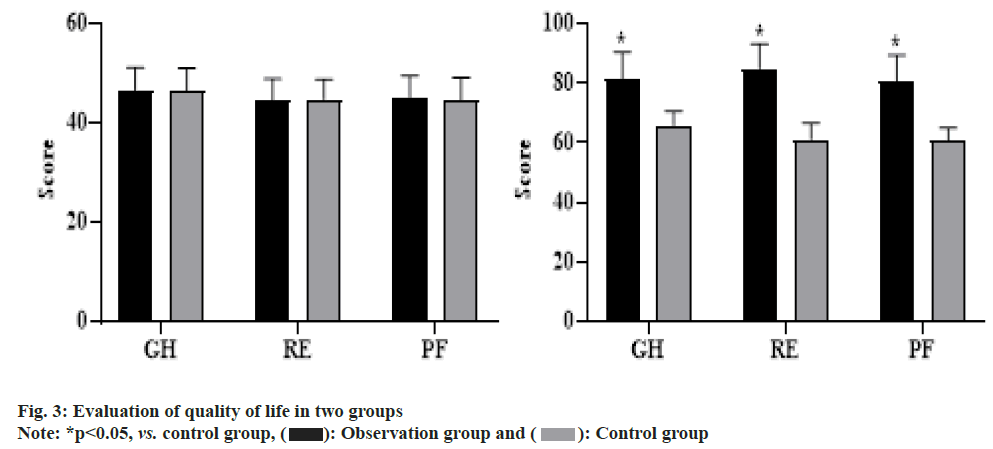
Inflammatory response is blood collection time and serum preparation were the same as blood lipid detection and serum high-sensitivity C-Reactive Protein (hs-CRP) and Interleukin-6 (IL-6) were detected by enzyme-linked immunosorbent assay.
Quality of life judging by 36-Item Short Form Survey (SF-36), this study focused on evaluating “General Health (GH)”, “Role-Emotional (RE)” and “Physiological Functioning (PF)”. As the score increased, it indicated that the quality of life was improved.
The adverse drug reactions during treatment and the occurrence of Major Adverse Cardiovascular Events (MACE) after 6 mo of treatment were recorded in the two groups.
Statistical analysis:
Statistical Package for Social Sciences (SPSS) 20.0 software was used for statistical analysis. Measurement data were expressed as (x±s), using t test; count data were expressed as rate (%), using Chi-square (χ2) test. p<0.05 meant that the difference was statistically significant.
Results and Discussion
Among the 100 enrolled patients, there were no postoper ative deaths and no early withdrawal from the trial in both groups. Basic clinical data presented no difference between the two groups p>0.05 as shown in Table 1.
| Clinical data | Control group | Observation group | χ2 | p |
|---|---|---|---|---|
| Age (year) | 59.5±4.2 | 59.1±4.6 | 0.253 | 0.872 |
| Male | 27 (54.0) | 29 (58.0) | 0.01 | 0.441 |
| Height (cm) | 171.6±3.5 | 170.8±4.3 | -0.153 | 0.896 |
| Weight (kg) | 70.4±10.2 | 70.8±10.8 | -0.927 | 0.328 |
| Hypertension | 33 (66.0) | 31 (62.0) | 0.332 | 0.332 |
| Diabetes | 9 (18.0) | 9 (18.0) | 0.309 | 0.358 |
| Hyperlipidemia | 8 (16.0) | 10 (20.0) | 0.454 | 0.341 |
| History of smoking | 23 (46.0) | 26 (52.0) | 0.278 | 0.312 |
| Family history | 22 (44.0) | 23 (46.0) | 0.013 | 0.519 |
| Left ventricular ejection fraction (%) | 44.7±6.2 | 45.1±7.6 | -0.826 | 0.551 |
| Myocardial infarction | 11 (22.0) | 10 (20.0) | 0.027 | 0.637 |
Table 1: General Data in Two Groups
Before treatment, hs-CRP and IL-6 presented no difference between two groups (p>0.05). After 6 mo of treatment, hs-CRP and IL-6 in the two groups were lower than before treatment, observation group was lower than control group and presented statistical difference as shown in fig. 1.
The venous graft inner diameter between two groups was compared, observation group was higher than control group at 3 mo and 6 mo after operation and presented statistical difference (p<0.05, fig. 2).
Before treatment, TC, TG, HDL-C and LDL-C levels presented no difference between two groups (p>0.05). After treatment, TC, TG and LDL-C levels were lower and HDL-C level was higher than those before treatment in two groups, TC, TG and LDL-C levels were lower and HDL-C level was higher in observation group than those in control group and presented statistical difference (p<0.05, Table 2). After 6 mo of treatment, the improvement rate of vein garft stenosis in study group was higher than that in control group (p<0.05) and the disease progression rate in study group was lower than that in control group (p<0.05, Table 3).
| Group | n | TC | TG | HDL-C | LDL-C | ||||
|---|---|---|---|---|---|---|---|---|---|
| Before treatment | After treatment | Before treatment | After treatment | Before treatment | After treatment | Before treatment | After treatment | ||
| Control group | 50 | 8.16±2.17 | 5.97±1.08* | 2.98±0.33 | 1.89±0.07* | 1.11±0.03 | l.96±0.15* | 4.57±0.71 | 3.28±0.27* |
| Observation group | 50 | 8.19±2.14 | 3.86±0.25*# | 2.94±0.31 | 1.15±0.05*# | 1.13±0.11 | 2.76±0.14*# | 4.61±0.68 | 3.11±0.22#* |
| t | 0.071 | 2.667 | 0.637 | 3.353 | 1.265 | 3.274 | 0.293 | 3.52 | |
| p | 0.944 | 0.009 | 0.526 | <0.001 | 0.209 | 0.0003 | 0.772 | <0.001 | |
Note: *p<0.05 vs. before treatment and #p<0.05 vs. control group
Table 2: The Blood Lipid Indicators in Two Groups
| n | Improved | Stable | Progressed | |
|---|---|---|---|---|
| Control group | 50 | 25 (50.00) | 20 (40.00) | 5 (10.00) |
| Observation group | 50 | 17 (34.00) | 21 (42.00) | 11 (22.00) |
| χ2 | 3.741 | 0.531 | 2.753 | |
| p | 0.015 | 0.841 | 0.026 |
Note: *p<0.05, vs. control group
Table 3: Evaluation of the Treatment Effect in Two Groups
After 6 mo of treatment, MACE incidence in observation group was markedly lower than that in control group (p<0.05). No significant adverse drug reactions occurred in two groups during treatment period as shown in Table 4.
| Observation group n (%) | Control group n (%) | χ2 | p | |
|---|---|---|---|---|
| Stable angina | 1 (2.00) | 3 (6.00) | ||
| Unstable angina | 1 (2.00) | 4 (8.00) | ||
| Acute myocardial infarction | 1 (2.00) | 2 (4.00) | ||
| Total | 3 (6.00) | 9 (18.00) | 5.217 | 0.017 |
Note: *p<0.05, vs. control group
Table 4: The Occurrence of Adverse Reactions in Two Groups
SF-36 (GH, RE, PF) presented no difference between groups before intervention (p>0.05); after 6 mo of intervention, relative to control group, the above indicators in observation group presented elevation (p<0.05, fig. 3).
Coronary heart disease is the leading cause of death worldwide. CABG, which restores myocardial perfusion (revascularization) of coronary heart disease patients by transplanting autologous blood vessels, is a widely used clinical treatment method[5]. The great saphenous vein has become the graft vessel of choice in 80 % of CABG revascularization due to its long length and superficial anatomical location[6]. However, venous graft restenosis requires a second operation, which severely limits the efficacy of CAB [7,8].
Venous graft restenosis, primarily due to the development of “arterial” atherosclerosis after venous grafting into the arterial environment. Dyslipidemia is the main cause of arteriosclerosis and a risk factor for coronary heart disease. The patients’ hyperlipidemia leads to massive lipid deposition on the vascular endothelium, causing proliferation and calcification of endothelial cells, resulting in gradual narrowing or even occlusion of the lumen. Dyslipidemia can be reflected in increased TG, TC and LDL-C levels and decreased HDL-C level[9]. All lipid regulation guidelines stipulate that the main purpose of lowering blood lipids is to reduce LDL-C and TC levels. Atorvastatin calcium, as a kind of 3-Hydroxy-3-Methylglutaryl-CoA (HMGCoA) reductase, can highly compete with it for the reaction of CoA in a selective manner, thereby inhibiting its activity and blocking cholesterol from binding to HMG-CoA reductase to reduce plasma free lipoprotein and cholesterol levels, while increasing LDL receptors in liver cells, accelerating LDL metabolism and reducing LDL-C and TC levels, but it is not sensitive to regulation of HDL-C and TG[10]. Ezetimibe, a newly-developed drug, is a highly selective drug that interferes with cholesterol absorption. It can inhibit the protein in the small intestine to transport cholesterol, thereby inhibiting the function of intestinal absorption of cholesterol, regulating plasma free cholesterol level, and reducing cholesterol storage level in the liver. This product can be used in combination with atorvastatin calcium to reduce LDL-C level[11]. While controlling a high-fat diet, it can be used independently to regulate blood lipids or in combination with HMG-CoA reductase inhibitors (statins) to treat hypercholesterolemia caused by various factors, which can significantly reduce plasma LDL-C, TC and Apolipoprotein B (ApoB) levels. According to the tests, under the action of conventional dosage, atorvastatin calcium can reduce LDL-C level by 30 %-40 %, but after increasing the dosage, LDL-C reduction only increases by 7 % and in the intestine, 50 %-60 % of cholesterol is still ingested, so it is necessary to inhibit the reabsorption of cholesterol in the intestine[12]. Ezetimibe regulates cholesterol by inhibiting the reabsorption of cholesterol in the intestine, so it is a new type of anti-hyperlipidemic drug relative to statins. The pharmacological mechanism of the drug is to interfere with the transport of cholesterol by Niemann-Pick C1-Like 1 (NPC1L1) protein in the brush edge of the small intestine, so that the small intestine cannot fully absorb a large amount of cholesterol and it can also prevent the liver from storing and transporting cholesterol, so as to regulate cholesterol level in the liver and increase the number of LDL-C receptors and accelerate the metabolism of cholesterol in plasma[13]. The combination of ezetimibe and atorvastatin can exert a synergistic effect, which can simultaneously prevent blood lipids from endogenous production and exogenous uptake and can significantly reduce cholesterol level in plasma, reduce blood lipids and slow down hardening trend of arteries. According to relevant tests, the probability of increase in transaminase in patients who use this product in combination with statins is 2.1 %, while the probability of increase in transaminase in patients who use statins alone is only 0.5 %. Moreover, this form of rise has no obvious clinical manifestations, does not cause the accumulation of bile and can return to normal levels after a period of treatment. In many literatures, there are many reports of ezetimibe combined with statins for the treatment of hyperlipidemia. The combination of ezetimibe and low-dose statins significantly reduced LDL-C level and achieved better results than statins alone[14]. Additionally, the combination of ezetimibe and simvastatin had a better effect on elderly patients with elevated blood lipids, with good acceptance of patients and fewer adverse reactions in the liver, gastrointestinal tract and muscle[15]. Herein, before treatment, TC, TG, HDL-C and LDL-C levels presented no difference between two groups. After treatment, TC, TG and LDL-C levels in two groups presented depletion and the level of HDL-C level presented elevation relative to those before treatment. TC, TG and LDL-C levels were lower and HDL-C level was higher in combined group than those in single group. The differences were statistically significant, indicating that atorvastatin combined with ezetimibe can effectively reduce the blood lipid level of patients after CABG, which is beneficial to the recovery process of patients.
Studies have revealed that atorvastatin up regulates the activity of endothelial nitric oxide synthase, accelerates endothelial repair and reduces the release of tissue factor from macrophages[16]. Atorvastatin can also inhibit the accumulation of inflammatory cells to the lesion site, thereby effectively reducing the synthesis and release of inflammatory cytokines and reducing endothelial inflammatory response. Herein, serum hs-CRP and IL-6 levels presented decrease in coronary heart disease patients in observation group relative to control group, the reason is related to the anti-inflammatory role of ezetimibe. It has been reported that taking ezetimibe alone can effectively reduce hs-CRP and the effect is independent of the lipid-lowering effect[17], but the antiinflammatory mechanism of ezetimibe remains elusive, whether there is a synergistic effect with statins needs further study. Recently, regardless of lipid-lowering drug, decrease of lipid level has association with regulation of inflammatory responses[18]. Herein, the decrease in hs- CRP and IL-6 caused by atorvastatin in combination with ezetimibe or atorvastatin alone can be partly attributed to the decrease in LDL-C level. Moreover, due to the enhanced curative effect and fewer adverse reactions when combined with medication, the patients’ physical discomfort can be relieved as soon as possible and the confidence in cure can be enhanced. In addition, the side effects are mild, the treatment risk will not be increased and the patients can be given a sense of security, so it can also improve the quality of life. Therefore, the results demonstrated that the qualities of life were better and the incidence of adverse reactions was lower in observation group than those in control group.
In conclusion, in the treatment of restenosis after CABG, the combination of ezetimibe and atorvastatin has a very good effect, which can not only ensure the therapeutic effect, but also control blood lipids and the incidence of adverse reactions is very low, improving the quality of life of patients, which is worthy of good promotion in clinical treatment.
Acknowledgement:
Run Sheng Wei and Dan Wang have contributed equally to this work.
Conflict of interests:
The authors declare that no conflict of interests associated with this work.
References
- de Stephan CM, Schneider DJ. Antiplatelet therapy for patients undergoing coronary artery bypass surgery. Kardiol Pol 2018;76(6):945-52.
[Crossref] [Google Scholar] [Pub Med]
- Gao G, Zheng Z, Pi Y, Lu B, Lu J, Hu S. Aspirin plus clopidogrel therapy increases early venous graft patency after coronary artery bypass surgery: A single-center, randomized, controlled trial. J Am Coll Cardiol 2010;56(20):1639-43.
[Crossref] [Google Scholar] [Pub Med]
- Neumann FJ, Sousa-Uva M, Ahlsson A, Alfonso F, Banning AP, Benedetto U, et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J 2019;40(2):87-165.
[Crossref] [Google Scholar] [Pub Med]
- Velazquez EJ, Lee KL, Jones RH, Al-Khalidi HR, Hill JA, Panza JA, et al. Coronary-artery bypass surgery in patients with ischemic cardiomyopathy. N Engl J Med 2016;374(16):1511-20.
[Crossref] [Google Scholar] [Pub Med]
- Spadaccio C, Benedetto U. Coronary artery bypass grafting (CABG) vs. percutaneous coronary intervention (PCI) in the treatment of multivessel coronary disease: Quo vadis?-A review of the evidences on coronary artery disease. Ann Cardiothorac Surg 2018;7(4):506-15.
[Crossref] [Google Scholar] [Pub Med]
- Khan Y, Cheema MA, Abdullah HM, Sattar Y, Haq S, Balaratna A, et al. Great saphenous vein stump: A risk factor for superficial/deep venous thrombosis and an indication for prophylactic anticoagulation?-A retrospective analysis. J Community Hosp Intern Med Perspect 2019;9(6):473-6.
[Crossref] [Google Scholar] [Pub Med]
- McKavanagh P, Yanagawa B, Zawadowski G, Cheema A. Management and prevention of saphenous vein graft failure: A review. Cardiol Ther 2017;6(2):203-23.
[Crossref] [Google Scholar] [Pub Med]
- Gaudino M, Benedetto U, Fremes S, Ballman K, Biondi-Zoccai G, Sedrakyan A, et al. Association of radial artery graft vs. saphenous vein graft with long-term cardiovascular outcomes among patients undergoing coronary artery bypass grafting: A systematic review and meta-analysis. JAMA 2020;324(2):179-87.
[Crossref] [Google Scholar] [Pub Med]
- Wang X, Tian M, Zheng Z, Gao H, Wang Y, Wang L, et al. Rationale and design of a multicenter randomized trial to compare the graft patency between no-touch vein harvesting technique and conventional approach in coronary artery bypass graft surgery. Am Heart J 2019;210:75-80.
[Crossref] [Google Scholar] [Pub Med]
- Shah B, Pillinger M, Zhong H, Cronstein B, Xia Y, Lorin JD, et al. Effects of acute colchicine administration prior to percutaneous coronary intervention: COLCHICINE-PCI randomized trial. Circ Cardiovasc Interv 2020;13(4):e008717.
[Crossref] [Google Scholar] [Pub Med]
- Cao BJ, Wang XW, Zhu L, Zou RJ, Lu ZQ. Dedicator of cytokinesis 2 silencing therapy inhibits neointima formation and improves blood flow in rat vein grafts. J Mol Cell Cardiol 2019;128:134-44.
[Crossref] [Google Scholar] [Pub Med]
- Bach RG, Cannon CP, Giugliano RP, White JA, Lokhnygina Y, Bohula EA, et al. Effect of simvastatin-ezetimibe compared with simvastatin monotherapy after acute coronary syndrome among patients 75 years or older: A secondary analysis of a randomized clinical trial. JAMA Cardiol 2019;4(9):846-54.
[Crossref] [Google Scholar] [Pub Med]
- Ouchi Y, Sasaki J, Arai H, Yokote K, Harada K, Katayama Y, et al. Ezetimibe lipid-lowering trial on prevention of atherosclerotic cardiovascular disease in 75 or older (EWTOPIA 75) a randomized, controlled trial. Circulation 2019;140(12):992-1003.
[Crossref] [Google Scholar] [Pub Med]
- Poh KK, Chin CT, Tong KL, Tan JK, Lim JS, Yu W, et al. Cholesterol goal achievement and lipid-lowering therapy in patients with stable or acute coronary heart disease in Singapore: Results from the dyslipidemia international study II. Singapore Med J 2019;60(9):454-62.
[Crossref] [Google Scholar] [Pub Med]
- Menotti A, Puddu PE, Adachi H, Tolonen H, Kafatos A. Association of serum cholesterol with coronary heart disease mortality during 50-year follow-up in ten cohorts of the seven countries study. Nutr Metab Cardiovasc Dis 2020;30(8):1337-46.
[Crossref] [Google Scholar] [Pub Med]
- Wang J, Ai XB, Wang F, Zou YW, Li L, Yi XL. Efficacy of ezetimibe combined with atorvastatin in the treatment of carotid artery plaque in patients with type 2 diabetes mellitus complicated with coronary heart disease. Int Angiol 2017;36(5):467-73.
[Crossref] [Google Scholar] [Pub Med]
- Sakuma M, Toyoda S, Hashimoto R, Yazawa H, Masuyama T, Hirose S, et al. Add-on ezetimibe treatment to low-dose statins vs. medium-intensity statin monotherapy in coronary artery disease patients with poorly controlled dyslipidemia. Hypertens Res 2019;42(12):1923-31.
[Crossref] [Google Scholar] [Pub Med]
- Liu D, Shen T, Ren C, Xu S, Zhou L, Bai J, et al. The effects of atorvastatin and rosuvastatin on exercise tolerance in patients with coronary heart disease. Expert Opin Drug Saf 2020;19(9):1203-8.
[Crossref] [Google Scholar] [Pub Med]
 : Observation and
: Observation and  : Control Group
: Control Group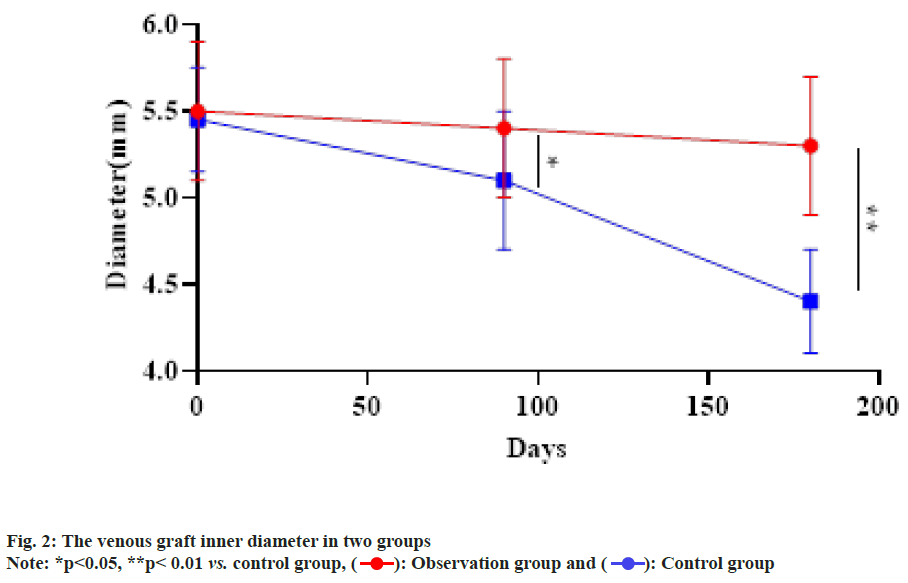
 : Observation group and
: Observation group and  : Control group
: Control group