- *Corresponding Author:
- X. Li
Department of Anesthesiology
Linyi Central Hospital
Linyi 276400, China
E-mail: ysmzwhl@163.com
| This article was originally published in a special issue, “Trending Topics in Biomedical Research and Pharmaceutical Sciences” |
| Indian J Pharm Sci 2022:84(1) Spl Issue “266-269” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
This paper is to discuss the clinical efficacy for small dose of propofol and sufentanil intravenous anesthesia in endoscopic variceal ligation. 62 patients of endoscopic variceal ligation treated in our hospital from April 2013 to October 2014 are selected to be randomly divided into control group and observation group. The contrastive analysis for anesthetic effect was made after giving sufentanil+propofol to control group and small dose of sufentanil+propofol to observation group. Incidence rates of hyoxemia and hypotension in the observation group were respectively 3.23 % and 6.45 %, far less than the 38.71 % and 16.13 % in the control group. Therefore, the coincidence time of patients in the observation group was significantly short than that in the control group, showing a significant difference (p<0.05). Small dose of propofol+sufentanil applied in endoscopic variceal ligation works well and has a relatively high safety.
Keywords
Sufentanil, propofol, endoscopic variceal ligation, anesthetia
The esophageal varices is one of the most common complications among liver cirrhosis patients. Endoscopic Variceal Ligation (EVL) is an effective means to prevent and treat the esophageal varices bleeding. EVL has already been widely and clinically applied and gained ideal effect in the treatment of esophageal varices[1-3]. The selection for anesthetic techniques, drugs and dosage in the process of operative treatments would lead to grave consequences[4-7]. The application on EVL by the small dose of sufentanil and propofol has obtained a good efficacy in this study, wherein the report is presented.
The 62 objects of study are all patients of EVL treated in our hospital from April 2013 to October 2014. The Child-Pugh grading of all patients is B-C and American Society of Anesthesiologists (ASA) grading is I-II. These patients are all absence of mental illness, renal insufficiency, serious heart and lung diseases, related drug allergy history as well as sedatives and opioid dependence. The objects of study were equally divided into the control group and observation group based on the random number method, where each for 31 objects. In the control group, gender: 18 male patients and 13 female patients; average age: (46.7±2.4); ASA grading: 13 patients for I and 17 patients for II; Child-Pugh grading: 19 patients for B and 11 patients for II. In the observation group, gender: 17 male patients and 14 female patients; averaged age: (45.8±2.8); ASA grading: 14 patients for I and 16 patients for II; Child- Pugh grading: 18 patients for B and 12 patients for II. There was no significant difference in terms of gender, age, state of illness and other general information (p>0.05).
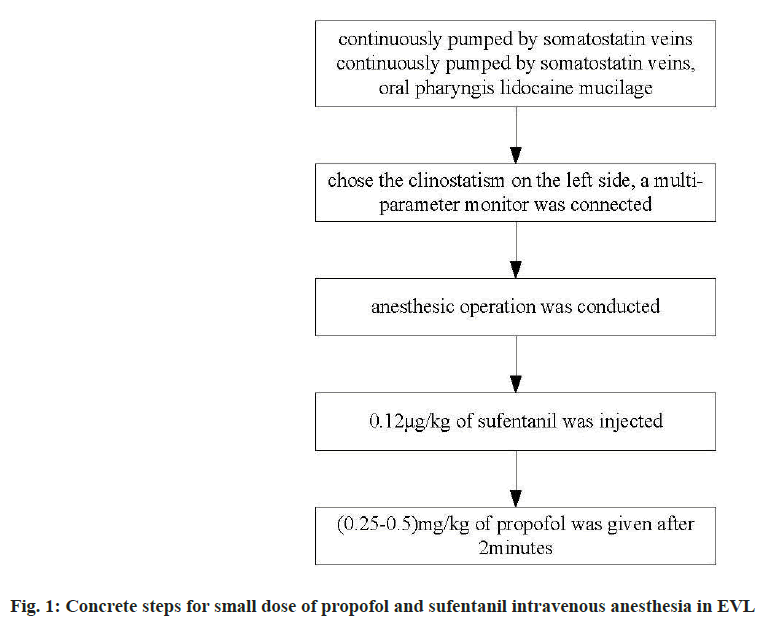
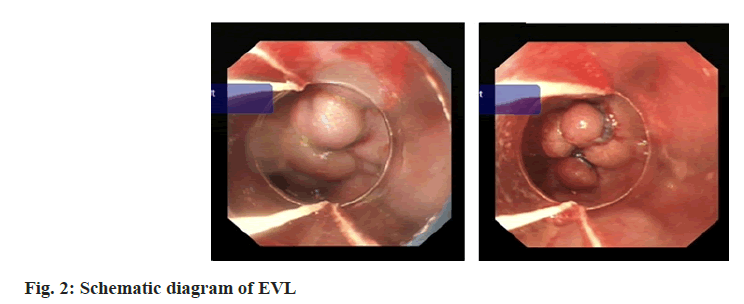
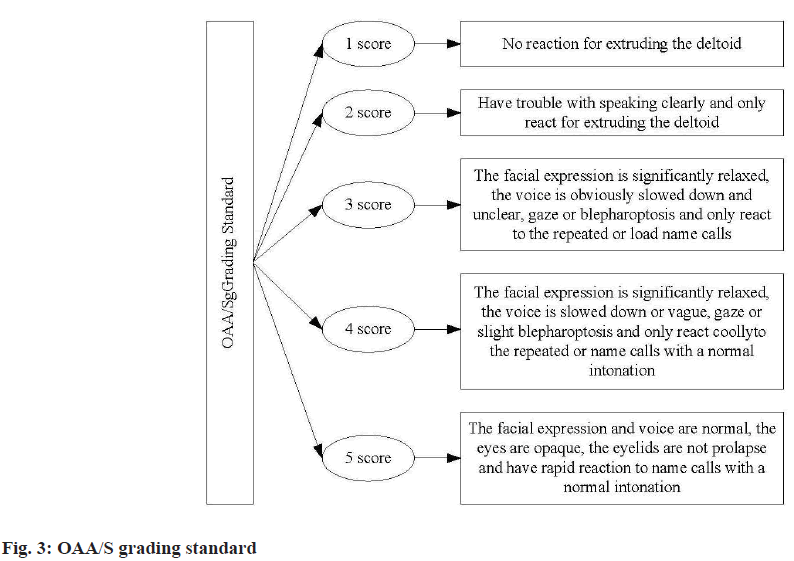
All patients were continuously pumped by somatostatin veins with fasting for 12 h before operation. In this way, the venous channels were opened for anesthesia to pars laryngea by the oral pharyngis lidocaine mucilage. The patients chose the clinostatism on the left side with conventional oxygen mask and at the same time, a multi-parameter monitor was connected for the real-time monitoring of respiratory, heart rate, blood pressure and other parameters of patients. Anesthesia procedure: The patients in the control group were injected by 1.5 μg/kg of fentanyl and propofol after 2 min, wherein the drug dose is 0.8-1.2 mg/kg and duration of the infusion should exceed 1 min. It may be deemed as the state of general anesthesia when a patient cannot react with an eyelash reflex, at which moment the operation should be carried out. The blood pressure, heart rate and saturation of pulse oximetry were closely monitored during the operation. The atropine of 0.2-0.5 mg was intravenously injected when blood pressure was lower than 80/50 mmHg; the atropine of 0.2-0.5 mg was intravenously injected when the heart rate was lower than 50/min; the assisted ventilation was carried out when oxyhemoglobin saturation was lower than 90 %. The patients in observation group were injected by 0.12 μg/kg of sufentanil and after 2 min, 0.25-0.5 mg/kg of propofol was given. The states of consciousness were closely observed and when it reached up to 3 Observer’s Assessment of Alertness/Sedation (OAA/S) grading, the stomachoscopy operation can be conducted. The concrete steps for application of small dose of propofol and sufentanil intravenous anesthesia in EVL can be seen in fig. 1. Fig. 2 is the schematic diagram of EVL.
The dosage of propofol can be gradually added based on the actual situation of patients during the operation, wherein the added dosage needs to be controlled in the scope of 10-20 mg. The OAA/S grading standard is shown as fig. 3.
The data are statistically analyzed and processed by Statistical Package for the Social Sciences (SPSS) 18.0 software, wherein the counting and measuring data are represented by Percent (%), (x̄±s) for Chi Square (χ2) and t test. p<0.05 was used to represent the obvious difference.
The incidence rates of hypotension and hyoxemia in the observation group are significantly lower than those in the control group and so does the postoperative recovery time of consciousness. There is an obvious difference (p<0.05), whose concrete details are shown in Table 1.
| Group | n | Hyoxemia | Hypotension | Vomiting reflex | Bucking in gastroscope |
|---|---|---|---|---|---|
| Control group | 31 | 12 (38.71) | 5 (16.13) | 1 (3.23) | 1 (3.23) |
| Observation group | 31 | 1 (3.23) | 2 (6.45) | 1 (3.23) | 1 (3.23) |
| χ2 | 4.621 | 2.352 | 0.00 | 0.00 | |
| p | <0.05 | <0.05 | >0.05 | >0.05 |
Table 1: Situation for Adverse Reactions of Patients in Two Groups
The postoperative recovery time of consciousness for patients in the observation group is 9.5±2.4 min, while that in the control group is 16.8±1.4 min, significantly shorter than that in the control group with a significant difference (p<0.05).
EVL is an important, effective and commonly used clinic means to treat and prevent the esophageal varices bleeding[8]. The selection for anesthetic techniques and drugs in EVL would lead to grave consequences.
Although the propofol has a short effect time when used and short postoperative recovery time of consciousness, it still has some inhibitory effects on the circulatory and respiratory system, which are closely associated with to the drug dosage[9]. The result of clinic study made by Zhang et al.[10] have shown that, using large dose of propofol for a long time would lead to the hyperlipidemia, metabolic acidosis, liver fatty infiltration and other serious complications. Although EVL gains a relatively operation time, stronger drug susceptibility may occur in the treatment process due to the poor liver function of patients. Therefore, the misuse of drugs in the treatment process may be easily exposed for obvious circulatory and respiratory inhibiting effect, which may cause serious damages to the liver function of patients[11].
As a strong opioid drug, the sufentanil has a better irritation and duration effect than fentanyl, which may have some inhibitory effects on the respiratory of patients[12]. The result of study made by Xu et al.[13] has shown that, there is a greater similarity between the effect on the circulatory system by sufentanil and fentanyl. However, higher doses may lead to the symptom of dropped heart rate and add the incidence rate of nausea, emesis and other adverse reactions. Many clinical results have suggested that, the sufentanil presents the high fat soluble and selectivity in its application process, whose analgesic potency is equal to 1000 times of morphine. Besides, it has no significant accumulation and only has small quantity of nonspecific binding in the brain tissue. For this reason, it is easily to be eliminated[14-17].
But different doses of sufentanil have different application effects, so the dosage should be reasonably selected based on physical truths. Larger doses would lead to a shorter analgesic effect time and better analgesic effect sufentanil. In this way, the incidence rate of adverse reactions would also be increased. The propofol and opioid are possessed of mutual concurrent effects, so selecting a reasonable dose of propofol and sufentanil can promote the full exertion of drug effect, reduce the drug dosage and lower the side effect of drug[18-20].
In this study, the small dose of propofol and sufentanil has gained a good anesthetic effect in the observation group, whose incidence rate of adverse reactions is significantly lower than that in the control group. Above all, small dose of propofol+sufentanil intravenous anesthesia in EVL can achieve an ideal anesthetic effect and high safety, which is worth a wide application in clinic.
Conflict of interests:
The authors declared no conflicts of interest.
References
- Liang H, Xing Z, Jin X. Analysis for optimal initial dosage of remifentanil TCI in EVI under a gastroscope. J Hainan Med Univ 2015;14(5):641-2.
- Liang H, Jin X. Application for propofol plus remifentanil TCI in EVI under a gastroscope. China Prescription Drug 2015;18(5):281-2.
- Muhammad Khyani IA, Qureshi MA, Mirza T, Umar Farooq M. Detection of interleukins-6 and 8 in saliva as potential biomarkers of oral pre-malignant lesion and oral carcinoma: A breakthrough in salivary diagnostics in Pakistan. Pak J Pharm Sci 2017;30(3):817-23.
[Google Scholar] [PubMed]
- Aroune D, Libdiri F, Leboucher S, Maouche B, Marco S, El-Aoufi S. Changes in the NFκB and E-cadherin expression are associated to diabetic nephropathy in Psammomys obesus. Saudi J Biol Sci 2017;24(4):843-50.
[Crossref] [Google Scholar] [PubMed]
- Ren Y, Jiao X, Zhang L. Expression level of fibroblast growth factor 5 (FGF5) in the peripheral blood of primary hypertension and its clinical significance. Saudi J Biol Sci 2018;25(3):469-73.
[Crossref] [Google Scholar] [PubMed]
- Lou Y, Shi J, Guo D, Qureshi AK, Song L. Function of PD-L1 in antitumor immunity of glioma cells. Saudi J Biol Sci 2017;24(4):803-7.
[Crossref] [Google Scholar] [PubMed]
- Li W, Jia MX, Wang JH, Lu JL, Deng J, Tang JX, et al. Association of MMP9-1562C/T and MMP13-77A/G polymorphisms with non-small cell lung cancer in southern Chinese population. Biomolecules 2019;9(3):107.
[Crossref] [Google Scholar] [PubMed]
- Wu Y, Xu YG. Observation for effects of dezocine combined with propofol in EVI of liver cirrhosis. J Mod Pract Med 2014;6(6):104-5.
- Zheng ZJ, Su FX, Zhang ZM. Clinical application for EVI under a trachea cannula anesthesia endoscopic. J Nongken Med 2014;11(4):325-6.
- Zhang F, Wang GL, Xu RH. Application for propofol and etomidate in EVI under a gastroscope. J Guide China Med 2013;8(1):250-1.
- Tian LH, Chen XL, Xu ZY. Comparison for anesthetic effect of sevoflurane inhalation anesthesia and TIVA in EVI. J Pract Clin Med 2015;15(2):362-3.
- Li H. Effect and safety analysis for EVI under a gastroscope and painless gastroscope. J Mod Diagn Treatment 2015;06(1):114-5.
- Xu SP, Yu L, Qu TL. Efficacy for propofol plus remifentanil TCI in EVI under a gastroscope. Chin J Mod Drug Appl 2015;17(13):105-6.
- Li Z. Clinical observation for propofol combining with different doses of painless abortion surgery. J Public Health 2013;1(16):92-3.
- Pei PJ, Li XJ, Wang MF. Application for propofol plus remifentanil TCI in EVI under a gastroscope. Zhejiang J Trauma Surg 2014;15(2):325-6.
- Dangarembizi R, Chivandi E, Dawood S, Erlwanger K, Mazuru G, Michael M, et al. The fatty acid composition and physicochemical properties of the under utilised Cassia abbreviata seed oil. Pak J Pharm Sci 2015;28(3):1005-8.
[Google Scholar] [PubMed]
- Ruiz-Olmedo MI, González-Hernández I, Palomares-Alonso F, Franco-Perez J, Jung-Cook H. Effect of nitazoxanide on albendazole pharmacokinetics in cerebrospinal fluid and plasma in rats. Saudi Pharm J 2017;25(3):413-8.
[Crossref] [Google Scholar] [PubMed]
- Huang HG, He JX, Li KJ. Randomized controlled evaluation for the propofol plus remifentanil in gastroscope diagnosis and treatment of liver cirrhosis patients. J Mod Dig Interv 2015;3(4):168-9.
- Haidar AM, Al-Assas KM, Dawabah AA. Prevalence, distribution and intraspecific variation of Heterodera schachtii populations from semiarid environment. Saudi J Biol Sci 2016;23(2):293-9.
- Jose J, Al-Tamimi FA, Helal MM, Jimmy B, Al Riyami Q, Al Busaidi I. Targeted study to evaluate the cardiovascular risk factor status among patients and efficacy of statins in attaining goal lipid levels in a regional hospital in Sultanate of Oman. Saudi Pharm J 2015;23(4):371-6.
[Crossref] [Google Scholar] [PubMed]