- *Corresponding Author:
- S. Y. Chan
Department of Pharmacy, General Hospital of Melaka, Jalan Mufti Haji Khalil, Melaka-75400
E-mail: sychan@usm.my
| Date of Submission | 23 August 2016 |
| Date of Revision | 28 December 2016 |
| Date of Acceptance | 24 March 2017 |
| Indian J Pharm Sci 2017;79(2):294-302 |
Abstract
The understanding of adult patients receiving cancer chemotherapy of their regimen is important for better control of chemotherapy-related side effects. Often, patients forget, misunderstand or unsatisfied with the information received. The purpose of this study is to investigate the effectiveness of pharmacist-led pre-chemotherapy counseling on the knowledge of chemotherapy treated breast cancer patients. It is a randomized and prospective study where patients were randomly distributed into intervention group who received pharmacist-led pre-chemotherapy counseling and control group who did not receive pharmacist-led pre-chemotherapy counseling. Knowledge assessments and perception of the patients were carried out after pharmacist-led pre-chemotherapy counseling in both intervention and control group using a structured validated questionnaire. Overall, 38 out of 40 patients completed the study with a 97% response rate. Significant improvement in the understanding of chemotherapy regimen and its side-effects was observed in the intervention group as compared to the control group. Besides, patients counseled by pharmacists were able to recall back the information even at the sixth cycle of the chemotherapy regimen compared to the control group. Majority of the breast cancer patients agreed that pharmacist-led pre-chemotherapy counseling was effective. This study suggests that pharmacist-led pre-chemotherapy counseling improves patient knowledge and understanding of the chemotherapy regimen received.
Keywords
Pre-chemotherapy, counselling, breast cancer, pharmacist
Incidence and prevalence of breast cancer have been increasing in Asian countries [1-3]. In Malaysia, there were about 18 219 new cancer cases diagnosed in 2007, which involved 8123 (44.6%) males and 10 096 (55.4%) females [4]. Among the cancer cases reported, breast cancer was noted to be one of the most frequently reported among Malaysians. It has taken up 18.1% of the total cancer cases, 32.1% of the female cancers cases and 33.7% of the Chinese females in Malaysia who are identified to be the group of people with the highest risk of breast cancer [4]. According to a report by the International Agency for Research in Cancer (GLOBOCAN) 2012, age-standardized incidence rate (ASR) of breast cancer in Malaysia is estimated to be 38.7 per 100 000 persons with 5410 new cases in 2012 [5,6]. Besides, the National Cancer Registry of Malaysia revealed an ASR of breast cancer in Malaysia as 29.1 per 100 000 women in 2007 [4]. This implies that approximately 1 in 35 women in the country will develop breast cancer in her lifetime.
Chemotherapy is one of the main therapies for breast cancer with the principle of destroying the actively dividing cancer cells through the use of anticancer drugs. As a result, other cells, that are actively divided in the body, such as cells in bone marrow, cells in the lining of the mouth, intestines and the hair follicles, would also be affected by chemotherapy. This leads to extensive side effects of chemotherapy such as nausea, vomiting, myelosuppression, fatigue, mucositis, diarrhoea and alopecia. Besides suffering from these side effects of the chemotherapy, there are reported isolation feel, social and physical distress cases from the effect of chemotherapy treatment [7] among breast cancer patients. This group of patients is likely to experience uncertainty and anxiety or seek scientifically unacceptable therapies, i.e. from alternative healers [7,8].
A large number of patients reported poor understanding and unable to recall what doctors had told them regarding their chemotherapy regimen. In addition, they often express dissatisfaction with the quantity and quality of information received on their disease and treatment [9,10]. This may be ascribed to the inadequate knowledge transmission during interpersonal (professional-layman) communication and care [11]. In a study by Hogbin and Fallowfield, time constraints, poor communication skills in doctors, physicians withholding information and patients’ incapability to remember the information were the major reasons for inadequate knowledge transmission [12]. As a consequence, patients are less likely to neither comply or adhere to the prescribed treatment and medical advice, nor take part in the medical decision-making process, which may contribute negatively to the long-term outcomes [8,9,13,14]. According to a study conducted in Amsterdam, cancer patients wish to be well-informed about both general and specific aspects of their diagnosis, prognosis and treatment [15-17]. Therefore, information is of considerable importance in helping patients and their families to cope with the chemotherapy related complications.
Most studies showed the positive effect of counselling on quality of life for patient [7,16,18-20]. Cozaru and coworkers found that, among the categories of counselors who helped in alleviating the distress of breast cancer patient, only 23% was attributed by medical team [20]. In this context, the involvement of a pharmacist in the counseling was not specified. As multidisciplinary approach of medical staffs has been reported to give rise to the optimum outcome of patient care [21], in the recent years, the role of the pharmacist has been actively incorporated into the primary health care system in revealing pharmaceutical care in Malaysia. The involvement of a pharmacist has led to improvement in health outcomes and cost-effective therapy [22]. For instance, pharmacist-led medical therapy adherence clinic of warfarin and pharmacistled diabetes counselling have shown great impact on patient compliance to the medicine prescribed [22].
To the best of our knowledge, there are only limited studies reported on the effectiveness of pharmacistled pre-chemotherapy counselling to cancer patients in Malaysia. One of those is the study reported by Periasamy et al. in 2015 in which the positive outcome of chemotherapy counseling by a pharmacist has been attributed to psychological effect and self-esteem in oncology patient [23]. Since chemotherapy is one of the main therapies for breast cancer patient, it is important for the patient to better understand the regimen, expectation and its influence on their daily life throughout the treatment period. In light of this, purpose of current study is to determine the effectiveness and benefits of a pharmacist-led chemotherapy counselling to breast cancer patients in Hospital Melaka.
Materials and Methods
Ethical approval:
This study was registered under National Medical Research Register of Malaysia with the registration number of NMRR-10-742-6077. Permission to conduct this study was obtained from the Ministry of Health, Research and Ethnics Committee, Malaysia.
Development of the questionnaire:
Questionnaire was designed to collect information on socio-demographic data, patients’ knowledge, perception and adherence to the chemotherapy prescribed. It was developed in English and translated to the national language Bahasa Melayu. In addition to the socio-demographic data (gender, age, race, education, occupation and marital status), the questionnaire consisted of 22 items, which were divided into three-dimension structured categories that included firstly, patients’ general knowledge, side effects management and potential interaction of their prescribed chemotherapy: 11 questions. Secondly, patients’ adherence attitudes: 5 questions and finally patients’ perception with pharmacy services: 6 questions.
Subjects:
Subjects of the study were breast cancer patients. Inclusion criteria of the patients are listed below: patient who were enrolled to Hospital Melaka to receive chemotherapy, patient who were diagnosed with breast cancer, including local or metastasised, patient who were 18 y or older, patient who were about to take chemotherapy for the first time, patients who were willing to participate in the study and patient who were able to speak in Bahasa Melayu, English or Mandarin. Patients who received oral chemotherapy or those on palliative care were excluded.
Sample size:
Power and sample size calculation software version 3.12 was used to calculate the sample size. According to the calculated sample size, 24 patients were needed in each group (control and intervention groups) to detect significant difference between the groups with 80% power and alpha 0.05. The source of standard deviation and detectable difference was taken as 2.14 and 1.75, respectively as reported by Periasamy et al. [23] with significant effect of counseling on patient’s outcome. However, the obtained sample size obtained in the current study was highly dependent on the available number of patients who enrolled for chemotherapy treatment in the permitted study time frame by the ethical approval from Ministry of Health Research and Ethnics Committee, Malaysia.
Procedure and data collection:
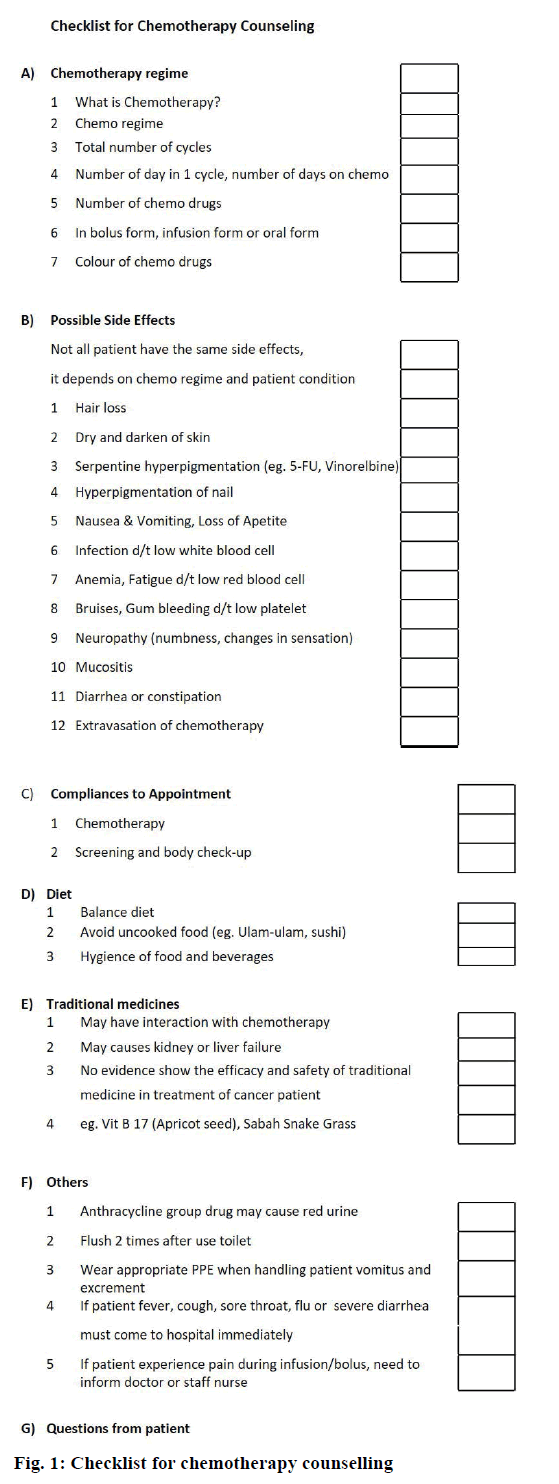
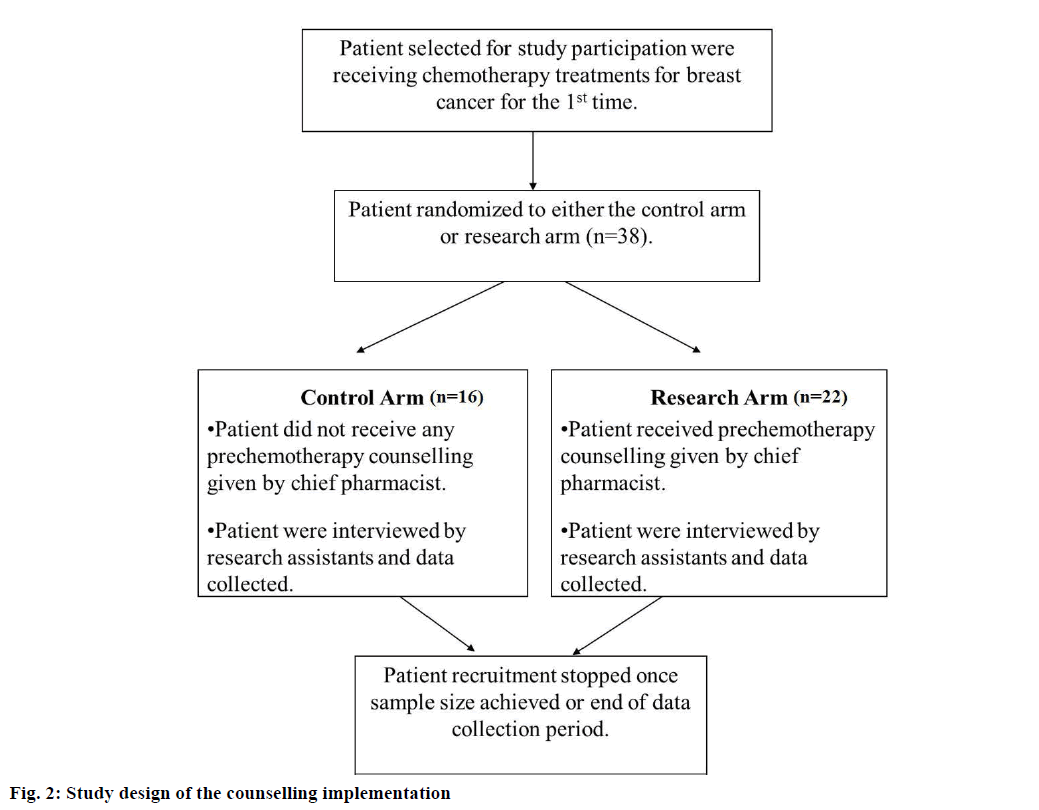
This study employed a randomized blinded and prospective study design. All the patients who were undergoing first time chemotherapy regimen were invited to join the study and asked to provide written informed consent. The participated patients were randomized to the control arm, where they did not receive any pre-chemotherapy counselling or the intervention arm where chemotherapy counselling was given by a chief pharmacist according to simple random sampling technique. The pharmacist-led prechemotherapy counselling was carried out in face-toface manner using a chemotherapy counselling checklist as shown in Figure 1. The counselling points covered the purpose of chemotherapy treatment, chemotherapy side effects and its management, importance of compliance to chemotherapy appointment date and the possibility of interaction between chemotherapy and traditional medicine.
After pharmacist-led chemotherapy counseling, the participated patients in both arms were asked to complete a questionnaire through a 15-20 min faceto- face interview by two trained research assistants after second and sixth cycle of their chemotherapy regimen using the developed 22-item questionnaire. These research assistants were blinded about the status of the participants (not informed whether the patient was in control arm or intervention arm). The interviews were conducted in wards or day care clinic in Hospital Melaka. Figure 2 outlines the flow of the study design.
The participated patients were awarded one point for each correct response and zero points for each wrong or “not sure” response on questions related to assessment of chemotherapy knowledge. Questions on the source of information provided and perception on the effectiveness of the pharmacist-led counselling were not scored.
Data analysis:
All analyses were performed using statistical packages for social sciences (SPSS) version 15.0. A 2-sided P<0.05 was considered statistically significant. Student’s t-test was used to test for group differences and interval level data; while Pearson correlation test was used to find the relationship between the study measures and the pharmacist-led intervention. When more than two categories’ means are compared, oneway ANOVA was used to test the mean differences.
Results and Discussion
Due to the limited number of patients enrolled for the chemotherapy regimen, the current sample size was below the calculated value, which required 24 patients in each group. Only 40 patients were approached for the survey based on the patient’s enrolment of chemotherapy treatment. However, two patients rejected the interview. Hence, the total sample size was 38 with 95% (38/40) response rate.
Socio-demographic information of 38 breast cancer patients was presented in Table 1. All of the patients in this study were female (100%) although male (0%) was not an exclusion criterion. The majority of the patients were Malay (68.4%) followed by Chinese (23.7%). Approximately 50% of the patients were aged between 50-60 y old. Most of the patients received only secondary education (47.4%).
| Characteristics | Number of patients (n=38) | Percentage (%) |
|---|---|---|
| Gender | ||
| Male | 0 | (0%) |
| Female | 38 | (100%) |
| Race | ||
| Malay | 26 | (68.4%) |
| Chinese | 9 | (23.7%) |
| Indian | 2 | (5.3%) |
| Others | 1 | (2.6%) |
| Age (in y) | ||
| 18-30 y | 1 | (2.6%) |
| >30-40 y | 2 | (5.3%) |
| >40-50 y | 11 | (29.0%) |
| >50-60 y | 20 | (52.6%) |
| >60 y | 4 | (10.5%) |
| Education level | ||
| None | 4 | (10.5%) |
| Primary | 16 | (42.1%) |
| Secondary | 18 | (47.4%) |
| Tertiary | 0 | (0%) |
| Occupation | ||
| Employed | 2 | (5.3%) |
| Not employed | 4 | (10.5%) |
| Self-employed | 1 | (2.6%) |
| Housewife | 27 | (71.1%) |
| Retired | 4 | (10.5%) |
| Status | ||
| Single | 0 | (0%) |
| Married | 37 | (97.4%) |
| Widow/widower | 1 | (2.6%) |
| Divorcee | 0 | (0%) |
Table 1: Socio-Demographic information of the participated breast cancer patients (N=38)
During the counselling session for intervention group several common queries have been raised. These include, “Can I take supplement?”, “What type of food do I need to avoid?”, “Will the side effects be permanent?” and also “What do I need to do if side effects occur?” All the raised queries were responded accordingly by the chief pharmacist.
Table 2 showed the result of Pearson correlation test that correlate the socio-demographic data of the patient to score of their knowledge related to chemotherapy. Occupation did not significantly correlate with patients’ knowledge score (occupation P=0.475). On the contrary, education and age shown significant weak correlation with knowledge score at correlation value of r=0.361 (it is defined as “weak correlation” in Pearson correlation test) at statistical P=0.001 and r=0.249 at statistical P=0.030, respectively (Table 2). This result is in agreement to a study by Pohls et al., who indicate that advanced education level leads to superior knowledge in relation to breast cancer incidence and various personal risk factors [24].
| Statistical tests | Both groups | Research | Control |
|---|---|---|---|
| Correlations test | P value, correlation coefficient (Patient demographic vs. knowledge score) | ||
| Occupation | 0.475, r=–0.083# | 0.215, r=–0.119# | 0.466, r=0.016# |
| Education | 0.001**, r=0.361 | 0.001*,r=0.436 | 0.140,r=0.204 |
| Age | 0.030**, r=–0.249 | 0.055, r=–0.239 | 0.160, r=-0.188 |
| Counselling | 0.001**,r=–0.353 | - | - |
| Student’s t-test | P value (Intervention vs. control group) | Mean of knowledge score | Mean of knowledge score |
| Both cycles | 0.002*, 95% CI | 5.76 ± 0.49 | 4.38 ± 2.22 |
| At 2nd cycle | 0.019*, 95% CI | 5.83 ± 0.52 | 4.27 ± 2.40 |
| At 6thcycle | 0.047*, 95% CI | 5.70±0.50 | 4.50 ± 2.10 |
| One-way Anova | P value | Research (P value) | Control (P value) |
| (Compare among different education backgrouds) | |||
| At 2ndcycle | 0.024* | 0.109 | 0.069 |
| At 6thcycle | 0.101 | 0.280 | 0.295 |
Table2: Relationship between patient demographic, pharmacist-led counseling and patients’ knowledge scores
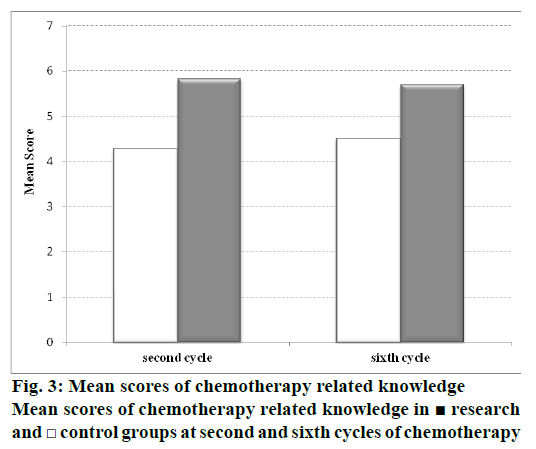
Figure 3 showed the mean score of participants in the control and intervention groups. The mean scores of participants in intervention group were 5.83±1.52 and 5.70±1.50 in the second and the sixth cycle, respectively. On the other hand, the mean score of participants in control group was 4.27±2.40 and 4.50±2.10 in the second and the sixth cycle, respectively. No significant differences were observed in the knowledge score of both groups between the second and the sixth cycle. However, comparing the control and intervention group, Student’s t-test analysis showed that there was a significant difference between mean score of intervention group and control group with P<0.05 (P=0.019), CI=(0.115, 3.004) at second cycle and P<0.05 (P=0.047), CI=(0.014, 2.377) at sixth cycle. This implies the positive influence of pre-chemotherapy counselling to the patients in intervention group.
As there is weak positive correlation found between the education backgrounds and score knowledge of the patients as mentioned in previous section (Table 2), further analysis was carried out to identify possible influence of education background as confounding factor that give rise to false positive of pre-chemotherapy effect on the studied samples. To do this, One-way ANOVA was performed to compares the mean score differences among the different education levels, i.e. not educated, primary education and secondary education in this study. It is found that there is no significant differences between the education backgrounds and knowledge score at 6th cycle of chemotherapy with the obtained P=0.101 (P>0.05). On the contrary, knowledge score at 2nd cycle revealed significant differences with education backgrounds with the obtained P=0.024 (P<0.05). These results could neither rule out nor confirm the effect of background education as confounding factor that lead to false positive effect of pre-chemotherapy effect on patient’s knowledge since both cycles shows significant different of means knowledge score between the control and intervention groups after prechemotherapy counselling. Furthermore, when the dataset of both group were analyse separately, there was insignificant different of means score knowledge from the different education backgrounds (Table 2, one-way ANOVA test) in the respective groups. Since significant weak correlation between the education background and knowledge score has been identified, hence, the potential of the education background as confounding factor shall not be overlooked. More extensive study shall be carried out to reconfirm this.
One of the shortcoming of the current study is that baseline knowledge score for both intervention and control group was not taken. However, as the purpose of the study is focusing on differentiating the knowledge score between and intervention and control group, hence the analysis is still valid.
Both control and intervention groups had 100% adherence. Patient adherence in this study reflected patients who completed six cycles of chemotherapy and did not drop out at any cycles. This may be due to the systematic reminder of the DCC in general hospital Melaka, which contacted the patients a day before their appointed chemotherapy date.
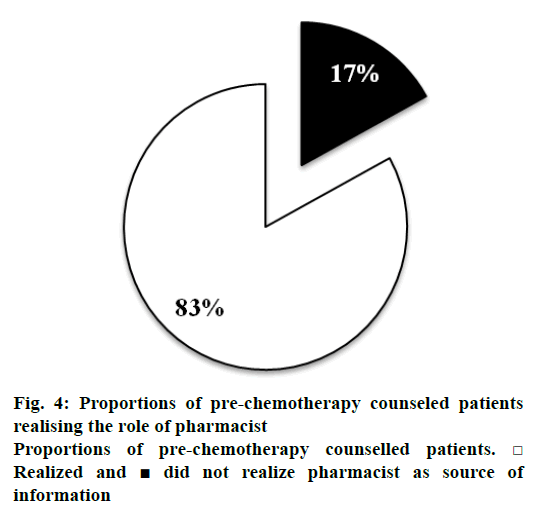
Despite the pharmacist-led counselling, some patients showed uncertainty and did not realize who contributed to the source of information received. Figure 4 compares the percentage of patients between those who did and did not realize pharmacist as the prechemotherapy counsellor. It can be seen for the pie chart that, significant proportion (i.e. 83%) of the prechemotherapy counselled patients were able to identify pharmacists as source of information.
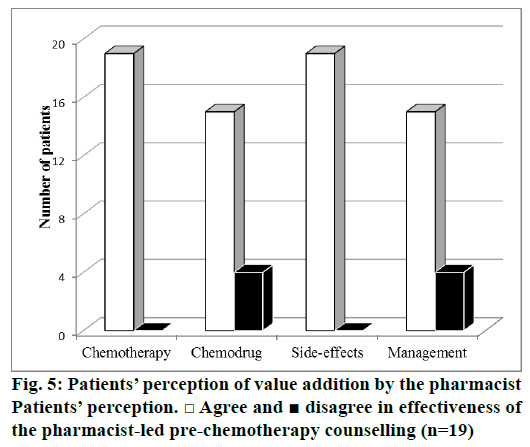
As the role of pharmacist is closely related to patient’s perception, this component was further evaluated in those patient who knew pharmacist as a source of information (n=19). Figure 5 displayed the patients’ perception on the information received. More than 70% of them agreed that counseling offered by the pharmacist was effective. This includes the chemotherapy regimen, the drug, side effects and their management. This result is in agreement to a recently conducted study in managing complex medication needs [25].
Breast cancer is a traumatizing disease associated with complex therapies [26]. Oftentimes, newly diagnosed breast cancer patient is likely to face multiple concerns such as physical, emotional and chemotherapy side effect [20,27]. The impact may be intensified when the patient is exposed to their first chemotherapy regimen [27]. In this regards, adequate information or patient counselling must be supplied in addressing potential fears or stigmas associated with chemotherapy and hence increase adherence to the given treatment [27]. On the other hand, integrating pharmacist into the primary health care system has been increasingly recognized as a means to manage complex medication needs, reduce drug costs, length of hospital stay and improve economic outcomes [25,28]. The role of pharmacist has been diversified from medication centred to patient centred care [29]. Studies showed that pharmacist involvement was well accepted with high satisfactory score by both the patient and physicians [25,30]. In oncology setting however, the role of the pharmacist is rather in an imbalance, which deals with compounding of the drug, calculation of body surface area of patients and communication to the prescriber [26,28]. Limited activity has been focused on cancer patient-centred care.
In the current study, all the counseling sessions were conducted by an experienced chief pharmacist with a particular focus on the management of chemotherapy including side-effects, compliance as well as potential interaction with traditional medicines. The presented results showed that there was significant different in the knowledge assessment score between patient who were counselled and not counselled by pharmacist. One may argue that the increase in knowledge score does not necessarily improves patient outcomes. However, a few studies have proven the link between the knowledge and outcomes for patient outcome [31]. This has strengthened the essentiality of pre-chemotherapy counselling.
A survey indicated that less than 70% of the information given to cancer patients was understood despite the prior discussion with their physicians [32]. Pharmacist has been suggested to be the ideal bridge information between physicians and patient [28], in the current study, patient centred care via pharmacist was attempted through pre-chemotherapy counselling. It has been shown that pharmacist-led pre-chemotherapy counselling was effective in conveying chemotherapy drug related messages. This finding is in agreement to a study where pharmacist has given rise to positive input to the patient and established industry-independent drug information for both patient and physicians besides the traditional role of pharmacist in compounding cytotoxic drug [26]. As the appreciation of specialize knowledge of pharmacist in oncology field is increasing, the role of pharmacist in patient centred care in oncology setting shall be focused for optimum therapeutic outcomes.
In regard to the role of pharmacist in pre-chemotherapy counselling, majority of the patients were able to identify pharmacist as source of information. However, 17% of the patient did not recognize the source of information given, which may be attributed to the perception of patient who sees the pharmacist as a medication distributor [33] or the limited role of pharmacist in the primary health care system in Asian countries, particularly in Malaysia [2]. Apart from that, a few patients in the current study did not agree that pharmacist helped to understand and remember the medication for chemotherapy to overcome the sideffects. Further investigation should be carried out in this aspect to improve the counseling competencies to recognize limitation of the pharmacist-led prechemotherapy interventions. As the pharmacist is said to be the most accessible healthcare professional [25] and the ideal middle man to bridge the gap between the physician and patient [28], its role in the oncology setting may highly contributed to positive therapeutic outcome and prevention of chemo-drug related problem.
The current study highlighted that chemotherapy counseling conducted by the pharmacist was effective. Knowledge assessment between the control and intervention groups showed that age and occupation did not influence patients’ knowledge. However, patient’s education level is shown to be related to the ability in receiving the knowledge. After pharmacist intervention, it was found that the intervention group had better knowledge scores and understanding of their chemotherapy regimen, chemo drug side effects and its management. Besides, patients had good perception of the pharmacist-led pre-chemotherapy counselling. Overall, pharmacist-led pre-chemotherapy counseling has not only contributed positively to the knowledge of breast cancer patients but has also given a good impression of oncology pharmacist in the treatments of breast cancer patients. With that in mind, the role of oncology pharmacists should be extended as part of the primary care management of breast cancer patients, which includes pre-chemotherapy counseling and the expansion and scaling up of this pharmacist-led patientcentred intervention in Malaysia is the next challenge!
Acknowledgements
The participation of the breast cancer patients in this study is greatly appreciated.
Conflict of interests
Authors report no conflict of interests.
Financial support and sponsorship
Nil.
References
- Ghafoor Q, Sanghera P, Grieve RJ. A Study of medical intervention in routine breast cancer follow-up. Clin Oncol 2010;22:91-6.
- Bhoopathy N, Yip CH, Hartman M, Uiterwaal CSPM, Devi BCR, Peeters PHM, et al. Breast cancer research in Asia: Adopt or adapt Western knowledge? Eur J Cancer 2013;49:703-9.
- Bhoopathy N, Yip CH, Hartman M, Saxena N, Taib NA, Ho GF, et al. Adjuvant! Online is overoptimistic in predicting survival of Asian breast cancer patients. Eur J Cancer 2012;48:982-9.
- Omar ZA, Tamin NSI. National Cancer Registry Report 2007. Malaysia: National Cancer Registry, Ministry of Health, Malaysia; 2011.
- http://globocan.iarc.fr/Pages/fact_sheets_cancer.aspx.
- Yip CH, Bhoopathy N, Teo SH. A Review of Breast Cancer Research in Malaysia. Med J Malaysia 2014;69:8-22.
- Ganz PA, Yip CH, Gralow JR, Distelhorst SR, Albain KS, Andersen BL, et al. Supportive care after curative treatment for breast cancer (survivorship care): Resource allocations in low- and middle-income countries. A Breast Health Global Initiative 2013 consensus statement. Breast 2013;22;606-15.
- Jefford M, Tattersall MHN. Informing and involving cancer patients in their own care. Lancet Oncol 2002;3:629-37.
- McPherson CJ, Higginson IJ, Hearn J. Effective methods of giving information in cancer: a systematic literature review of randomized controlled trials. J Public Health Med 2001;23:227-34.
- Butow PN, Maclean M, Dunn SM, Tattersall MH, Boyer MJ. The dynamics of change: cancer patient's preferences for information, involvement and support. Ann Oncol 1997;8:857-63.
- Abu Abed M, Himmel W, Vormfelde S, Koschack J. Video-assisted patient education to modify behavior: A systematic review. Patient Educ Couns 2014;97:16-22.
- Hogbin B, Fallowfield L. Getting it taped: the “bad news” consultation with cancer patients. Br J Hosp Med 1989;41;330-3.
- Ong LM, Visser MR, Lammes FB, van Der Velden J, Kuenen BC, de Haes JC. Effect of providing cancer patients with the audiotaped initial consultation on satisfaction, recall and quality of life: a randomized, double-blind study. J Clin Oncol 2000;18:3052-60.
- Iconomou G, Viha A, Koutras A, Vagenakis AG, Kalofonos HP. Information needs and awareness of diagnosis in patients with cancer receiving chemotherapy: a report from Greece. Palliat Med 2002;16:315-21.
- Derdiarian AK. Informational needs of recently diagnosed cancer patients. Nurs Res 1986;35:278-81.
- Wevers MR, Hahn DEE, Verhoef S, Bolhaar MDK, Ausems MGEM, Aaronson NK, et al. Breast cancer genetic counseling after diagnosis but before treatment: A pilot study on treatment consequences and psychological impact. Patient Educ Couns 2012;89:89-95.
- Tattersall MH, Butow PN, Griffin AM, Dunn SM. The take-home message: patients prefer consultation audiotapes to summary letters. J Clin Oncol 1994;12:1305-11.
- Al-Arifi MN. Patients’ perception, views and satisfaction with pharmacists’ role as health care provider in community pharmacy setting at Riyadh, Saudi Arabia. Saudi Pharm J 2012;20:323-30.
- Hoving C, Dercksen MW, Bosch H, Golde R, Tjan-Heijnen VCG, Roijen J, et al. 42 Novice Research Dissemination Awardee: Fertility counseling in young women with breast cancer: a cross-sectional study. Eur J Oncol Nurs 2014;18:S11.
- Cozaru GC, Papari AC, Sandu ML. The Effects of psycho-education and counselling for women suffering from breast cancer in support groups. Procedia Soc Behav Sci 2014;128:10-5.
- Harford JB, Otero IV, Anderson BO, Cazap E, Gradishar WJ, Gralow JR, et al. Problem solving for breast health care delivery in low and middle resource countries (LMCs): consensus statement from the breast health global initiative. Breast 2011;20:S20-S9.
- Al-Quteimat OM, Amer AM. Evidence-based pharmaceutical care: The next chapter in pharmacy practice. Saudi Pharm J 2016;24:447-51.
- Periasamy U, Sidik SM, Rampal L, Ismail SIF. Outcome of chemotherapy counseling by pharmacists on psychological effects and self esteem among oncology patients in a Government Hospital in Malaysia. Med J Malaysia 2015;70:131-41.
- Pöhls UG, Renner SP, Fasching PA, Lux MP, Kreis H, Ackermann S, et al. Awareness of breast cancer incidence and risk factors among healthy women. Eur J Cancer Prev 2004;13:249-56.
- Chen CH, Liau YJ, Wu PF. Inpatient satisfaction with TCM medication counseling services provided by pharmacists. Eur J Integr Med 2012;4:e281-e8.
- Döhler N, Krolop L, Ringsdorf S, Meier K, Ko YD, Kuhn W, et al. Task allocation in cancer medication management -Integrating the pharmacist. Patient Educ Couns 2011;83:367-74.
- Reece JC, Chan YF, Herbert J, Gralow J, Fann JR. Course of depression, mental health service utilization and treatment preferences in women receiving chemotherapy for breast cancer. Gen Hosp Psychiatry 2013;35:376-81.
- Francis J, Abraham S. Clinical pharmacists: Bridging the gap between patients and physicians. Saudi Pharm J 2014;22:600-2.
- Rayes IK, Hassali MA, Abduelkarem AR. The role of pharmacists in developing countries: The current scenario in the United Arab Emirates. Saudi Pharm J 2015;23:470-4.
- Al Rahbi HAM, Al-Sabri RM, Chitme HR. Interventions by pharmacists in out-patient pharmaceutical care. Saudi Pharm J 2014;22:101-6.
- Huynh TK, Trovato JA. Assessment of patients’ knowledge and management of chemotherapy- related adverse effects. J Hematol Oncol Pharm 2014;4:123-7.
- Hershman D, Calhoun E, Zapert K, Wade S, Malin J, Barron R. Patients' perceptions of physician-patient discussions and adverse events with cancer therapy. Arch Drug Inf 2008;1:70-8.
- Liekweg A, Eckhardt M, Taylor SM, Erdfelder E, Jaehde U. Psychometric assessment and application of a questionnaire measuring patient satisfaction with information on cancer treatment. Pharm World Sci 2005;27:96-103.
 research
and
research
and  control groups at second and sixth cycles of chemotherapy
control groups at second and sixth cycles of chemotherapy