- *Corresponding Author:
- Xuejing Pang
Department of Dentistry, Kunming Children’s Hospital, Kunming, Yunnan 650228, China
E-mail: pxj2012@126.com
| This article was originally published in a special issue, “Emerging Therapeutic Interventions of Biopharmaceutical Sciences” |
| Indian J Pharm Sci 2024:86(3) Spl Issue “115-121” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
This report intends to study the efficacy of curcumin and alcohol-containing mouthwashes in the treatment of chronic periodontal disease. 114 chronic periodontal disease patients, admitted between November 2018 and November 2022 were considered and all the patients received basic treatment for chronic periodontal disease. On this basis, research group (n=59) was treated with curcumin and alcohol-containing mouthwashes, while the control group (n=55) was treated with compound gargle solution chlorhexidine gluconate. The curative effect and adverse reactions such as discomfort, oral inflammation, and tissue edema were studied. Similarly, periodontal indices like probing depth, sulcus bleeding index, attachment loss, gingival crevicular fluid inflammation, high-sensitivity c-reactive protein, tumor necrosis factor-alpha, interleukin-8, and serum matrix metalloproteinases were compared between the two groups. The data showed an evidently higher overall response rate of treatment in the research group compared with the control group; the incidence of adverse reactions was similar in the two groups. Markedly lower post-interventional probing depth, sulcus bleeding index, attachment loss, high-sensitivity c-reactive protein, tumor necrosis factor-alpha, interleukin-8, and serum matrix metalloproteinases was observed in the research group, compared with the pre-intervention values and the control group. Conclusively, the curcumin and alcohol-containing mouthwash is effective in treating chronic periodontal disease, which can improve the periodontal indices of patients and inhibit gingival crevicular fluid inflammation.
Keywords
Curcumin, matrix metalloproteinases, tumor necrosis factor, chlorhexidine, c-reactive protein
Chronic Periodontal Disease (CPD) primarily affects tooth supporting structures such as gums, bones and periodontal ligaments and is often accompanied by various inflammatory reactions, which may trigger tooth loss and systemic inflammatory reactions[1,2]. The disease is also infectious, involving interactions between pathogenic bacteria and host immune responses, which activates the host immune system and induces the synthesis and release of cytokines, pro-inflammatory mediators and Matrix Metalloproteinases (MMPs), leading to tissue destruction[3,4]. Periodontitis is a typical representative of CPD, followed by periodontal swelling and gingivitis[5]. According to statistics, CPD as a worldwide epidemic, afflicts approximately 3.9 billion people all over the world, with the prevalence rates of mild and severe periodontitis being 35 % and 11 %, respectively[6,7].
The disease will not only lead to dietary and communication restrictions in patients, but may cause systemic diseases such as stroke, cancer, cardiovascular disease and chronic kidney disease, resulting in varying degrees of negative impact on patients’ quality of life[8-10]. Hence, the prevention and treatment of CPD is of great significance to improve the clinical outcomes and quality of life among these patients.
Curcumin, a polyphenol compound derived from the rhizome of the edible spice Curcuma longa and a widely consumed food ingredient, has medicinal value, a certain degree of safety and high bioavailability, as well as anticancer, anti-inflammatory, antioxidant, and glucose homeostasis-modulating actions[11,12]. It is known to play an anti-inflammatory role by inhibiting transcription factor, Nuclear Factor Kappa B (NF-κB) cells, and can also induce Nuclear factor erythroid 2-related factor 2 (Nrf2) axis to strengthen antioxidant defense mechanisms[13].
A rat study showed that curcumin has an outstanding inhibitory effect on innate immune responses related to periodontal disease, which is associated with the reduction of inflammatory infiltration and the increase of collagen content and fibroblast count, suggesting the high therapeutic potential of curcumin in chronic inflammatory periodontal diseases[14]. Zhang et al.[15] also reported that curcumin had a similar effect on periodontal health restoration in periodontitis treatment compared with chlorhexidine. Evidence has also demonstrated the certain antibacterial activity of curcumin against periodontal pathogens, can effectively inhibit periodontal biofilms by hindering the growth of bacterial strains, thus exerting antibacterial activity[16].
This study proposed a curcumin and alcoholcontaining mouthwash for the treatment of CPD, hoping to provide a new clinical reference for the prevention and treatment of such periodontal disease in patient population.
Materials and Methods
General information:
The Ethics Committee of Kunming Children’s Hospital has granted approval for this research, and the informed consent from the patients was obtained. Primarily, 114 CPD patients who received treatment in Kunming Children’s Hospital between November 2018 and November 2022 were selected were grouped as research group and control group, each of 59 patients. The research group was treated with curcumin and alcohol-containing mouthwashes. Similarly, 55 patients were categorized as control group, who were treated with compound gargle solution, chlorhexidine gluconate. Both the groups showed clinical comparability with no significant difference in baseline data (p>0.05).
Eligibility criteria:
The eligibility for participating in this study along with the inclusion and exclusion criteria is discussed below.
Inclusion criteria: All the patients meeting the diagnostic criteria for CPD after examination and diagnosis were considered; patients who had no symptoms such as displacement and masticatory dysfunction and patients with no contraindications to the treatment regimens of this study nor patients with the history of orthodontic treatment, previously were included in the study.
Exclusion criteria: Patients who were affected by periodontal recovery or affected by periodontal hyperplasia due to the long-term use of immunosuppressants and antibiotics; patients prone to allergies to the drugs used in this study; patients who used traditional Chinese medicinal preparation before 1 mo of enrollment of this study; patients who had poor oral habits, patients having family genetic history of maxillofacial trauma; dental deformities due to oral tumors and other causes; breast-feeding or pregnant women; patients with the history of mental illness and incomplete patient data were excluded from the study.
Treatment methods:
All the patients received basic treatment for periodontitis. They were advised to brush their teeth twice daily, morning and night. The gargle was composed of curcumin, edible alcohol, low molecular weight chitosan, sorbitol, parabens, Sodium Hydroxide (NaOH), drinking water, etc. As per the recommended dosage, all the patients were guided to use 50 ml of gargle each time for 2-3 min, twice a day. The research group was additionally treated with curcumin and alcoholcontaining mouthwashes while the control group was treated with compound gargle solution of chlorhexidine gluconate, where the patients were asked to gargle 50 ml of the gargle solution of chlorhexidine gluconate for 2-3 min, twice a day. Both the groups received the treatment for 4 w.
Detection indicators:
Both the groups were comparatively analyzed for curative effects; adverse reactions such as discomfort, oral inflammation, and tissue edema; periodontal indices such as Probing Depth (PD), Sulcus Bleeding Index (SBI), Attachment Loss (AL), Gingival Crevicular Fluid (GCF) inflammation, high-sensitivity C-Reactive Protein (hs-CRP), Tumor Necrosis Factor-Alpha, (TNF-α), Interleukin-8 (IL-8) and serum MMP-3, 8, and 13
Curative effects: The evaluation criteria of significant response included is that the inflammation subsided after treatment and the symptoms such as gum swelling and pain disappeared, with no inflammatory exudation and a <4 mm decrease in PD. A response corresponds to subsided inflammation after treatment and alleviated symptoms such as gingival swelling and pain, with no inflammatory exudation, and a <4 mm decrease in PD. Non-response means that the clinical signs and symptoms of the patients have not changed significantly or even worsened after treatment. The Overall Response Rate (ORR) of treatment was the sum of marked response rate and response rate.
Adverse reactions: Adverse reactions such as discomfort, oral inflammation and tissue edema were statistically accounted and the incidence rate was calculated. Periodontal indices considered were PD, SBI, and AL which were detected before and after treatment using a periodontal probe.
Levels of GCF inflammatory factors and serum MMPs: The absorbent paper point was inserted into the GCF for complete contact with GCF for 1 min. The absorbent paper was then taken out and placed into a centrifuge tube, followed by the addition of 0.3 ml phosphate buffer solution, thorough dissolution, and the supernatant obtained after 10 min of rotary centrifugation was considered as sample of GCF. Enzyme-Linked Immunosorbent Assay (ELISA) was then carried out to determine GCF hs-CRP, TNF-α, and IL-8 levels. On the other hand, before and after treatment, 6 ml of venous blood was taken from patients in both the groups, and the upper serum was separated by centrifugation and stored at -70° for examination. Serum MMP-3, 8, and 13 was also measured following ELISA assay.
Statistical analysis:
Statistical analysis of the data was carried out by Statistical Package of Social Sciences (SPSS) 18.0 software package at a significant level of p<0.05. Count data was represented by the number of cases, (percentage (%)) (n, %) and the quantitative data were described as Standard Deviation (SD)±Standard Error of Mean (SEM). Chi-square (χ2) test was performed to identify inter-group differences of count data, while independent sample t-test was performed for comparing the quantitative data between groups.
Results and Discussion
Baseline data of CPD patients was analyzed, where we compared and analyzed the basic characteristics of the patients like age, sex, disease course, disease type, education level and marital status of both the groups. We found no significant difference (p>0.05) (Table 1).
| Indicators | Research group (n=59) | Control group (n=55) | χ2/t | p |
|---|---|---|---|---|
| Age | 42.02±6.94 | 43.29±6.85 | 0.983 | 0.328 |
| Sex | ||||
| Male | 30 (50.85) | 27 (49.09) | 0.035 | 0.851 |
| Female | 29 (49.15) | 28 (50.91) | ||
| Disease course (y) | 4.44±0.88 | 4.38±0.73 | 0.395 | 0.694 |
| Disease type | ||||
| Periodontitis | 32 (54.24) | 35 (63.64) | 1.052 | 0.591 |
| Periodontal swelling | 18 (30.51) | 13 (23.64) | ||
| Gingivitis | 9 (15.25) | 7 (12.72) | ||
| Educational level | ||||
| Junior high school and below | 27 (45.76) | 25 (45.45) | 1.348 | 0.51 |
| Senior high school or technical secondary school | 19 (32.20) | 22 (40.00) | ||
| Junior college or above | 13 (22.04) | 8 (14.55) | ||
| Marital status | ||||
| Married | 33 (55.93) | 38 (69.09) | 2.098 | 0.148 |
| Single | 26 (44.07) | 17 (30.91) |
Table 1: Analysis of Baseline Data of Patients with CPD
Then, we analyzed the curative effect in CPD patients, in which we examined the total effective patients in the research group which was found to be 54 (91.53 %), and it was statistically elevated, compared with in the control group which was found to be 42 (76.36 %) (p<0.05) (Table 2).
| Indicators | Research group (n=59) | Control group (n=55) | χ2/t | p |
|---|---|---|---|---|
| Significant response | 33 (55.93) | 22 (40.00) | ||
| Response | 21 (35.60) | 20 (36.36) | ||
| No response | 5 (8.47) | 13 (23.64) | ||
| Overall response | 54 (91.53) | 42 (76.36) | 4.921 | 0.027 |
Table 2: Analysis of Curative Effect in Patients with CPD
Similarly, the adverse reactions among the CPD patients of two groups were observed. The research and control groups showed a comparable incidence of adverse reactions, with 6 (10.17 %) and 8 (14.54 %) respectively, experiencing discomfort, oral inflammation and edema (p>0.05) (Table 3).
| Indicators | Research group (n=59) | Control group (n=55) | χ2/t | p |
|---|---|---|---|---|
| Discomfort | 2 (3.39) | 3 (5.45) | ||
| Oral inflammation | 2 (3.39) | 2 (3.64) | ||
| Tissue edema | 2 (3.39) | 3 (5.45) | ||
| Total | 6 (10.17) | 8 (14.54) | 0.506 | 0.477 |
Table 3: Analysis of Adverse Reactions in Patients with CPD
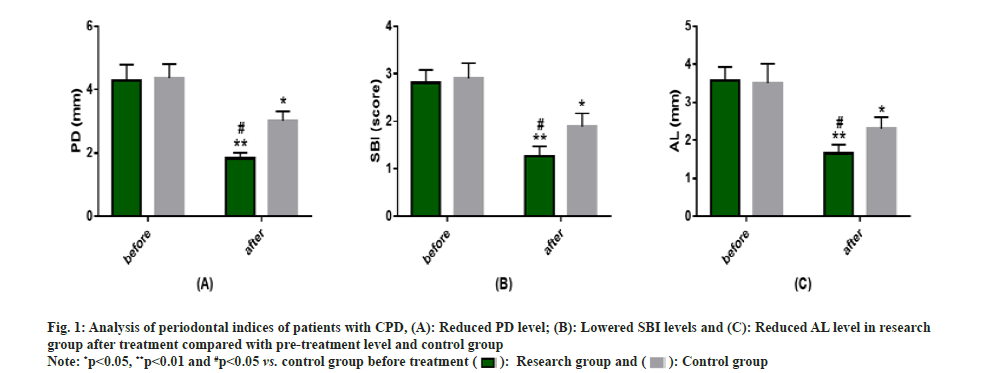
Further, periodontal indices among CPD patients in two groups were analyzed. Periodontal indices such as PD, SBI, and AL were detected and no significant inter-group differences were found in these 3 indices before treatment (p>0.05). However, after treatment these 3 indices were reduced to different degrees (p<0.05) in research group, with even lower PD, SBI and AL levels compared with the control group (p<0.05) (fig. 1).
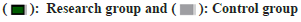
Similarly, GCF inflammatory factors in CPD patients were analyzed. The levels of inflammatory factors namely, hs-CRP, TNF-α, and IL-8 in GCF were measured and no evident difference was found between the groups before treatment (p>0.05). However, these indices showed a significantly decreased count after treatment (p<0.05), with lower hs-CRP, TNF-α, and IL-8 levels in the research group vs. the control group (p<0.05) (fig. 2).
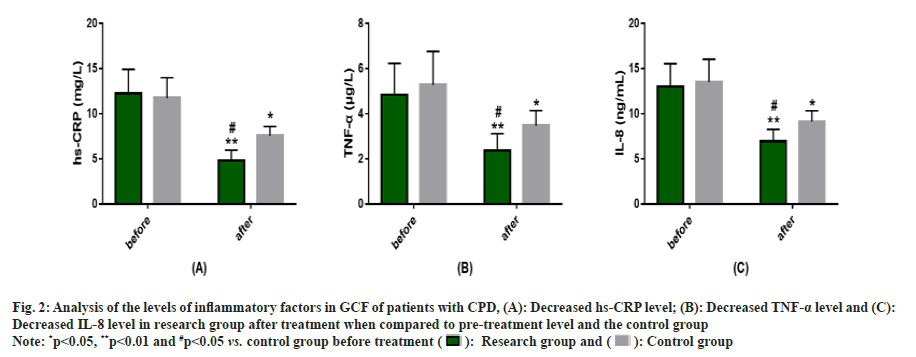
Serum MMPs in CPD patients was analyzed. Serum MMPs (MMP-3, 8, and 13) were determined and no significant difference was found between groups before treatment (p>0.05); but they all decreased significantly after treatment (p<0.05), with an even more significant reduction degree of the above indices in the research group (p<0.05) (fig. 3).
CPD progressively and negatively affects the integrity of the tissues that support the teeth and triggers other types of chronic disease in the body, which may be related to the spread of periodontal bacteria or locally activated lymphocytes to extra oral tissues[17,18]. Moreover, the damage caused by the disease to the periodontal tissue is often irreversible[19]. In order to prevent CPD progression and repair the damage of the disease to patients' body as much as possible, it is necessary to conduct in-depth exploration to find effective and safe treatments.
Here, we first evaluated the curative effects of the two treatments, and identified statistically higher ORR in the research group compared with the control group (91.53 % vs. 76.36 %), indicating that the curcumin and alcohol-containing mouthwash is better than compound gargle solution chlorhexidine gluconate in treating CPD and can significantly resolve symptoms. In the study of Anusha et al.[20], the curcumin-containing mouthwash effectively reduced disease activity when it is used in nonsurgical periodontal treatment of patients with rheumatoid arthritis and chronic periodontitis, suggesting the effectiveness of the curcumincontaining mouthwash in the treatment of chronic periodontitis, similar to our findings. As reported by Meghana et al.[21], curcumin gel used in patients with chronic periodontitis undergoing periodontal flap surgery not only inhibited tissue edema and restored tissue color, but also exerted a positive impact on wound healing and pain relief. The subsequent safety evaluation revealed that a similar incidence of discomfort, oral inflammation and tissue edema in the research and control groups (10.17 % vs.14.54 %), suggesting that the mouthwash containing curcumin and alcohol would not increase the incidence of adverse reactions in patients and has a certain safety, consistent with the research results of Anitha et al.[22]. Regarding the toxicity of curcumin in clinical trials, Chainani- Wu N et al.[23] pointed out that even if curcumin is used up to 8000 milligrams daily for 3 mo, there would be no toxic reactions. In this study the concentration of curcumin used in the mouthwash was only 2 % and the dosage was within the range of 8000 milligrams.
According to the evaluation results of periodontal indices, the research group had markedly lowered PD, SBI, and AL after treatment, lower than the pre-treatment levels and the control group, indicating that curcumin- and alcohol-containing mouthwashes facilitate periodontal rehabilitation in CPD patients. In the study of Siddharth et al.[24], subgingivally delivered 2 % curcumin also significantly improves the periodontal indicators such as PD, SBI, and AL in patients with chronic periodontitis, while being effective for patients with local and moderate chronic periodontitis and those in the periodontal maintenance stage. hs-CRP, TNF-α, and IL-8, as we all know, are all inflammatory indices reflecting GCF inflammation, which have a close positive correlation with clinical periodontal parameters and mediate the systemic inflammatory cascade in the body[25,26].
Therefore, we tested the above indicators, and found their reduced levels in the research group after treatment that were not only lower than the pre-treatment levels and the control group, suggesting that the mouthwash containing curcumin and alcohol can significantly inhibit GCF inflammation in CPD patients. Serum MMPs were also evaluated. After treatment, the MMP- 3, MMP-8, and MMP-13 of the research group reduced markedly and were significantly lower than the pre-treatment levels and the control group, indicating that mouthwashes containing curcumin and alcohol can significantly inhibit CPD procession.
Finally, the mouthwash containing curcumin and alcohol has outstanding curative effect on CPD, which is superior to the compound gargle solution chlorhexidine gluconate in efficacy and similar to it in safety. It can maintain oral health by reducing periodontal indices such as PD, SBI, and Al, while achieving anti-inflammatory effects and inhibiting CPD progression by reducing GCF inflammatory factors (hs-CRP, TNF-α and IL-8, etc.) and downregulating serum MMPs (e.g., MMP-3, MMP-8, and MMP-13).
Conflict of interests:
The authors declared no conflict of interest.
References
- Kinane DF, Stathopoulou PG, Papapanou PN. Periodontal diseases. Nat Rev Dis Primers 2017;3:1-14.
[Crossref] [Google Scholar] [PubMed]
- Woo HN, Cho YJ, Tarafder S, Lee CH. The recent advances in scaffolds for integrated periodontal regeneration. Bioact Mater 2021;6(10):3328-42.
[Crossref] [Google Scholar] [PubMed]
- Dahiya P, Kamal R, Gupta R. Obesity, periodontal and general health: Relationship and management. Indian J Endocrinol Metab 2012;16(1):88-93.
[Crossref] [Google Scholar] [PubMed]
- Oppermann RV, Weidlich P, Musskopf ML. Periodontal disease and systemic complications. Braz Oral Res 2012;26:39-47.
[Crossref] [Google Scholar] [PubMed]
- Razina IN, Chesnokova MG, Nedoseko VB. The relevance of Candida spp. in chronic periodontal disease. Stomatologiia 2017;96(4):4-6.
[Crossref] [Google Scholar] [PubMed]
- Richards D. Oral diseases affect some 3.9 billion people. Evid Based Dent 2013;14(2):35.
[Crossref] [Google Scholar] [PubMed]
- Bui FQ, Almeida-da-Silva CLC, Huynh B, Trinh A, Liu J, Woodward J, et al. Association between periodontal pathogens and systemic disease. Biomed J 2019;42(1):27-35.
[Crossref] [Google Scholar] [PubMed]
- Popa GV, Costache A, Badea O, Cojocaru MO, Mitroi G, Lazăr AC, et al. Histopathological and immunohistochemical study of periodontal changes in chronic smokers. Rom J Morphol Embryol 2021;62(1):209-17.
[Crossref] [Google Scholar] [PubMed]
- Carrizales-Sepúlveda EF, Ordaz-Farías A, Vera-Pineda R, Flores-Ramírez R. Periodontal disease, systemic inflammation and the risk of cardiovascular disease. Heart Lung Circ 2018;27(11):1327-34.
[Crossref] [Google Scholar] [PubMed]
- Kitamura M, Mochizuki Y, Miyata Y, Obata Y, Mitsunari K, Matsuo T, et al. Pathological characteristics of periodontal disease in patients with chronic kidney disease and kidney transplantation. Int J Mol Sci 2019;20(14):3413.
[Crossref] [Google Scholar] [PubMed]
- Kim Y, Clifton P. Curcumin, cardiometabolic health and dementia. Int J Environ Res Public Health 2018;15(10):2093.
[Crossref] [Google Scholar] [PubMed]
- Sehgal A, Kumar M, Jain M, Dhawan DK. Combined effects of curcumin and piperine in ameliorating benzo(a)pyrene induced DNA damage. Food Chem Toxicol 2011;49(11):3002-6.
[Crossref] [Google Scholar] [PubMed]
- Esatbeyoglu T, Huebbe P, Ernst IM, Chin D, Wagner AE, Rimbach G. Curcumin--from molecule to biological function. Angew Chem Int Ed Engl 2012;51(22):5308-32.
[Crossref] [Google Scholar] [PubMed]
- Guimarães MR, de Aquino SG, Coimbra LS, Spolidorio LC, Kirkwood KL, Rossa C Jr. Curcumin modulates the immune response associated with LPS-induced periodontal disease in rats. Innate Immun 2012;18(1):155-63.
[Crossref] [Google Scholar] [PubMed]
- Zhang Y, Huang L, Mazurel D, Zheng H, Yang J, Deng D. Clinical efficacy of curcumin vs. chlorhexidine as an adjunct to scaling and root planing for the treatment of periodontitis: A systematic review and meta-analysis. Phytother Res 2021;35(11):5980-91.
[Crossref] [Google Scholar] [PubMed]
- Fakheran O, Khademi A, Bagherniya M, Dehghannejad M, Sathyapalan T, Sahebkar A. Antibacterial activity of curcumin against periodontal pathogens: A systematic review. Adv Exp Med Biol 2021;1291:239-49.
[Crossref] [Google Scholar] [PubMed]
- Hajishengallis G, Chavakis T. Local and systemic mechanisms linking periodontal disease and inflammatory comorbidities. Nat Rev Immunol 2021;21(7):426-40.
[Crossref] [Google Scholar] [PubMed]
- Hajishengallis G. Periodontitis: From microbial immune subversion to systemic inflammation. Nat Rev Immunol 2015;15(1):30-44.
[Crossref] [Google Scholar] [PubMed]
- Dannewitz B, Holtfreter B, Eickholz P. Periodontitis-therapy of a widespread disease. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2021;64(8):931-40.
[Crossref] [Google Scholar] [PubMed]
- Anusha D, Chaly PE, Junaid M, Nijesh JE, Shivashankar K, Sivasamy S. Efficacy of a mouthwash containing essential oils and curcumin as an adjunct to nonsurgical periodontal therapy among rheumatoid arthritis patients with chronic periodontitis: A randomized controlled trial. Indian J Dent Res 2019;30(4):506-11.
[Crossref] [Google Scholar] [PubMed]
- Meghana MVS, Deshmukh J, Devarathanamma MV, Asif K, Jyothi L, Sindhura H. Comparison of effect of curcumin gel and noneugenol periodontal dressing in tissue response, early wound healing, and pain assessment following periodontal flap surgery in chronic periodontitis patients. J Indian Soc Periodontol 2020;24(1):54-9.
[Crossref] [Google Scholar] [PubMed]
- Anitha V, Rajesh P, Shanmugam M, Priya BM, Prabhu S, Shivakumar V. Comparative evaluation of natural curcumin and synthetic chlorhexidine in the management of chronic periodontitis as a local drug delivery: A clinical and microbiological study. Indian J Dent Res 2015;26(1):53-6.
[Crossref] [Google Scholar] [PubMed]
- Chainani-Wu N. Safety and anti-inflammatory activity of curcumin: A component of tumeric (Curcuma longa). J Altern Complement Med 2003;9(1):161-8.
[Crossref] [Google Scholar] [PubMed]
- Siddharth M, Singh P, Gupta R, Sinha A, Shree S, Sharma K. Comparative evaluation of subgingivally delivered 2 % curcumin and 0.2 % chlorhexidine gel adjunctive to scaling and root planing in chronic periodontitis. J Contemp Dent Pract 2020;21(5):494-9.
[Google Scholar] [PubMed]
- Dag A, Firat ET, Kadiroglu AK, Kale E, Yilmaz ME. Significance of elevated gingival crevicular fluid tumor necrosis factor-alpha and interleukin-8 levels in chronic hemodialysis patients with periodontal disease. J Periodontal Res 2010;45(4):445-50.
[Crossref] [Google Scholar] [PubMed]
- Hegde R, Awan KH. Effects of periodontal disease on systemic health. Dis Mon 2019;65(6):185-92.
[Crossref] [Google Scholar] [PubMed]