- *Corresponding Author:
- Weiqin Zhou
Department of Gynecology and Obstetrics, The First Affiliated Hospital of Soochow University, Suzhou, Jiangsu Province 215000, China
E-mail: zhouweiqin@suda.edu.cn
| This article was originally published in a special issue, “Drug Discovery and Repositioning Studies in Biopharmaceutical Sciences” |
| Indian J Pharm Sci 2024:86(4) Spl Issue “18-26” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
Endometriosis, which affects 10 %-15 % of women, complicates infertility diagnosis and treatment. Laparoscopy is essential for diagnosing and treating endometriotic lesions and related disorders. Post-laparoscopy natural pregnancy rates inform endometriosis-related infertility treatment options. Understanding laparoscopy’s efficacy in different endometriosis phases is crucial for enhancing reproductive outcomes and directing care options, despite research shortages. This study evaluates spontaneous pregnancy rates post-laparoscopy to help understand and treat endometriosis-related infertility. This study assesses the success rate of unintentional pregnancies in women who have had laparoscopy for infertility and endometriosis. We selected infertile women who had laparoscopies at our University Hospital from medical records from November 2021 to October 2023. Age 22 to 35, 24 mo of infertility despite unprotected intercourse, regular menstrual cycles (28 d-37 d), surgically confirmed endometriosis, normal fallopian tube function, and no recent ovulatory medication therapy, assisted reproductive technologies or hormone therapy post-surgery were the eligibility laparoscopies under general anesthesia were review board-approved and informed consent. Endometriosis patient’s reproductive outcomes after laparoscopic surgery are examined in this study. Age, initial infertility rates, body mass index, and infertility duration vary between pregnant and non-pregnant patients. The 1 y cumulative intrauterine pregnancy rate after laparoscopy rises to 50 %, suggesting surgical benefits. Laparoscopic findings and procedures vary between pregnant and non-pregnant patients, making endometriosis-related infertility management complicated. Laparoscopy’s effectiveness and endometriosis infertility treatment decisions are informed by this research. This study provides important information for both patients and physicians since it shows that infertile women with endometriosis can conceive naturally 50 % of the time 1 y after laser surgery.
Keywords
Endometriosis, laparoscopy, infertile, menstrual cycle
Endometriosis, a prevalent gynecological ailment, manifests as the presence of endometrial tissue beyond the confines of the uterus, affecting around 10 % to 15 % of women before menopause. Its precise origin remains elusive, though several theories attempt to elucidate its genesis. Among these, retrograde menstruation, where endometrial cells flow backwards through fallopian tubes and implant in the pelvic cavity, stands as the primary accepted theory. Other hypotheses include mesothelium metaplasia, in situ development of Mullerian remnants, and potential genetic or immunological influences. As an estrogen-dependent condition, endometriosis manifests with pelvic pain and infertility. It’s crucial to acknowledge the complexity of endometriosis, underscoring the need for further extensive research to unravel its intricate pathogenesis[1-3].
Endometriosis, strongly linked to infertility, impacts approximately 30 % to 50 % of affected women. Its influence on fertility is multifaceted, involving mechanisms like inflammation, progesterone resistance, altered oocyte release, and impaired transport of sperm and embryos, alongside disrupted ovarian function. These factors contribute to compromised oocyte quality, impaired fertilization, and challenges in successful implantation, resulting in diminished pregnancy rates. While surgical and assisted reproductive interventions, such as In Vitro Fertilization (IVF), show promise in enhancing pregnancy rates for women with endometriosis, the decision to pursue these treatments hinges on various factors like symptoms, ultrasound findings, ovarian reserve, and patient preferences. However, comprehending the intricate mechanisms and developing effective treatments for endometriosisrelated infertility warrants further exploration and research efforts[4-9].
Diagnosing infertility linked to endometriosis poses intricate challenges due to its multifaceted nature. The disease manifests diversely across subtypes and presentations, complicating identification. Moreover, symptoms like pelvic pain and menstrual irregularities often mirror other conditions, blurring the line for discerning infertility causes. The gold standard for diagnosis-laparoscopy-poses invasiveness and isn’t universally suitable. Compounded by the absence of specific biomarkers or definitive imaging methods, diagnosing endometriosis-related infertility demands a comprehensive approach, amalgamating medical history, physical scrutiny, imaging modalities, and occasionally surgical exploration for conclusive assessment[10-15].
Laparoscopy stands as a pivotal tool in both diagnosing and addressing endometriosis-related concerns. By providing a direct visual inspection of endometrial implants and associated abnormalities, it serves as the gold standard for diagnosis, offering clarity in observing pelvic structures. Surgeons can precisely identify and remove visible endometriotic areas and address adhesions, reinstating pelvic anatomy and potentially enhancing fertility. Research highlights that laparoscopic excision of visually detected endometriosis significantly alleviates pelvic discomfort and boosts patient contentment. However, the procedure’s efficacy heavily relies on the expertise of skilled surgeons, ensuring accurate diagnosis and optimal therapeutic outcomes[16-21].
Evaluating the rate of natural pregnancy postlaparoscopy in patients diagnosed with infertility due to endometriosis aims to gauge the efficacy of this surgical intervention in enhancing fertility. Endometriosis significantly impacts fertility, and laparoscopy offers a means to address this by identifying and removing endometriotic lesions while rectifying associated pelvic irregularities. Assessing the rate of spontaneous pregnancies post-laparoscopy provides crucial insights into the procedure’s success in enabling conception without resorting to Assisted Reproductive Technologies (ART). This data serves as a valuable guide for healthcare providers, aiding in informed treatment decisions for managing infertility stemming from endometriosis[22-27].
Laparoscopy plays a pivotal role in both diagnosing and addressing infertility by identifying and rectifying underlying issues like endometriosis, adhesions, and tubal factors that may hinder fertility. Evidence indicates its potential to facilitate natural conceptions and live births in a significant proportion of infertility cases. However, comprehensive studies examining laparoscopy’s efficacy across diverse patient groups and comparing it with alternative treatments are crucial. Such research endeavors would offer more robust insights, guiding clinicians in making informed decisions when managing infertility, thereby enhancing patient care[22,24,28].
Presently, gaps exist in comprehending the fertility outcomes after laparoscopic surgery for endometriosisrelated infertility. Crucially, the absence of specific randomized controlled trials tailored to assess postsurgical fertility in advanced endometriosis patients underscores a significant knowledge void. Moreover, limitations in the predictive capability of the revised American Fertility Society (r-AFS) classification for fertility outcomes post-surgery emphasize the necessity for more effective prognostic tools like the Endometriosis Fertility Index (EFI). Debate persists regarding the effectiveness of laparoscopic surgery in early-stage endometriosis cases, despite established improvements in fertility rates for minimal and mild endometriosis. Additionally, there’s a pressing need for research exploring optimal management strategies across different endometriosis stages and comparing treatment modalities’ outcomes, from surgery to expectant or medical therapies. Addressing these gaps through further investigation is imperative for enhancing our insights into fertility outcomes following laparoscopy for endometriosisrelated infertility[29-32].
The primary aim of this assessment is to evaluate the rate of spontaneous pregnancies in individuals diagnosed with infertility attributed to endometriosis post-laparoscopy. This study seeks to contribute essential insights into the understanding and management of infertility specifically associated with endometriosis, shedding light on the effectiveness of laparoscopic surgery as a potential treatment option for improving natural pregnancy rates in these individuals.
Materials and Methods
Research design:
The retrospective study was conducted on 550 patients who were presented with infertility and later diagnosed with endometriosis and the data was obtained by examining medical records from the hospital. The patients were infertile women who had undergone surgical laparoscopy in our hospital. The participants from the prior study were also examined closely and excluded if they did not meet the criteria. The recruitment process had the following eligibility criteria. Participants must meet the following criteria; age between 22 y and 35 y, experiencing infertility for at least 12 mo despite unprotected intercourse, having regular menstrual cycles lasting between 28 d and 37 d, diagnosed with endometriosis based on surgical and histological evidence, absence of other infertility factors and confirmed normal fallopian tube function as determined by hysterosalpingography, and no use of ovulatory drug therapy, ART or hormone therapy within 1 y after surgery. This investigation was authorized by the review board for human research at our University Hospital, and signed informed consent was obtained from each woman. Surgical procedures known as laparoscopies were conducted while the patient was under the influence of general anesthesia. The illness stage was assessed using the rAFS classification of the American Society for Reproductive Medicine (ASRM). The laparoscopic surgical procedure entailed the eradication or extraction of all observable endometriotic implants and the dissolution of adhesions.
Inclusion and exclusion criteria:
Inclusion criteria: Patients who presented with infertility and later diagnosed as endometriosis; patients who are between the ages of 22 y to 35 y old; participants must have been infertile for 12 mo despite unprotected sexual activity; women with a regular menstrual cycle 28 d-37 d, and surgical and histological diagnosis of endometriosis were included in this study.
Exclusion criteria: Women without infertility for 24 mo despite unprotected sexual activity; intermittent menstrual periods outside 28 d-37 d and no surgical or histological evidence of endometriosis were excluded from this study.
Statistical analysis:
A pregnancy that was detected within the uterus occurred within a year following the laparoscopy. In a study comparing pregnant and non-pregnant women, age, Body Mass Index (BMI), length of infertility, CA-125 levels, endometriosis stage, laparoscopic results, and surgical type were compared. All data analyses were done in Statistical Package for the Social Sciences (SPSS) 12.0 (Chicago, Illinois, United States of America (USA)). Fisher’s exact and Mann-Whitney U tests were used as needed. The significance criterion for all analyses was p<0.05.
Results and Discussion
Patient characteristics of pregnant (n=226) and nonpregnant (n=324) persons are compared in the Table 1. The average age of pregnant patients is 29.9 y, which is lower than the average age of non-pregnant patients, which is 33.1 y. The rates of primary infertility are comparable in both groups. Pregnant individuals exhibit a somewhat elevated BMI (21.9 kg/m2) compared to non-pregnant individuals (21.0 kg/m2). Pregnant patients have a shorter period of infertility, with an average of 31.9 mo, compared to non-pregnant patients who have an average length of 42.9 mo. In pregnant women, CA-125 levels are elevated at 36.9 μ/ml, compared to non-pregnant patients who have levels of 22.0 u/ml. In addition, this study has found a significant p<0.03 of CA-125 levels among pregnant and non-pregnant patients. The prevalence of rAFS stages varies, with stages I-II being more frequent in pregnant individuals and stages III-IV being more prevalent in non-pregnant individuals.
| Patient characteristics | Pregnant patients (n=226) | Non-pregnant patients (n=324) | p |
|---|---|---|---|
| Age (y) | 29.9±3.4 | 33.1±4.0 | 0.06 |
| Primary infertility (%) | 152 (67.25 %) | 210 (64.81) | 0.06 |
| BMI (kg/m2) | 21.9±2.4 | 21.0±2.3 | 0.07 |
| Duration of infertility (mo) | 31.9±13.9 | 42.9±32.0 | 0.08 |
| CA-125 (µ/ml) | 36.9±42.9 | 22.0±16.1 | 0.03 |
| rAFS stage | |||
| I-II | 100 (44.24 %) | 180 (55.55 %) | 0.07 |
| III-IV | 126 (55.75 %) | 144 (44.44 %) | |
Table 1: Patient Characteristics in Pregnant and Non-Pregnant Patients
In Table 2, the distribution of patients across different rAFS stages is presented. Among the total 550 patients, the majority were classified into stage III, constituting 66.66 % (200 patients). Stage II follows with 150 patients (60.00 %), while stage I and stage IV have 100 patients each, representing 40.00 % and 33.33 % of the total, respectively. The overall percentage distribution indicates that stage III has the highest proportion among the rAFS stages, contributing to 54.55 % of the entire patient population. This table provides a concise overview of the distribution of patients based on their rAFS stage, offering insights into the prevalence of different stages within the studied population.
| rAFS Stage | Patients | Total |
|---|---|---|
| I | 100 (40.00 %) | 250 (45.46 %) |
| II | 150 (60.00 %) | |
| III | 200 (66.66 %) | 300 (54.55 %) |
| IV | 100 (33.33 %) | |
| Total | 550 (100 %) | |
Table 2: Number of Patients in each rAFS Stage
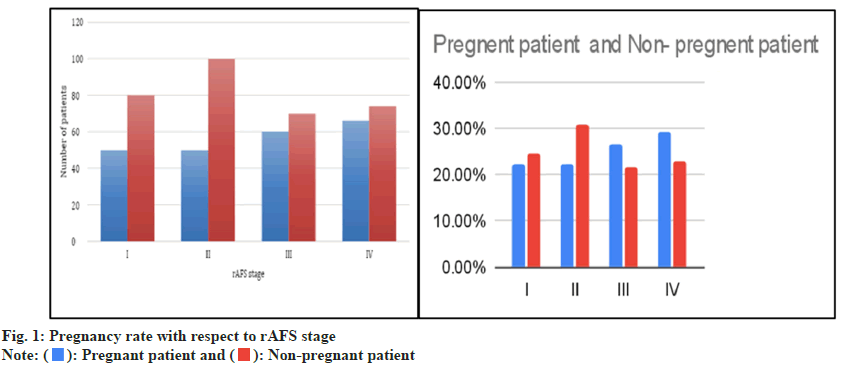
Fig. 1 depicts the pregnancy rate in relation to the rAFS stage among two groups of patients: Those who are pregnant (n=226) and those who are not pregnant (n=324). The patient distribution among the four rAFS phases is as follows; stage I has a prevalence of 22.12 % in pregnant individuals and 24.69 % in non-pregnant individuals. Stage II has a prevalence of 22.12 % in pregnant individuals and 30.86 % in non-pregnant individuals. Stage III has a prevalence of 26.54 % in pregnant individuals and 21.60 % in non-pregnant individuals. Stage IV has a prevalence of 29.20 % in pregnant individuals and 22.83 % in non-pregnant individuals. The data shown in the picture indicates that pregnancy rates change across different stages, hence emphasizing potential correlations between the severity of endometriosis (rAFS stage) and the outcomes of pregnancy.
Table 3 displays laparoscopic observations in a group of 226 pregnant patients and 324 non-pregnant patients. Endometriomas are present in 15.43 % of pregnant individuals and 18.51 % of non-pregnant individuals. Small endometriomas are more common in both groups. There are also reported incidences that affect both sides. The prevalence of peritubal/ subovarian adhesions is higher in non-pregnant patients (44.44 %) compared to pregnant patients (33.62 %). Posterior cul-de-sac obliteration is observed in 26.31 % of pregnant individuals and 25.00 % of non-pregnant individuals. The degree of obliteration varies, with lesions being categorized as partial, total or superficial. These findings offer valuable understanding of the laparoscopic features of endometriosis in both pregnant and non-pregnant populations.
| Laparoscopic finding | Pregnant patients (n=226) | Non-pregnant patients (n=324) | p |
|---|---|---|---|
| Endometrioma | 50 (15.43 %) | 60 (18.51 %) | 0.06 |
| Unilateral | 50 (15.43 %) | 60 (18.51 %) | 0.08 |
| Small | 30 (60.00 %) | 45 (75.00 %) | 0.07 |
| Large | 20 (40.00 %) | 15 (25.00 %) | 0.07 |
| Bilateral | 50 (15.43 %) | 60 (18.51 %) | 0.11 |
| Small Endometrioma | 30 (60.00 %) | 50 (83.33 %) | 0.06 |
| Large Endometrioma | 20 (40.00 %) | 10 (16.66 %) | 0.07 |
| Peritubal/subovarian adhesion | 76 (33.62 %) | 144 (44.44 %) | 0.09 |
| Posterior cul-de-sac obliteration | 20 (26.31 %) | 36 (25.00 %) | 0.11 |
| Partial | 16 (21.05 %) | 40 (27.77 %) | 0.07 |
| Complete | 20 (26.31 %) | 32 (22.22 %) | 0.08 |
| Superficial lesion only | 20 (26.31 %) | 36 (25.00 %) | 0.07 |
Table 3: Laparoscopic Findings in Pregnant and Non-Pregnant Patients
Table 4 presents the laparoscopic observations in a group of 226 pregnant patients and 324 nonpregnant patients. The predominant procedures in both categories are fulguration, with a prevalence of 30.97 % in pregnant individuals and 31.17 % in non-pregnant individuals, and endometrioma enucleation, with a prevalence of 22.12 % in pregnant individuals and 21.60 % in non-pregnant individuals. Fenestration and fulguration are carried out in 17.69 % of pregnant patients and 18.51 % of non-pregnant instances. In addition, the significant p value was 0.04 among pregnant and non-pregnant patients. The occurrence of unilateral salpingo-oophorectomy is higher in pregnant individuals (13.27 %) compared to non-pregnant patients (9.87 %). The procedure of adhesiolysis is carried out in 8.84 % of pregnant cases and 9.87 % of non-pregnant cases, whereas myomectomy is performed in 7.07 % of pregnant instances and 8.95 % of non-pregnant cases and p value was 0.04.
| Laparoscopic finding | Pregnant patients (n=226) | Non-pregnant patients (n=324) | p |
|---|---|---|---|
| Fulguration | 70 (30.97 %) | 101 (31.17 %) | 0.04 |
| Endometrioma enucleation | 50 (22.12 %) | 70 (21.60 %) | 0.07 |
| Fenestration and fulguration | 40 (17.69 %) | 60 (18.51 %) | 0.08 |
| Unilateral salpingo-oophorectomy | 30 (13.27 %) | 32 (9.87 %) | 0.09 |
| Adhesiolysis | 20 (8.84 %) | 32 (9.87 %) | 0.08 |
| Myomectomy | 16 (7.07 %) | 29 (8.95 %) | 0.04 |
Table 4: Laparoscopic Procedure in Pregnant and Non-Pregnant Patients
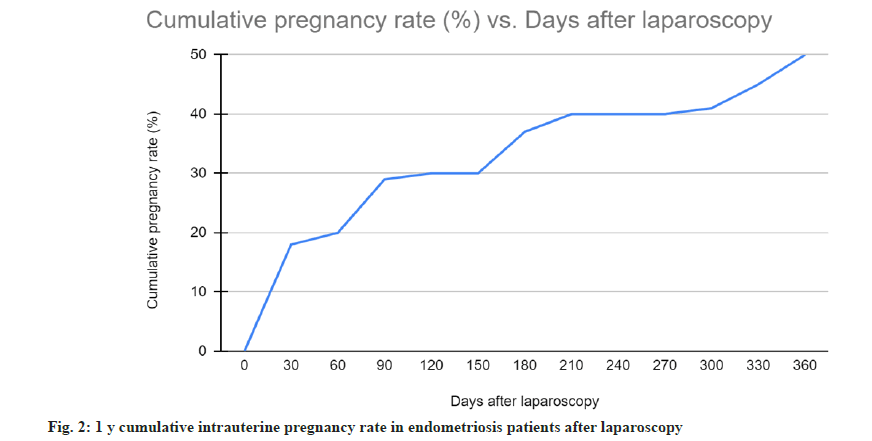
The cumulative intrauterine pregnancy rate in endometriosis patients following laparoscopy follows the guidelines shown in fig. 2. There is a clear upward trend in the cumulative pregnancy rate as seen in the graph. A rate of 0 % is seen at the outset (0 d following laparoscopy), which increases to 18 % at 30 d and 30 % at 120 d. At 360 d after laparoscopy, the trend continues to rise, reaching 50 %. This provides more evidence that laparoscopy may enhance reproductive outcomes for endometriosis patients, since intrauterine pregnancy rates seem to have improved gradually over the year after surgery.
In a study by Pantou et al.[22] which delved into the efficacy of laparoscopic surgery as a diagnostic and therapeutic measure for infertility among women with undetermined causes despite standard investigations and multiple failed IVF attempts. Out of the 107 eligible women, laparoscopic intervention revealed endometriosis in 62 patients (57.94 %), pelvic adhesions in 25 patients (23.3 %), and unexplained infertility in 20 cases (18.69 %). Following corrective procedures for endometriosis and adhesions, patients were encouraged to conceive naturally, while those with unexplained infertility underwent a single IVF cycle. Within the 1st y after laparoscopy, 48.38 % of those with diagnosed endometriosis achieved natural conception, resulting in live births for 93.4 % of them. Similarly, 44 % of patients with adhesions attained natural conception. However, among those with unexplained infertility, only 20 % achieved clinical pregnancy after the first IVF cycle. These findings underscore laparoscopy’s promising role in diagnosing and addressing infertility, notably through revealing pertinent diagnostic details, offering a valuable alternative to excessive reliance on IVF for patients with undetermined infertility issues and recurrent IVF failures.
In a study by Porpora et al.[33] 47 infertile women underwent laparoscopic treatment for endometriosis. The distribution of endometriosis stages among the patients was 11 % for stage I, 11 % for stage II, 53.3 % for stage III, and 24.4 % for stage IV. Over an average follow-up of 48.5+/-18.44 mo, the overall pregnancy rate reached 64.4 %. The majority, 69 % (18 out of 26 women), conceived within 6 mo postlaparoscopy, with 23 % conceiving at 12 mo, 11 % within 24 mo, and another 11 % after 2 y (p<0.01). In addition, this study has found a significant p<0.03 of CA-125 levels among pregnant and nonpregnant patients. Adhesions in the adnexa and tubal conditions notably influenced pregnancy rates. However, no significant differences were observed concerning the disease stage or the presence of ovarian endometrioses. These findings highlight that laparoscopic treatment significantly improves fertility, particularly within the initial 6 mo following surgery, where adnexal adhesions and tubal status play key roles in determining reproductive outcomes.
In a retrospective study by Centini et al.[34] at an endometriosis tertiary center, 115 patients who underwent laparoscopic surgery for deep endometriosis-related infertility were assessed. Analysis of fertility outcomes post-surgery correlated pregnancy rates with lesion characteristics; number, size, and location (anterior, posterolateral, pouch of Douglas, or multiple locations). Over an average follow-up of 22 mo, the overall pregnancy rate was 54.78 % (n=63), resulting in a live birth rate of 42.6 % (n=49). Of the patients with the opportunity for spontaneous conception (n=70), the overall pregnancy rate was 60 % (n=42), with 38.5 % (n=27) conceived spontaneously and 21.4 % (n=15) via Assisted Reproductive Technology (ART). Removal of multiple lesions correlated with higher post-surgery pregnancy rates. Interestingly, isolated lesion size and disease location didn’t significantly affect the pregnancy rate, whereas patients receiving their first surgical treatment for multiple lesions exhibited higher pregnancy rates (odds ratio, 4.18). This study highlights that laparoscopic excision of deep endometriosis significantly enhances pregnancy rates, emphasizing the impact of initial surgical intervention on multiple lesions for improved fertility outcomes.
A prospective cohort study by Bianchi et al.[35] involved 179 infertile women under 38 y exhibiting symptoms or signs of Deep Infiltrative Endometriosis (DIE) in Sao Paulo, Brazil. They were divided into two groups; group A (IVF only, n=105) and group B (extensive laparoscopic DIE excision before IVF, n=64). Out of these, 10 were lost to follow-up. Group B underwent laparoscopic excision of approximately 5±2 DIE lesions. In addition, the significant p value was 0.04 among pregnant and non-pregnant patients.
The patient characteristics between groups were similar in terms of age, infertility duration and d 3 serum follicle-stimulating hormone levels. However, group B had more previous IVF attempts. IVF outcomes differed notably between the groups; the total dose of recombinant follicle-stimulating hormone required for ovulation induction was slightly higher in group B (2542 IU) compared to group A (2380 IU), and the number of oocytes retrieved was slightly lower in group B (9) compared to group A (10). Despite these differences, the pregnancy rate after IVF was significantly higher in group B (41 %) than in group A (24 %). Importantly, the odds of achieving pregnancy were 2.45 times greater in the extensive laparoscopic excision group (B) than in the IVF-only group (A).
Pregnancy rates post-laparoscopy are influenced by multiple variables. The presence of tubal adhesions may diminish cumulative pregnancy rates, contrasting with cases lacking adhesions. Severity levels of endometriosis significantly impact these rates. Factors such as younger age, superior ovarian reserve, and enhanced sperm parameters are linked to increased pregnancy probabilities. Tubal status, endometriosis severity, age, ovarian reserve, and sperm quality collectively play roles in determining post-laparoscopy pregnancy outcomes[36,37].
Research demonstrates that laparoscopic surgery effectively boosts natural pregnancy rates in women grappling with endometriosis-related infertility, particularly within the initial 6 mo post-surgery. Adnexal adhesions and tubal conditions significantly influence reproductive outcomes, while disease stage and ovarian endometriomas seem less impactful. These findings advocate for laparoscopy as a viable therapeutic avenue for individuals with minimal to moderate endometriosis-related infertility, facilitating the removal of visible endometriotic areas, pelvic restoration and improved fertility. Clinically, this underscores the importance of counselling patients, emphasizing the optimal pregnancy window post-surgery and the significance of pre-surgical assessment for adhesions and tubal conditions. Laparoscopy emerges as a valuable tool in managing endometriosis-related infertility, yet tailored considerations for each patient’s unique characteristics are pivotal in treatment decisions[33,38,39].
The existing literature highlights potential areas for further exploration regarding laparoscopic treatment in endometriosis-related infertility. Studies often exhibit limited long-term follow-up, necessitating comprehensive research to gauge sustained pregnancy rates post-surgery. Understanding how different stages and locations of endometriosis affect natural pregnancy rates after laparoscopy is crucial for tailored treatment approaches. Investigating the impact of adjuvant therapies combined with surgery on fertility outcomes is a pertinent avenue for future research. Developing predictive models considering patient-specific factors like age and severity of endometriosis is pivotal for informed patient selection. Moreover, assessing the surgery’s impact on patients’ overall quality of life beyond just achieving pregnancy would offer a more comprehensive perspective. In summary, addressing these aspectslong- term follow-up, diverse endometriosis types, adjuvant therapies, patient selection, and quality of life-remains essential for advancing understanding and optimizing treatment strategies[23-26,33,34,37,40].
This study concluded that the current study concludes that among infertile women with endometriosis alone, the natural conception rate was 50.00 % 1 y following laparoscopic surgery. With this knowledge, infertile patients who are seeking treatment for endometriosis and the physicians who are counseling them should find it helpful. There are still significant knowledge gaps about the natural conception rates following laparoscopy for infertility caused by endometriosis, while this area of research has made significant contributions. For starters, when it comes to severe endometriosis, there is a dearth of randomized controlled trials that are designed to evaluate the success of reproductive treatments after surgery. There is a need for better prognostic tools like the EFI because the r-AFS classification is not very good at predicting fertility outcomes. This study found that significantly more pregnant and non-pregnant than pregnant patients and fulguration, and myomectomy was done. We need further studies comparing surgical, expectant and medicinal treatments for endometriosis so we may better care for patients and make informed treatment decisions. Optimal management options should be the focus of this research.
Funding:
The project was supported by Suzhou University Horizontal Research Project, (Grant/Award Number: XY202110301612) and Suzhou University Horizontal Research Project, (Grant/Award Number: H230971).
Conflict of interests:
The authors declared no conflict of interests.
References
- García MM, Olartecoechea B, Royo MP, Aubá M, Lopez G. Endometriosis. Rev Med Univ Navarra 2009;53(2):4-7.
- Patel BG, Lenk EE, Lebovic DI, Shu Y, Yu J, Taylor RN. Pathogenesis of endometriosis: Interaction between endocrine and inflammatory pathways. Best Pract Res Clin Obstetr Gynaecol 2018;50:50-60.
[Crossref] [Google Scholar] [PubMed]
- Burney RO, Giudice LC. Pathogenesis and pathophysiology of endometriosis. Fertil Steril 2012;98(3):511-9.
[Crossref] [Google Scholar] [PubMed]
- Stilley JA, Birt JA, Sharpe-Timms KL. Cellular and molecular basis for endometriosis-associated infertility. Cell Tissue Res 2012;349:849-62.
[Crossref] [Google Scholar] [PubMed]
- Koch J, Rowan K, Rombauts L, Yazdani A, Chapman M, Johnson N. Endometriosis and infertility-A consensus statement from ACCEPT (Australasian CREI Consensus Expert Panel on Trial evidence). Aust N Z J Obstet Gynaecol 2012;52(6):513-22.
[Crossref] [Google Scholar] [PubMed]
- Gupta S, Goldberg JM, Aziz N, Goldberg E, Krajcir N, Agarwal A. Pathogenic mechanisms in endometriosis-associated infertility. Fertil Steril 2008;90(2):247-57.
[Crossref] [Google Scholar] [PubMed]
- Carvalho LF, Rossener R, Azeem A, Malvezzi H, Simoes Abrao M, Agarwal A. From conception to birth: How endometriosis affects the development of each stage of reproductive life. Minerva Ginecol 2013;65(2):181-98.
[Google Scholar] [PubMed]
- Cecchino GN, Cozzolino M, Roque M, García-Velasco JA. Endometrioma and reproductive issues: A well-informed patient may be the driver for change. Minerva Ginecol 2020;72(3):149-56.
[Crossref] [Google Scholar] [PubMed]
- Corachán A, Pellicer N, Pellicer A, Ferrero H. Novel therapeutic targets to improve IVF outcomes in endometriosis patients: A review and future prospects. Hum Reprod Update 2021;27(5):923-72.
[Crossref] [Google Scholar] [PubMed]
- Pascoal E, Wessels JM, Aas-Eng MK, Abrao MS, Condous G, Jurkovic D, et al. Strengths and limitations of diagnostic tools for endometriosis and relevance in diagnostic test accuracy research. Ultrasound Obstet Gynecol 2022;60(3):309-27.
[Crossref] [Google Scholar] [PubMed]
- Bulletti C, Coccia ME, Battistoni S, Borini A. Endometriosis and infertility. J Assist Reprod Genet 2010;27:441-7.
- Whitehill K, Yong PJ, Williams C. Clinical predictors of endometriosis in the infertility population: Is there a better way to determine who needs a laparoscopy? J Obstetr Gynaecol Canada 2012;34(6):552-7.
[Crossref] [Google Scholar] [PubMed]
- Bonavina G, Taylor HS. Endometriosis-associated infertility: From pathophysiology to tailored treatment. Front Endocrinol 2022;13:1020827.
[Crossref] [Google Scholar] [PubMed]
- Gianetto-Berrutti A, Feyles V. Endometriosis related to infertility. Minerva Ginecol 2003;55(5):407-16.
- Macer ML, Taylor HS. Endometriosis and infertility. Obstetr Gynecol Clin North Am 2012;39(4):535-49.
- Nawrocka-Rutkowska J, Szydlowska I, RylA, Ciecwiez S, Ptak M, Starczewski A. Evaluation of the diagnostic accuracy of the interview and physical examination in the diagnosis of endometriosis as the cause of chronic pelvic pain. Int J Environ Res Public Health 2021;18(12):6606.
[Crossref] [Google Scholar] [PubMed]
- Perper MM, Nezhat F, Goldstein H, Nezhat CH, Nezhat C. Dysmenorrhea is related to the number of implants in endometriosis patients. Fertility Sterility 1995;63(3):500-3.
[Crossref] [Google Scholar] [PubMed]
- Sananes S, Canis M, Levardon M, Dubuisson JB, Donnez J. Role of gonadotrophin-releasing hormone agonists in the treatment of external genital endometriosis: Review of 77 cases. Clin Ther 1992;14:17-28.
[Google Scholar] [PubMed]
- Gratton SM, Choudhry AJ, Vilos GA, Vilos A, Baier K, Holubeshen S, et al. Diagnosis of endometriosis at laparoscopy: A validation study comparing surgeon visualization with histologic findings. J Obstetr Gynaecol Canada 2022;44(2):135-41.
[Crossref] [Google Scholar] [PubMed]
- Jacobson TZ, Duffy JM, Barlow DH, Farquhar C, Koninckx PR, Olive D. Laparoscopic surgery for subfertility associated with endometriosis. Cochrane Database Syst Rev 2010;1:CD001398.
[Crossref] [Google Scholar] [PubMed]
- Wykes CB, Clark TJ, Chakravati S, Mann CH, Gupta JK. Efficacy of laparoscopic excision of visually diagnosed peritoneal endometriosis in the treatment of chronic pelvic pain. Eur J Obstetr Gynecol Reprod Biol 2006;125(1):129-33.
[Crossref] [Google Scholar] [PubMed]
- Pantou A, Simopoulou M, Sfakianoudis K, Giannelou P, Rapani A, Maziotis E, et al. The role of laparoscopic investigation in enabling natural conception and avoiding in vitro fertilization overuse for infertile patients of unidentified aetiology and recurrent implantation failure following in vitro fertilization. J Clin Med 2019;8(4):548.
[Crossref] [Google Scholar] [PubMed]
- Lin JF, Sun CX, Hua KQ, Xue XH, Li Y. Clinical study of effect of laparoscopic diagnosis and treatment on pelvic endometriosis-associated infertility. Zhonghua Fu Chan Ke Za Zhi 2005;40(1):9-12.
[Google Scholar] [PubMed]
- Mahran A, Abdelraheim AR, Eissa A, Gadelrab M. Does laparoscopy still has a role in modern fertility practice? Int J Reproduct Biomed 2017;15(12):787-94.
[Google Scholar] [PubMed]
- Fuchs F, Raynal P, Salama S, Guillot E, Le Tohic A, Chis C, et al. Fertility after laparoscopic surgery for pelvic endometriosis in patients with unsuccessful pregnancy. J Gynecol Obstetr Reproduct Biol 2007;36(4):354-9.
- Lee HJ, Lee JE, Ku SY, Kim SH, Kim JG, Moon SY, et al. Natural conception rate following laparoscopic surgery in infertile women with endometriosis. Clin Exp Reprod Med 2013;40(1):29.
[Crossref] [Google Scholar] [PubMed]
- Jin X, Beguerie JR. Laparoscopic surgery for subfertility related to endometriosis: A meta-analysis. Taiwan J Obstetr Gynecol 2014;53(3):303-8.
[Crossref] [Google Scholar] [PubMed]
- Hassa H, Aydin Y. The role of laparoscopy in the management of infertility. J Obstetr Gynaecol 2014;34(1):1-7.
[Crossref] [Google Scholar] [PubMed]
- Spencer S, Lazaridis A, Grammatis A, Hirsch M. The treatment of endometriosis-associated infertility. Curr Opinion Obstetr Gynecol 2022;34(5):300-14.
- Demir E, Soyman Z, Kelekci S. Outcomes between non-IVF and IVF treatment after laparoscopic conservative surgery of advanced endometriosis with endometriosis fertility index score >3. Medicine 2022;101(37):e30602.
[Crossref] [Google Scholar] [PubMed]
- Boujenah J, Cedrin-Durnerin I, Herbemont C, Bricou A, Sifer C, Poncelet C. Use of the endometriosis fertility index in daily practice: A prospective evaluation. Eur J Obstetr Gynecol Reprod Biol 2017;219:28-34.
[Crossref] [Google Scholar] [PubMed]
- Buyalos RP, Agarwal SK. Endometriosis-associated infertility. Curr Opinion Obstetr Gynecol 2000;12(5):377-81.
[Crossref] [Google Scholar] [PubMed]
- Porpora MG, Pultrone DC, Bellavia M, Franco C, Crobu M, Cosmi EV. Reproductive outcome after laparoscopic treatment of endometriosis. Clin Exp Obstetr Gynecol 2002;29(4):271-3.
[Crossref] [Google Scholar] [PubMed]
- Centini G, Afors K, Murtada R, Argay IM, Lazzeri L, Akladios CY, et al. Impact of laparoscopic surgical management of deep endometriosis on pregnancy rate. J Minimally Invasive Gynecol 2016;23(1):113-9.
[Crossref] [Google Scholar] [PubMed]
- Bianchi PH, Pereira RM, Zanatta A, Alegretti JR, Motta EL, Serafini PC. Extensive excision of deep infiltrative endometriosis before in vitro fertilization significantly improves pregnancy rates. J Minimally Invasive Gynecol 2009;16(2):174-80.
[Crossref] [Google Scholar] [PubMed]
- Maruyama M, Osuga Y, Momoeda M, Yano T, Tsutsumi O, Taketani Y. Pregnancy rates after laparoscopic treatment. Differences related to tubal status and presence of endometriosis. J Reprod Med 2000;45(2):89-93.
[Google Scholar] [PubMed]
- Wdowiak A, Wdowiak E, Stec M, Bojar I. Post-laparoscopy predictive factors of achieving pregnancy in patients treated for infertility. Wideochir Inne Tech Maloinwazyjne 2016;11(4):253-8.
[Crossref] [Google Scholar] [PubMed]
- Duffy JM, Arambage K, Correa FJ, Olive D, Farquhar C, Garry R, et al. Laparoscopic surgery for endometriosis. Cochrane Database Syst Rev 2014;4:CD011031.
[Crossref] [Google Scholar] [PubMed]
- Osuga Y, Koga K, Tsutsumi O, Yano T, Maruyama M, Kugu K, et al. Role of laparoscopy in the treatment of endometriosis-associated infertility. Gynecol Obstetr Invest 2002;53(1):33-9.
[Crossref] [Google Scholar] [PubMed]
- Karabacak O, Kambic R, Gursoy R, Ozeren S. Does ovulation induction affect the pregnancy rate after laparoscopic treatment of endometriosis? Int J Fertil Womens Med 1999;44(1):38-42.
[Google Scholar] [PubMed]