- *Corresponding Author:
- Qin Zeng
Department of Paediatric Nursing, West China Second University Hospital/West China School of Nursing, Sichuan University, Sichuan 610041, China
E-mail: zeng212212@163.com
| This article was originally published in a special issue, “Modern Applications in Biomedical Research and Pharmaceutical Sciences” |
| Indian J Pharm Sci 2022:84(3) Spl Issue “277-283” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
We systematically attempt to evaluate the influencing factors of drug treatment compliance in childhood asthma and to provide evidence for improving patient’s treatment compliance and improving treatment success rate. The Chinese literatures that met the inclusion and exclusion criteria, such as Wanfang Medical Database, China National Knowledge Infrastructure, VIP Chinese Science and Technology Periodical Database and Chinese Biomedical Database were systematically searched. Two researchers screened the literature, conducted strict quality evaluation, extracted data from literatures that met the quality standards and used RevMan5.3 statistical software to make forest charts for outcome indicators and analyze effects. A total of 13 literatures were included. Meta-analysis results showed that lack of asthma knowledge, bad psychology and parent’s trust in medical staff had no statistically significant effects on children’s treatment compliance, while the degree of illness had a statistically significant impact on compliance (p<0.1), the pooled odds ratio and 95 % confidence interval was 0.31 (0.22-0.43). The severity of illness is the main factor for drug treatment compliance in childhood asthma.
Keywords
Childhood asthma, corticosteroids, asthma, medication compliance
Bronchial asthma is a common chronic airway inflammatory disease in children characterized by airway hyper responsiveness, airway inflammation and airway remodeling[1]. Asthma attacks manifested as coughing, wheezing, chest tightness, etc., mostly at night or in the early morning[2]. About 300 million people worldwide have a history of asthma, asthma prevalence in European children ranges from 5 % to 20 %, the cumulative prevalence of asthma in urban children under 14 y old in China increased from 1.09 % in 1990 to 3.02 % in 2010[3,4]. At present, inhaled corticosteroids, oral leukotriene receptor antagonists and proper bronchodilators are mainly used for treating asthma[5]. Study shows 34 % of asthma deaths are due to poor medication compliance[6]. The reasons may be that parents have insufficient awareness of asthma knowledge, unfamiliarity with drug inhalation devices and their use methods, and worry about drug side effects, which lead to a decline in medication compliance[7]. Moreover, many studies have shown that there are many factors that affect childhood asthma medication compliance, but the results are inconsistent. In order to further clarify the influencing factors of medication compliance in childhood asthma, this study adopts meta-analysis method in evidence-based medicine to comprehensively analyze the influencing factors of childhood asthma medication compliance in recent years in China, to provide reliable and effective data for improving children’s medication compliance and improving asthma control rate.
Materials and Methods
Literature search:
Literature source: Literature are from China National Knowledge Infrastructure (CNKI), Wanfang Medical Database, VIP Chinese Science and Technology Periodical Database and Chinese Biomedical Database (CBM), Chinese search subject headings are "children" or "sick children", "bronchial asthma", "inhalation therapy", "compliance" or "medication compliance", "factor", at the same time, review the references and search to collect more relevant literature.
Literature type: All published domestic literatures related to the influencing factors of childhood asthma medication compliance.
Literature inclusion and exclusion criteria:
Literature inclusion criteria: Studies on the influencing factors of medication compliance in childhood asthma in China from January 2001 to April 2022 and the original data is complete, and relevant data can be directly or indirectly extracted for statistics.
Literature exclusion criteria: Literature reviews, other meta-analyses or conference papers; data missing or no analysis of influencing factors; literature with repeated reports, small sample size; low reliability and lack of study controls.
Literature screening:
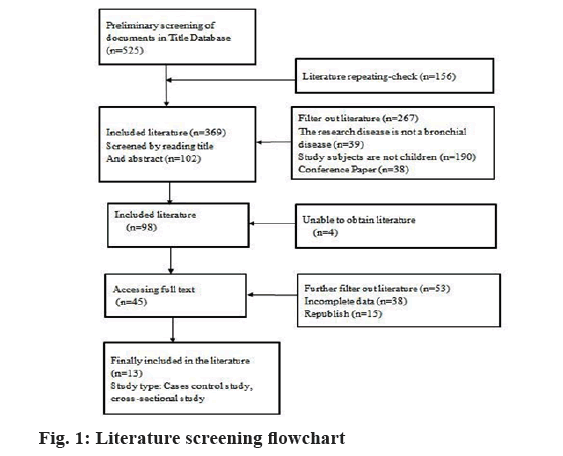
Firstly, according to the retrieval strategy screened the titles and abstracts of the literature in the selected database. After deduplication, complete the screening in two rounds according to the inclusion and exclusion criteria, first round screening by reading title and abstract, second round screening by reading the full article.
Data extraction:
Summarized the included literature, including the first author, publication time, number of investigators, good and bad compliance results, and influencing factors. Inclusion and exclusion of retrieved articles were independently performed by 2 investigators and cross-checked, in the event of disagreement, a third researcher will be asked to make a judgment.
Quality evaluation:
Adopt Agency for Health Research and Quality (AHRQ) recommended cross-sectional study evaluation criteria for quality assessment of included studies, the scale contains 11 items, use "yes", "no" and "unclear" to classify, respectively, and record "1", "0" and "10" points respectively. The total score is 0~11 points, of which 0~3 is low quality, 4~7 is medium quality, and 8~11 is high quality. The evaluation results of the AHRQ scale showed that the scores of the included studies were between 6 and 8, indicating that the quality of the included studies was above medium.
Statistical analysis:
Adopted RevMan5.3 statistical software to make a forest chart for the outcome indicators of interest and analyzed the effects, the data were combined specifically and tested for heterogeneity. When I2<50 % or p>0.1, it can be considered that multiple studies are homogeneous and adopted the fixed effect model; when I2>50 % or p<0.1, it is considered that various studies are heterogeneous, and adopted the random effect model. The outcome of this study was enumeration data and adopted Odds Ratio (OR) to analyze each effect size, expressed by 95 % Confidence Interval (CI). Adopted funnel plot and Begg’s test to detect publication bias, if the distribution of the inverted funnel plot is uniform and symmetrical, and p<0.05, it means that there is no publication bias.
Results and Discussion
From 2001 to 2022, a total of 525 related Chinese articles were retrieved. According to the inclusion and exclusion criteria, a total of 13 articles were finally included. A total of 2330 cases were investigated, of which 881 had good medication compliance, accounting for 37.81 % of the total. Among them, there were 11 high-scoring papers and 2 medium-quality papers, as shown in fig. 1 and Table 1[8-20].
| Serial number | First author | Year of publication (year) | Total number of people investigated (case) | Number of compliance (case) | Number of non-compliance (case) |
|---|---|---|---|---|---|
| 1 | Li JY[8] | 2007 | 168 | 88 | 80 |
| 2 | Shen XC[9] | 2010 | 186 | 59 | 127 |
| 3 | Yang YZ [10] | 2012 | 120 | 40 | 80 |
| 4 | He S[11] | 2012 | 140 | 50 | 90 |
| 5 | You Z[12] | 2013 | 106 | 40 | 66 |
| 6 | Luo QR[13] | 2013 | 130 | 42 | 88 |
| 7 | Zhang N[14] | 2015 | 209 | 84 | 125 |
| 8 | Zhang Y[15] | 2017 | 181 | 84 | 97 |
| 9 | Liang ML[16] | 2018 | 160 | 65 | 95 |
| 10 | Hu ST[17] | 2019 | 60 | 28 | 32 |
| 11 | Zhong TS[18] | 2020 | 350 | 88 | 262 |
| 12 | Du J[19] | 2021 | 100 | 26 | 74 |
| 13 | Wang YY[20] | 2021 | 420 | 187 | 233 |
Table 1: General Characteristics of the Included Literature
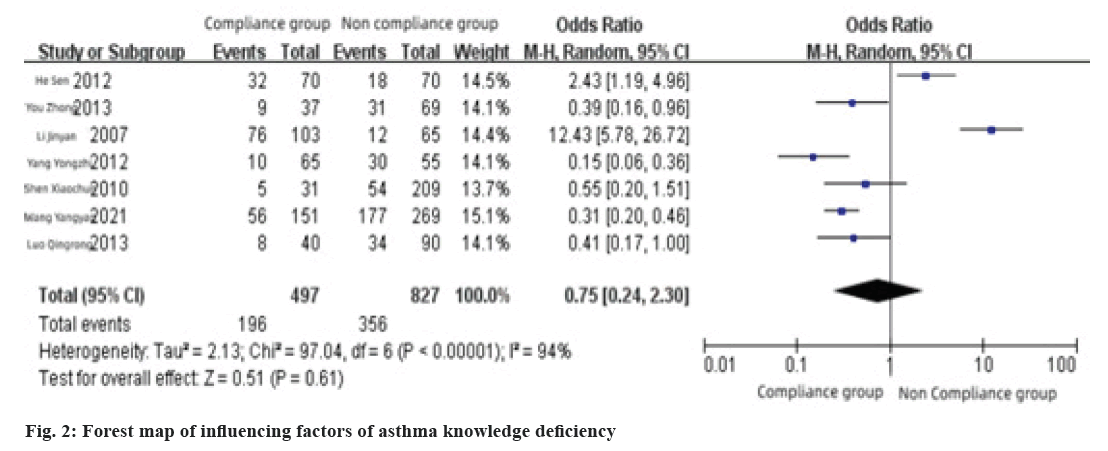
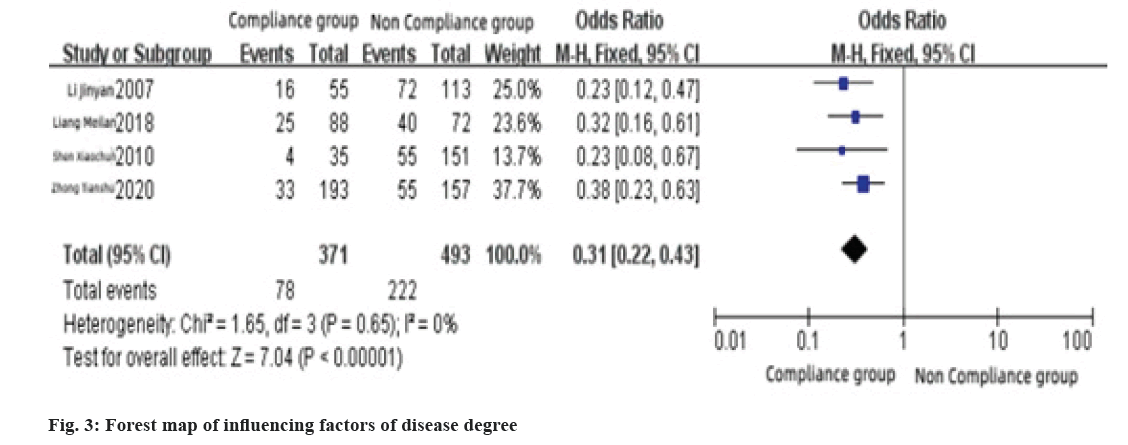
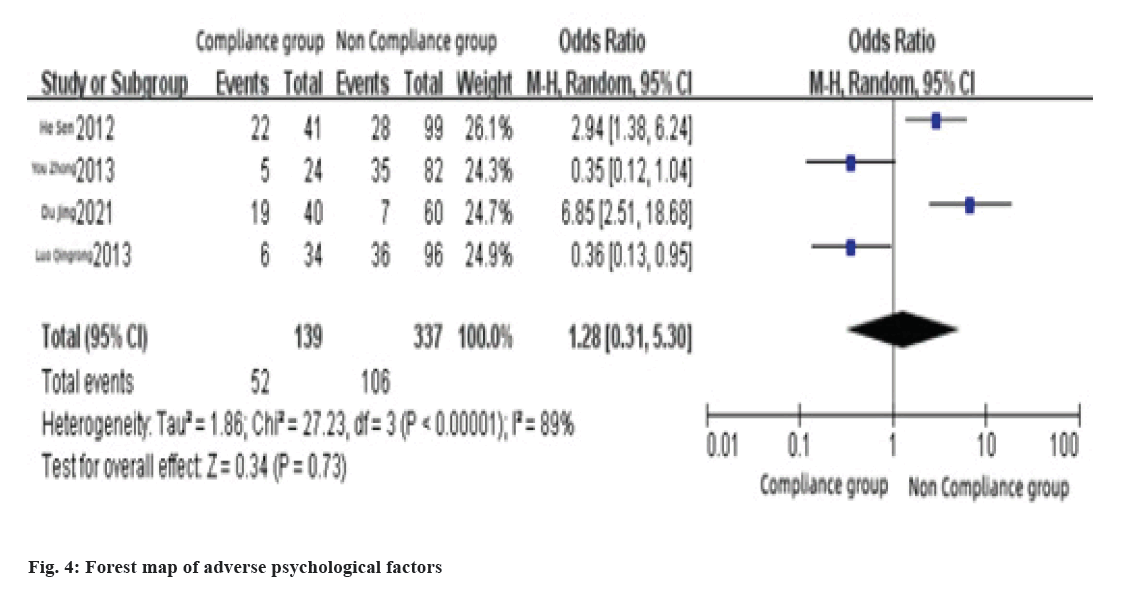
The results of the heterogeneity test showed that there was no heterogeneity among the related literatures (I2<50 %, p>0.1), so adopted the fixed effect model; lack of asthma knowledge, bad psychology, parent’s trust in medical staff (I2>94 %, p<0.1), so adopted random effects model. The results of the combined effect test showed that the lack of asthma knowledge, bad psychology and parent’s trust in medical staff had no statistically significant effects on children’s treatment compliance, but the degree of illness has a statistically significant effect on compliance, as shown in Table 2 and Table 3.
| Serial number | Influencing factors of the study | Score |
|---|---|---|
| 1 | Knowledge of asthma, drug awareness, trust of medical staff, severity of asthma, speed of symptom relief, family's financial situation, educational level of parents | 9 |
| 2 | Educational level of parents, knowledge of asthma, drug awareness, degree of illness, drug factors, trust of medical staff, family's financial situation, environmental factors | 9 |
| 3 | Lack of disease knowledge, adverse drug reactions, young age, little psychological support | 8 |
| 4 | Lack of bronchial asthma knowledge, adverse psychological reaction, adverse drug reactions, young age | 10 |
| 5 | Lack of knowledge about disease and hormone inhalation, existed adverse psychological reactions, not mastering hormone inhalation technology, general doctor-patient relationship | 10 |
| 6 | Lack of asthma knowledge, adverse psychological reactions, lack of awareness of inhaled hormones, general doctor-patient relationship | 9 |
| 7 | Parents' cognitive level, children's control over their parent’s lives, parental control over children’s behavior | 7 |
| 8 | Cumulative time of taking hormones, is the child involved, knowledge of hormone medication in children, understanding family support levels | 8 |
| 9 | Educational level of parents, parents awareness of asthma, children with serious course of the disease | 9 |
| 10 | High score of clinical symptoms of asthma, Forced expiratory volume 1 as a percentage of predicted, airway resistance as a percentage of predicted, vital capacity. The mask is too tight, inhalation time is too long | 10 |
| 11 | Asthma severity (severe), educational level of parents (college and above), parents awareness of asthma (understanding), level of parental trust in healthcare workers (trust) | 10 |
| 12 | The parents of the children have a poor understanding of the knowledge related to nebulization therapy, mental state of the child, atomizing method, Types of atomized drugs, parents distrust of health care workers | 9 |
| 13 | poor family economic conditions, left-behind children, lack of disease knowledge, adverse drug reactions, medical supervision, psychological support | 7 |
Table 2: Influencing Factors and Scores of Included Literature
| Influencing factors | Number of research articles | Heterogeneity test | Model selection | OR | 95 % CI | Combined effect test | |||
|---|---|---|---|---|---|---|---|---|---|
| I2 (%) | Q | p | Z | p | |||||
| General situation | |||||||||
| Lack of asthma knowledge | 7 | 94 | 97.04 | <0.0001 | Random | 0.75 | (0.24~2.30) | 0.51 | 0.61 |
| Degree of illness | 4 | 0 | 1.65 | 0.65 | Fixed | 0.31 | (0.22~0.43) | 7.04 | <0.0001 |
| Bad psychology | 4 | 89 | 27.23 | <0.0001 | Random | 1.28 | (0.31~5.30) | 0.34 | 0.73 |
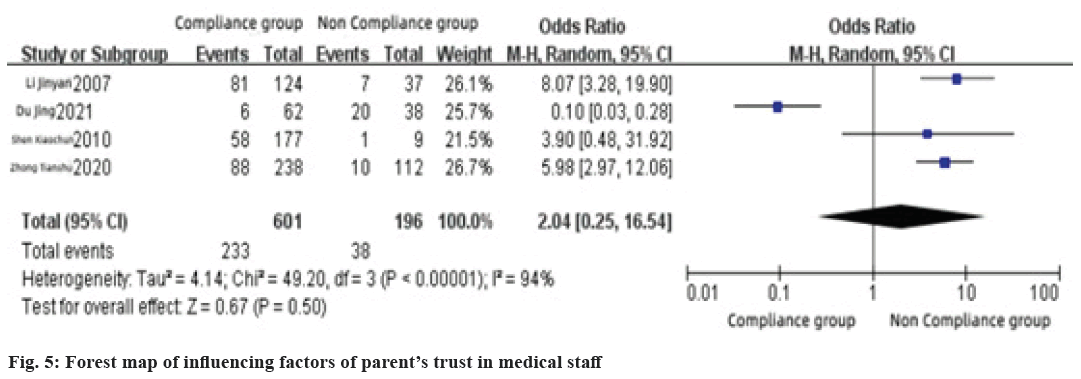
| Parents' trust in medical staff | 4 | 94 | 49.2 | <0.0001 | Random | 2.04 | (0.25~16.54) | 0.67 | 0.5 |
Table 3: Meta analysis of Influencing Factors of Medication Compliance in Childhood Asthma
This factor included 7 literatures and the results showed that there was heterogeneity among the literatures (I2=94 %, p<0.1), so adopted the random effect model, the results of meta-analysis showed that the lack of asthma knowledge had no significant effect on medication compliance of childhood asthma medication (Z=0.51, p>0.1), the combined OR value was 0.75 % and 95 % CI (0.24~2.30), as shown in fig. 2.
This factor included in 4 literatures. The results showed that there was heterogeneity among the literatures (I2=0 %, p>0.1), so adopted the fixed effect model, meta-analysis results showed that the degree of disease had a statistically significant effect on medication compliance of childhood asthma medication (Z=7.04, p<0.1), the combined OR value was 0.31, 95 % CI (0.22~0.43), as shown in fig. 3.
This factor included in 4 literatures. The results showed that there was heterogeneity among the literatures (I2=89 %, p<0.1), so adopted the random effect model, the results of meta-analysis showed that adverse psychological reactions had no significant effect on medication compliance of childhood asthma (Z=0.34, p>0.1), the combined OR value was 1.28, 95 % CI (0.31~5.30), as shown in fig. 4.
This factor included in 4 literatures. The results showed that the heterogeneity among the literatures (I2=94 %, p<0.1), so adopted the random effect model, meta-analysis results showed that parent’s trust in medical staff had no significant effect on childhood asthma medication compliance (Z=0.67, p>0.1), the combined OR value was 2.04, 95 % CI (0.25~16.54), as shown in fig. 5.
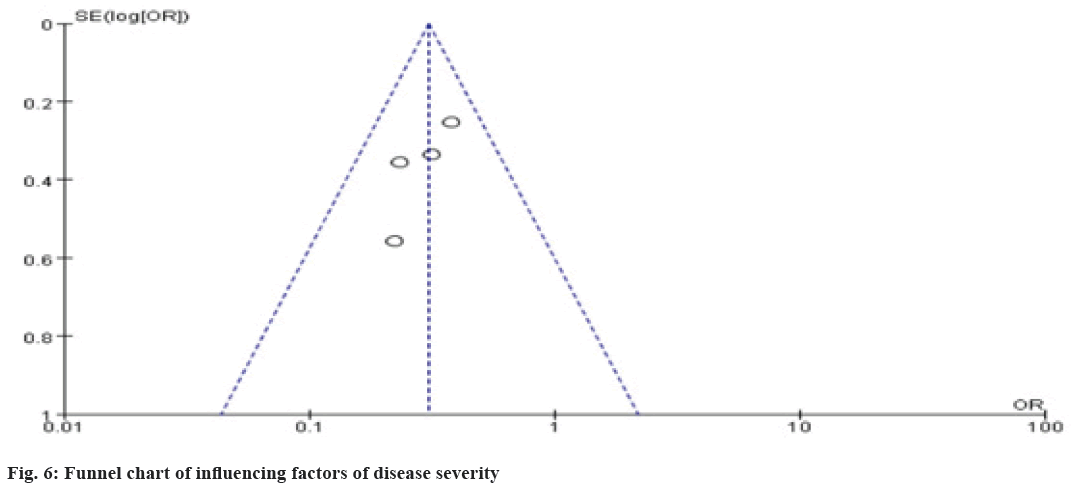
In this study, funnel plots were used to analyze publication bias. In the test of funnel plots, the reliability of the test was limited due to the limited number of literatures included in the research factors. Taking the factors with statistically significant differences in the combined effect as the research object, the funnel plot of the difference in treatment adherence caused by the severity of the disease is basically symmetrical, indicating that the bias is small as shown in fig. 6.
A study on children showed that the asthma medication compliance of children reached 86.9 % within 1 to 3 mo, decreased to 65.0 % at 4 to 6 mo and continued to drop to 52.5 % at 7 to 12 mo, indicates that children’s asthma medication compliance is poor and decreases with treatment time[21]. Previous studies have shown that children’s age, parent’s educational level, parent’s awareness of asthma, children’s serious illness, adverse psychological reactions, lack of awareness of inhaled hormones, general doctor-patient relationship, parent’s knowledge of nebulization therapy, adverse drug reactions, economic factors such as status can affect patient compliance, but in this meta-analysis, only the severity of the disease was shown to be the main factor leading to reduced medication compliance for childhood asthma.
According to previous research reports, carrying out health education is of great significance for consolidating the curative effect, delaying the disease and improving medication compliance. Health education is to make patients and relatives understand the whole process of the occurrence, development, treatment and prevention of diseases through planned, organized, systematic and evaluated educational activities, and to promote people to establish and form healthy lifestyles and behaviors. Therefore, by carrying out health education, explaining the cause of the disease in detail for children, improving the cognitive ability of the disease and improving the self-management ability of the children, the treatment behavior of the child can be changed from passive to active, so as to consolidate the curative effect and delay the disease aggravating effect[22].
In view of the current situation of reduced medication compliance for childhood asthma, nurses should closely monitor the condition of children on the basis of routine care, provide children with active psychological counseling and encourage them to actively receive treatment. In general, the more severe the disease, the more types of drugs the patient needs to use, resulting in a relatively weakened self-management ability of the child. Therefore, in addition to providing medication guidance to children and their families, helping them to master the treatment measures for adverse drug reactions, as well as remedial measures for not taking medicines on time or missing medicines. Nursing staff should also train parents on environmental knowledge, dietary care and child behavior. First, ensure that the living environment of the children is clean and tidy, prohibit pets and regularly clean and sterilize the living environment. Secondly, provide dietary care to the children, instructing children that their daily diet should be light, avoid spicy and greasy, balanced nutrition, avoid ingesting allergy-causing foods and drugs, and finally urge children to establish a regular schedule and develop a good life habits, proper exercise, improve their immunity[23], it is beneficial to avoid further aggravation of asthma in children and to improve medication compliance.
In summary, the degree of illness is the main factor affecting the poor medication compliance of childhood asthma. Therefore, clinical medical staff should strengthen the intervention behavior of health education for children and their parents, explain the importance of insisting on taking medicines and consolidating the curative effect to children and their parents, and at the same time correctly guide parents to treat children’s adverse drug reactions and encourage healthy life in order to achieve the purpose of improving medication compliance and controlling the occurrence of asthma. This study is the first time to conduct a meta-analysis on the influencing factors of drug treatment for childhood asthma. Due to the lack of included literature, the classification criteria of some influencing factors are not uniform, especially the literature related to some factors is less and the research results have certain limitations, further detailed research is required.
Conflict of interests:
The authors declared no conflict of interests.
References
- Yan M, Ai T, Chen HJ. Advances of mechanism of mesenchymal stem cells in animal experiments with bronchial asthma. Chin J Appl Clin Pediatr 2022;37(2):150-2.
- Liu CH, Li S, Shao MJ. Characteristics of lung function changes in children with bronchial asthma. Chin J Pract Pediatr 2021;36(6):412-6.
- Ferraro V, Carraro S, Bozzetto S, Zanconato S, Baraldi E. Exhaled biomarkers in childhood asthma: Old and new approaches. Asthma Res Pract 2018;4(1):9.
[Crossref] [Google Scholar] [Pub Med]
- Wang F, Gong JJ, Wang XM. Adherence to and influencing factors of inhaled corticosteroids for childhood asthma. Chin J Reprod Health 2015;6:501-7
- Qi KW, Zheng WS, Li MH. Clinical observation of Bailing capsule combined with inhaled glucocorticoid in the treatment of children with bronchial asthma. Shandong Med J 2021;61(4):76-9.
- Zhai C, Song Y, Su XF. Determinants of treatment compliance for inhaled glucocorticoids in asthma patients. Chin J Lung Dis 2020;13(3):302-6.
- Qin HT, Wang W, Lin N. Analysis on parents factors of influencing compliance of asthma children for inhalation therapy. Chin Nurs Res 2013;27(17):1699-700.
- Li JY, Zhang W. Study on correlation factor of inhalation compliance on ped-patient with asthma. Mod J Integr Tradit Chin Western Med 2007;16(33):4927-8.
- Shen XC. Investigation on the compliance of inhaled glucocorticoid therapy in children with bronchial asthma in Meizhou City. Jinan University; 2010.
- Yang YZ. Analysis of related factors affecting children's bronchial asthma treatment compliance. J Clin Exp Med 2012;11(5):384-5.
- He S. Influencing factors and nursing countermeasures of children's bronchial asthma treatment compliance. Chin J Mod Nur 2012;18(19):2303-5.
- You Z. Factors and countermeasures affecting the compliance of inhaled hormone therapy in children with asthma. Chin J Med Guide 2013;15(5):796-8.
- Luo QR. Factors and countermeasures affecting the compliance of inhaled hormone therapy in children with asthma. Lab Med Clin 2013;10(12):1550-2.
- Zhang N. Construction and effect evaluation of comprehensive management model for children with asthma. Shandong: Qingdao University; 2015.
- Zhang Y. Study on medication compliance and its influencing factors in children with long-term oral glucocorticoids. Beijing Union Medical College, China; 2017.
- Liang ML, Wu MJ, Wang W. Analysis of compliance with inhaled glucocorticoid therapy and nursing intervention in children with asthma. Int J Nurs 2018;37(6):803-6.
- Hu ST, Lei SQ, Li XH. Analysis of factors influencing the treatment compliance of inhaled glucocorticoid in children patients with bronchial asthma. Nurs Pract Res 2019;16(18):10-2.
- Zhong TS, Jiang Y, Ou Y. Evaluation in application and medication compliance of inhaled corticosteroids for children with asthma. J Clin Pulm Med 2020;25(5):697-701.
- Du J, Liang J. Compliance and influencing factors analysis of nebulizer therapy in asthma children with acute stage. Chin Med Herald 2021;18(12):131-4.
- Wang YY, Zhou LZ, Zhang LZ. Analysis of influencing factors on treatment compliance of children with bronchial asthma. Mater Child Health Care Chin 2021;36(4):878-80.
- Yu YC, Jia LL, Hu LH. Investigation on compliance to inhaled corticosteroids in children with asthma in remission stage. Chin J Hosp Pharm 2019;39(14):1494-8.
- Li QX, Zhang YL, Li H. Comparison of the effect of health education on schizophrenia patients with different course of disease. J Nurs 2009;16(6):76-7.
- Ma R. Parent’s meticulous training impact on quality of life in children with asthma. Nurs Pract Res 2015;12(12):73-4.